Summary
The following chapter is a contemporary overview of the management of patients with unprotected left main coronary artery disease. A background of the anatomy and pathophysiology of the left main stem is given, followed by the appropriate selection of patients electing to undergo either surgical or percutaneous revascularisation based on contemporary clinical evidence, established and new/emerging decision-making tools and international guidelines. Contemporary clinical issues in undertaking unprotected left main revascularisation are also discussed. Principles of adjunctive intravascular imaging and tools such as intravascular ultrasound, optical coherence tomography and physiological assessments of lesions – either invasively (pressure wire assessment) or non-invasively (HeartFlowTM technology applied to computed tomography angiography) – and how this influences distal left main bifurcation management. To conclude a dedicated practical based section involving ‘tips and tricks’ in undertaking left main percutaneous coronary intervention, is detailed.
Introduction
Significant unprotected left main coronary artery (ULMCA) disease occurs in 5-7% of patients undergoing coronary angiography [11. Stone P, Goldschlager N. Left main coronary artery disease: review and appraisal. Cardiovasc Med. 1979;4:165 – 177. , 22. DeMots H, Rosch J, McAnulty J. Left main coronary artery disease. Cardiovasc Clin. 1977;8:201 – 211. ]. The left main stem (LMS) is of particular importance as it supplies 84% of the blood flow to the left ventricle (LV) in a right dominant system (with 16% supplied by the right coronary artery [RCA]) and 100% of the blood flow to the LV in a left dominant system [33. Sianos G, Morel MA, A.P. K, Morice MC, Colombo A, Dawkins K, van den Brand M, Dyck NV, Russell ME, Mohr FW, Serruys PW. (2005 ) The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-27. The birth of the SYNTAX Score. , 44. Leaman DM, Brower RW, Meester GT, Serruys P, van den Brand M. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation. 1981;63:285-99. ]. Consequently, severe LMS disease and its association with multivessel disease potentially exposes patients to a high risk of life-threatening cardiovascular events secondary to a large territory of jeopardised myocardium. Moreover, there is accumulating evidence that clinical outcomes in patients with ULMCA disease are significantly influenced by the increasing prevalence of multivessel disease and its apparent association with clinical comorbidity and systemic atherosclerotic disease, [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. , 77. Park DW, Kim YH, Yun SC, Song HG, Ahn JM, Oh JH, Kim WJ, Lee JY, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug-eluting stents or coronary artery bypass grafting. J Am Coll Cardiol. 2011;57:2152-9.
High quality registry information associating coronary artery disease complexity (as defined by the SXscore) in patients undergoing ULM PCI to long term (5 year) clinical outcomes. Currently subject to the ongoing EXCEL trial., 88. Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Lee AJ, Price JF, d’Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodriguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197-208. , 99. Otah KE, Madan A, Otah E, Badero O, Clark LT, Salifu MO. Usefulness of an abnormal ankle-brachial index to predict presence of coronary artery disease in African-Americans. Am J Cardiol. 2004;93:481-3. , 1010. Sukhija R, Aronow WS, Yalamanchili K, Peterson SJ, Frishman WH, Babu S. Association of ankle-brachial index with severity of angiographic coronary artery disease in patients with peripheral arterial disease and coronary artery disease. Cardiology. 2005;103:158-60. , 1111. Igarashi Y, Chikamori T, Tomiyama H, Usui Y, Hida S, Tanaka H, Harafuji K, Yamashina A. Diagnostic value of simultaneous brachial and ankle blood pressure measurements for the extent and severity of coronary artery disease as assessed by myocardial perfusion imaging. Circulation. 2005;69:237-42. , 1212. Papamichael CM, Lekakis JP, Stamatelopoulos KS, Papaioannou TG, Alevizaki MK, Cimponeriu AT, Kanakakis JE, Papapanagiotou A, Kalofoutis AT, Stamatelopoulos SF. Ankle-brachial index as a predictor of the extent of coronary atherosclerosis and cardiovascular events in patients with coronary artery disease. Am J Cardiol. 2000;86:615-8. , 1313. Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262-9. , 1414. Adams MR, Nakagomi A, Keech A, Robinson J, McCredie R, Bailey BP, Freedman SB, Celermajer DS. Carotid intima-media thickness is only weakly correlated with the extent and severity of coronary artery disease. Circulation. 1995;92:2127-34. , 1515. Steinvil A, Sadeh B, Arbel Y, Justo D, Belei A, Borenstein N, Banai S, Halkin A. Prevalence and predictors of concomitant carotid and coronary artery atherosclerotic disease. J Am Coll Cardiol. 2011;57:779-83. , 1616. Ikeda N, Kogame N, Iijima R, Nakamura M, Sugi K. Carotid artery intima-media thickness and plaque score can predict the SYNTAX score. Eur Heart J. 2012 Jan;33:113-9. Epub 2011 Oct 25. , 1717. Korkmaz L, Bektas H, Korkmaz AA, Agac MT, Acar Z, Erkan H, Celik S. Increased Carotid Intima-Media Thickness is Associated With Higher SYNTAX Score. Angiology. 2011 Sep 22. [Epub ahead of print]. , 1818. Okwuosa TM, Greenland P, Ning H, Liu K, Bild DE, Burke GL, Eng J, Lloyd-Jones DM. Distribution of Coronary Artery Calcium Scores by Framingham 10-Year Risk Strata in the MESA (Multi-Ethnic Study of Atherosclerosis) Potential Implications for Coronary Risk Assessment. J Am Coll Cardiol. 2011;57:1838-45. , 1919. Farooq V, Brugaletta S, Serruys PW. Contemporary and evolving risk scoring algorithms for percutaneous coronary intervention. Heart. 2011;97:1902-13. ] factors which further add to the decision-making processes in determining the optimal revascularisation modality. This is discussed in detail in the clinical tools section of this chapter.
Patients with ULMCA disease treated medically have historically been reported to have a three-year mortality rate of 50% [2020. Taylor H, Deumite N, Chaitman B, Davis K, Killip J, Rogers W. Asymptomatic left main coronary artery disease in the Coronary Artery Surgery Study (CASS) registry. Circulation. 1989;79:1171–1179. , 2121. Cohen M, Gorlin R. Main left coronary artery disease: clinical experience from 1964 – 1974. Circulation. 1975;52:275 – 285. ]. Multiple studies have demonstrated a significant mortality benefit following treatment of LMS disease with coronary artery bypass grafting (CABG) compared to medical treatment [2222. Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563-70. , 2323. Chaitman BR, Fisher LD, Bourassa MG, Davis K, Rogers WJ, Maynard C, Tyras DH, Berger RL, Judkins MP, Ringqvist I, Mock MB, Killip T. Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am J Cardiol. 1981;48:765-77. , 2424. Takaro T, Peduzzi P, Detre KM, Hultgren HN, Murphy ML, van der Bel-Kahn J, Thomsen J, Meadows WR. Survival in subgroups of patients with left main coronary artery disease. Veterans Administration Cooperative Study of Surgery for Coronary Arterial Occlusive Disease. Circulation. 1982;66:14-22. , 2525. Caracciolo EA, Davis KB, Sopko G, Kaiser GC, Corley SD, Schaff H, Taylor HA, Chaitman BR. Comparison of surgical and medical group survival in patients with left main equivalent coronary artery disease. Long-term CASS experience. Circulation. 1995;91:2335-44. , 2626. Caracciolo EA, Davis KB, Sopko G, Kaiser GC, Corley SD, Schaff H, Taylor HA, Chaitman BR. Comparison of surgical and medical group survival in patients with left main coronary artery disease. Long-term CASS experience. Circulation. 1995;91:2325-34. ]. Although CABG has historically been regarded as the gold standard treatment for LMS disease, recent studies focusing on the safety and efficacy of PCI for ULMCA – which have incorporated important advances in percutaneous coronary intervention (PCI) techniques, stent technology and adjunctive pharmacotherapy – have allowed for the re-evaluation of the role of PCI in ULMCA disease [77. Park DW, Kim YH, Yun SC, Song HG, Ahn JM, Oh JH, Kim WJ, Lee JY, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug-eluting stents or coronary artery bypass grafting. J Am Coll Cardiol. 2011;57:2152-9.
High quality registry information associating coronary artery disease complexity (as defined by the SXscore) in patients undergoing ULM PCI to long term (5 year) clinical outcomes. Currently subject to the ongoing EXCEL trial., 2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. , 2929. Ferrante G, Presbitero P, Valgimigli M, Morice MC, Pagnotta P, Belli G, Corrada E, Onuma Y, Barlis P, Locca D, Eeckhout E, Di Mario C, Serruys PW. Percutaneous coronary intervention versus bypass surgery for left main coronary artery disease: a meta-analysis of randomised trials. EuroIntervention. 2011;7:738-46.
One of the first meta-analyses of randomised trials supporting the EXCEL hypothesis., 3030. Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, Lee JY, Kim WJ, Kang SJ, Lee SW, Lee CW, Park SW, Chung CH, Lee JW, Lim DS, Rha SW, Lee SG, Gwon HC, Kim HS, Chae IH, Jang Y, Jeong MH, Tahk SJ, Seung KB. Randomised trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364:1718-27. ]. For instance, nowadays if a patient has low coronary anatomy complexity, PCI has the same recommendation as CABG for treatment of ULMCA.
Despite previous guidelines’ recommendation of CABG as the standard procedure for ULMCA disease [3131. Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D, Vahanian A, Auricchio A, Bax J, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearney P, McDonagh T, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas PE, Widimsky P, Alfieri O, Dunning J, Elia S, Kappetein P, Lockowandt U, Sarris G, Vouhe P, von Segesser L, Agewall S, Aladashvili A, Alexopoulos D, Antunes MJ, Atalar E, Brutel de la Riviere A, Doganov A, Eha J, Fajadet J, Ferreira R, Garot J, Halcox J, Hasin Y, Janssens S, Kervinen K, Laufer G, Legrand V, Nashef SA, Neumann FJ, Niemela K, Nihoyannopoulos P, Noc M, Piek JJ, Pirk J, Rozenman Y, Sabate M, Starc R, Thielmann M, Wheatley DJ, Windecker S, Zembala M. Guidelines on myocardial Revascularisation: The Task Force on Myocardial Revascularisation of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501-55.
European Revascularisation Guidelines – an essential read!, 3232. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
2011 American Revascularisation Guidelines – a further essential read! Notably the recommendations to support ULM PCI in selected patients was increased from Class IIB in the 2009 guidelines to Class IIA in the present guidelines.], the most recent have already identified the suitability of ULMCA PCI in patients with low anatomical complexity of the coronary arteries [286286. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019 ;40:87-165. ]. The following questions are therefore raised. What is the optimal revascularisation modality for patients with ULMCA disease? Would clinical presentation alter the decision-making processes? If ULM PCI is to be undertaken how can I best undertake this and subsequently manage my patient longer term based on the best available clinical evidence? What about the future?
Introduction
- Significant unprotected left main coronary artery (ULMCA) disease occurs in 5-7% of patients undergoing coronary angiography
- Patients with ULMCA disease treated medically have been reported to have a three-year mortality rate of 50%
- CABG has historically been regarded as the gold standard treatment for ULMCA disease
- Important advances in percutaneous coronary intervention (PCI) techniques, stent technology and adjunctive pharmacotherapy have allowed for the re-evaluation of the role of PCI in ULMCA disease with current practice guidelines giving the same recommendation as CABG for patients with low coronary artery anatomy complexity and giving support for the consideration of unprotected left main percutaneous coronary intervention (ULM PCI) in patients with intermediate anatomy complexity.
Anatomy and pathophysiology of left main disease
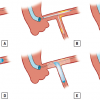
The LMS refers to the proximal segment of the left coronary artery that arises from the left aortic sinus, just below the sinotubular junction, to its bifurcation into the left anterior descending (LAD) and left circumflex (LCx) arteries. In approximately two thirds of patients, the LMS bifurcates into the LAD and LCx arteries; in one third of patients the LMS trifurcates into the LAD, LCx, and ramus intermedius [3333. Reig J, Petit M. Main trunk of the left coronary artery: anatomic study of the parameters of clinical interest. Clinical anatomy. 2004;17:6-13. , 3434. Park SJ, Park DW. Percutaneous coronary intervention with stent implantation versus coronary artery bypass surgery for treatment of left main coronary artery disease: is it time to change guidelines? Circ Cardiovasc Interv. 2009;2:59-68. ]. The LMS is generally divided into three anatomical regions: the ostium or origin of the LMS from the aorta, a mid-portion, and the distal portion. The LMS differs from other coronary arteries due its relatively greater elastic tissue content, particularly in the ostium – historically this may explain the elastic recoil and high restenosis rates observed following balloon angioplasty [3535. Macaya C, Alfonso F, Iniguez A, Goicolea J, Hernandez R, Zarco P. Stenting for elastic recoil during coronary angioplasty of the left main coronary artery. Am J Cardiol. 1992;70:105-7. ]. The segment of the LMS which extends beyond the aorta displays the same layered architecture as that of other coronary arteries.
Examination of 100 autopsy cases has demonstrated that the LMS has an average length of 10.8±5.2 mm (range 2 to 23 mm), an average diameter of 4.9±0.8 mm, and an average angle of the terminal branch division of 86.7±28.8° (range 40° to 165°), and that there is a positive correlation between LMS length and the angle between the terminal branches, with the longest LMS having the largest angle of division [3333. Reig J, Petit M. Main trunk of the left coronary artery: anatomic study of the parameters of clinical interest. Clinical anatomy. 2004;17:6-13. , 3636. Farinha JB, Kaplan MA, Harris CN, Dunne EF, Carlish RA, Kay JH, Brooks S. Disease of the left main coronary artery. Surgical treatment and long-term follow up in 267 patients. Am J Cardiol. 1978;42:124-8. ].
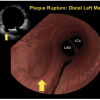
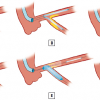
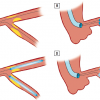
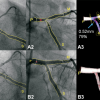
Furthermore, in a substudy of the SYNTAX trial utilising 3-dimensional quantitative coronary angiography (QCA), Girasis et al demonstrated a large variation in the angulation parameters of the LMS (proximal and distal bifurcation angles with mean pre-PCI end-diastolic values of 105.9 ± 21.7° and 95.6 ± 23.6° respectively). In particular, systolic motion was shown to result in a reduction of the distal (-8.2°) and an enlargement of the proximal (+8.5°) bifurcation angle ( Figure 1 ), and that subsequent PCI modified the distal bifurcation angle [3737. Girasis C, Serruys PW, Onuma Y, Colombo A, Holmes DR, Jr., Feldman TE, Bass EJ, Leadley K, Dawkins KD, Morice MC. 3-Dimensional bifurcation angle analysis in patients with left main disease: a substudy of the SYNTAX trial (SYNergy Between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery). JACC Cardiovasc Interv. 2010;3:41-8. ]. The incidence of MACCE at 12 months, however, did not differ across pre-PCI distal bifurcation angle values. Final 5-year reporting of the SYNTAX Trial demonstrated a restricted post-procedural systolic-diastolic distal bifurcation angle range to be associated with a higher 5-year adverse event rates after LMCA bifurcation PCI ( Figure e1 ). Namely, patients with post-PCI systolic-diastolic range <10° had a significantly higher MACCE (50.8% vs. 22.7%, p < 0.001) and repeat revascularization (37.4% vs. 15.5%, p = 0.002). In addition, post-PCI systolic-diastolic range <10° was shown to be an independent predictor of MACCE (hazard ratio: 2.65; 95% confidence interval: 1.55 to 4.52; p < 0.001). Conversely, the pre-PCI bifurcation angle value was shown not to affect clinical outcomes. [247247. Girasis C, Farooq V, Diletti R, Muramatsu T, Bourantas CV, Onuma Y, Holmes DR, Feldman TE, Morel MA, van Es GA, Dawkins KD, Morice MC, Serruys PW. Impact of 3-dimensional bifurcation angle on 5-year outcome of patients after percutaneous coronary intervention for left main coronary artery disease: a substudy of the SYNTAX trial (synergy between percutaneous coronary intervention with taxus and cardiac surgery). JACC Cardiovasc Interv. 2013;6:1250-60 ]. Confirmation of these findings are awaited from other randomised trials.
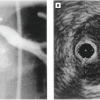
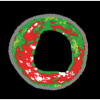
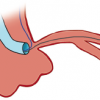
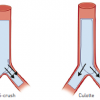
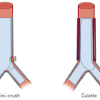
The atherosclerotic involvement of the LMS has previously been associated with its histology and flow haemodynamics [3838. Nakazawa G, Yazdani SK, Finn AV, Vorpahl M, Kolodgie FD, Virmani R. Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55:1679-87. ]. In the LMS, bifurcation intimal atherosclerosis is accelerated primarily in areas of low shear stress in the lateral walls (i.e., opposite the flow divider – carina) close to the LAD and LCx bifurcation ( Figure 2 ). Conversely, the bifurcation carina is frequently free of disease due to its being a high shear stress area. Furthermore, previous intravascular ultrasound (IVUS) studies have given further important insights into the distribution of plaque in the LMS [3939. Oviedo C, Maehara A, Mintz GS, Araki H, Choi SY, Tsujita K, Kubo T, Doi H, Templin B, Lansky AJ, Dangas G, Leon MB, Mehran R, Tahk SJ, Stone GW, Ochiai M, Moses JW. Intravascular ultrasound classification of plaque distribution in left main coronary artery bifurcations: where is the plaque really located? Circ Cardiovasc Interv. 2010;3:105-12.
Plaque distribution at the left main - an essential read!, 4040. Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, Waksman R, Laird JR, Jr., Suddath WO, Kent KM, Weissman NJ. Intravascular ultrasound assessment of the stenoses location and morphology in the left main coronary artery in relation to anatomic left main length. Am J Cardiol. 2001;88:1-4. ]. Oviedo et al demonstrated that bifurcation disease was rarely focal and that both sides of the flow divider (carina) were always disease-free [3939. Oviedo C, Maehara A, Mintz GS, Araki H, Choi SY, Tsujita K, Kubo T, Doi H, Templin B, Lansky AJ, Dangas G, Leon MB, Mehran R, Tahk SJ, Stone GW, Ochiai M, Moses JW. Intravascular ultrasound classification of plaque distribution in left main coronary artery bifurcations: where is the plaque really located? Circ Cardiovasc Interv. 2010;3:105-12.
Plaque distribution at the left main - an essential read!]. In addition continuous plaque from the LMS into the proximal LAD artery was seen in 90% of cases undergoing IVUS and that the plaque disease tended to be diffuse. Based on these findings of longitudinal and circumferential spatial plaque distribution, an IVUS classification system for bifurcation lesions was proposed ( Figure 3 and Figure 4 and Figure 5 ). Maehara et al [4040. Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, Waksman R, Laird JR, Jr., Suddath WO, Kent KM, Weissman NJ. Intravascular ultrasound assessment of the stenoses location and morphology in the left main coronary artery in relation to anatomic left main length. Am J Cardiol. 2001;88:1-4. ] demonstrated that short LMS (<10 mm) developed stenoses more frequently near the ostium compared to near the distal bifurcation (55% versus 38%), that long LMS developed stenoses more frequently near the distal bifurcation compared to near the ostium (77% versus 18%), and that the mid-portion of the LMS was infrequently stenosed (5-7% of patients). Furthermore, ostial LMS stenoses were more common in women (44% versus 20%), and were associated with larger lumen areas, less calcification, and more negative remodelling compared to mid or distal-bifurcation LMCA stenoses.
Anatomy and pathophysiology of left main coronary artery disease
- The LMS is generally divided into three anatomical regions: the ostium (arising from the left aortic sinus), a mid and a distal portion
- The distal portion of the LMS bifurcates into the LAD and LCx arteries in approximately two thirds of patients, and trifurcates into the LAD, LCx, and ramus intermedius in approximately one third of patients
- The greater elastic tissue content in the LMS (particularly the ostium) may historically explain the elastic recoil and greater restenosis rates observed following balloon angioplasty
- Intimal atherosclerosis is accelerated in low shear stress areas in the lateral walls of the LMS (i.e., opposite the flow divider – carina) close to the LAD and LCx bifurcation; conversely the carina is frequently free of disease due to its being a high shear stress area
- IVUS studies have shown that plaque burden in the LMS bifurcation is more frequently diffuse rather than focal, with continuous plaque from the LMS into the proximal LAD artery occurring in approximately 90% of cases
Review of global evidence for unprotected left main intervention
Within the last 10 to 15 years a large body of evidence has accumulated from registries and randomised trials supporting the feasibility, efficacy and safety of PCI for ULMCA disease in appropriately selected patients.
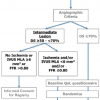
The international multicentre randomised EXCEL (Evaluation of XIENCE Prime versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularisation) trial was awaited because it could ultimately answer the question of the most appropriate revascularisation modality for patients with ULMCA disease [287287. Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, Kandzari DE, Morice MC, Lembo N, Brown WM 3rd, Taggart DP, Banning A, Merkely B, Horkay F, Boonstra PW, van Boven AJ, Ungi I, Bogáts G, Mansour S, Noiseux N, Sabaté M, Pomar J, Hickey M, Gershlick A, Buszman P, Bochenek A, Schampaert E, Pagé P, Dressler O, Kosmidou I, Mehran R, Pocock SJ, Kappetein AP; EXCEL Trial Investigators. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med. 2016;375::2223-2235. ]. EXCEL adopted an enrolment criteria of subjects with ULMCA disease up to intermediate anatomical complexity (SYNTAX Score <33) with minimal exclusion criteria ( Table e1 ) to allow meaningful comparisons between revascularisation modalities (Xience Everolimus-Eluting Stent vs. Coronary Artery Bypass Surgery) and enrolled 1905 subjects in 131 centres.
The primary endpoint analysis was conducted at a median follow-up of 3 years AND after all patients have reached the 2-year follow-up. To facilitate a more reliable ascertainment of the primary end point, an additional follow-up visit was performed when the last randomly assigned patients reached 2-year follow-up.
The trial was designed to determine if PCI was non-inferior to surgery in patients with ULMCA disease and low or intermediate SYNTAX score. The primary endpoint was a composite of all-cause death, any stroke or myocardial infarction.
In Kaplan–Meier analyses, the primary end point occurred at a similar rate in the PCI and CABG surgery groups (15.4% versus 14.7%; p=0.02 for non-inferiority; p=0.98 for superiority). In a landmark analysis at 30 days, PCI was superior to CABG surgery, showing a lower incidence of peri-procedural myocardial infarction using a clinically relevant definition. Use of PCI also resulted in less peri-procedural non-ischaemic events (bleeding, infection and renal failure). The final follow-up results of 5-years of EXCEL is awaited and will be presented in 2019.
Another recent randomised trial assessing the outcomes of PCI versus CABG in patients with ULMCA was the Nordic-Baltic-British left main revascularisation study (NOBLE) [288288. Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, Trovik T, Eskola M, Romppanen H, Kellerth T, Ravkilde J, Jensen LO, Kalinauskas G, Linder RB, Pentikainen M, Hervold A, Banning A, Zaman A, Cotton J, Eriksen E, Margus S, Sorensen HT, Nielsen PH, Niemela M, Kervinen K, Lassen JF, Maeng M, Oldroyd K, Berg G, Walsh SJ, Hanratty CG, Kumsars I, Stradins P, Steigen TK, Frobert O, Graham AN, Endresen PC, Corbascio M, Kajander O, Trivedi U, Hartikainen J, Anttila V, Hildick-Smith D, Thuesen L, Christiansen EH, investigators Ns. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388:2743-2752. ]. This trial included 1,201 patients randomised to either PCI with a DES (Biolimus- or Sirolimus- eluting stent) or to CABG. The primary endpoint in this trial was a non-inferiority comparison of PCI versus CABG with regards to MACCE at 5 years of follow-up. MACCE rates were significantly higher with PCI compared with CABG surgery (29% vs. 19%; p=0.0066), and the non-inferiority hypothesis was not met. Mortality was comparable in both revascularisation strategies, but CABG surgery was associated with significant reductions in non-procedural myocardial infarction, stroke, and repeat revascularisation. Procedural myocardial infarction was not assessed in this trial, and the stent thrombosis rate was substantially higher than in the EXCEL trial. This significant difference in stent thrombosis might probably reflect the distinguish stent types used in each trial. In addition, an inexplicably high rate of late stroke in the PCI group contributed to the increased risk of MACCE associated with this procedure [288288. Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, Trovik T, Eskola M, Romppanen H, Kellerth T, Ravkilde J, Jensen LO, Kalinauskas G, Linder RB, Pentikainen M, Hervold A, Banning A, Zaman A, Cotton J, Eriksen E, Margus S, Sorensen HT, Nielsen PH, Niemela M, Kervinen K, Lassen JF, Maeng M, Oldroyd K, Berg G, Walsh SJ, Hanratty CG, Kumsars I, Stradins P, Steigen TK, Frobert O, Graham AN, Endresen PC, Corbascio M, Kajander O, Trivedi U, Hartikainen J, Anttila V, Hildick-Smith D, Thuesen L, Christiansen EH, investigators Ns. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388:2743-2752. ].
The different coronary anatomy complexity in both trials (higher in NOBLE, as assessed by the SYNTAX score), the different stent platform and the longer follow-up in NOBLE, altogether might explain worse outcomes in NOBLE. The 5-years follow-up of EXCEL will clarify some of these questions.
In the interim, details of the meta-analyses to best explain the expanding literature are discussed below. Indications of PCI in other patient types are further detailed. In the next section, clinical tools associated with ULMCA disease, including the SYNTAX Score, are discussed, followed by indications of revascularisation in patients presenting with acute coronary syndrome together with other contemporary clinical issues in undertaking ULM revascularisation. To conclude this section, a summary of current international guidelines are given.
GLOBAL EVIDENCE
Unprotected left main PCI with bare metal stents
To date, no randomised controlled trials have been performed using bare metal stents (BMS) in ULM PCI. The longest follow-up available in the literature is from the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularisation) Registry (n=250: BMS n=100, CABG n=250) [4141. Alam M, Virani SS, Deswal A, Huang HD, Paniagua D, Kar B, Bozkurt B, Jneid H. Abstract 19671: Percutaneous Coronary Interventions with Drug-Eluting Stents for Unprotected Left Main Coronary Artery Stenosis are Associated with Reduced Stroke and Increased Repeat Revascularisation Risk Compared with Coronary Artery Bypass Graft Surgery: Results from a Contemporary Aggregate Data Meta-Analysis. Circulation. 2010; 122: A19671. ]. In the 10-year follow-up, the adjusted risks of death (HR 0.81; 95%, CI: 0.44 to 1.50; p=0.50) and the composite outcome of death/QWMI/CVA (HR: 0.92; 95% CI: 0.55 to 1.53; p=0.74) were similar between the 2 treatment groups (BMS and CABG). Notably, the rate of TVR was significantly higher in the BMS group (HR: 10.34; 95% CI: 4.61 to 23.18; p<0.001). For comparison, 5-year follow-up of another population who underwent ULM PCI with DES from the same registry (n=395: DES n=176, CABG n=219) [4141. Alam M, Virani SS, Deswal A, Huang HD, Paniagua D, Kar B, Bozkurt B, Jneid H. Abstract 19671: Percutaneous Coronary Interventions with Drug-Eluting Stents for Unprotected Left Main Coronary Artery Stenosis are Associated with Reduced Stroke and Increased Repeat Revascularisation Risk Compared with Coronary Artery Bypass Graft Surgery: Results from a Contemporary Aggregate Data Meta-Analysis. Circulation. 2010; 122: A19671. ] demonstrated no significant differences in death (HR: 0.83; 95% CI: 0.34 to 2.07; p=0.70) or the same composite outcome of death/QWMI/CVA (HR: 0.91; 95% CI: 0.45 to 1.83; p=0.79). The rate of TVR was, however, higher in the DES group compared to the CABG group (HR: 6.22; 95% CI: 2.26 to 17.14; p<0.001); with the effect being less pronounced compared to BMS.
In addition, Nomura et al [4242. Nomura A, Yamaji K, Shirai S, Soga Y, Nagashima M, Arita T, Ando K, Sakai K, Goya M, Yokoi H, Iwabuchi M, Nobuyoshi M. Very Long term Outcomes after Percutaneous Coronary Intervention with Bare Metal Stents for Unprotected Left Main Coronary Artery Disease. EuroIntervention. 2012 In Press. ] recently demonstrated that the reference diameter of the left main trunk prior to PCI and the SYNTAX Score were both predominant determinants of repeat revascularisation at 10 years following BMS implantation in ULM PCI.
Meta-analyses of all studies investigating unprotected left main PCI with DES
Alam et al (2010) [4141. Alam M, Virani SS, Deswal A, Huang HD, Paniagua D, Kar B, Bozkurt B, Jneid H. Abstract 19671: Percutaneous Coronary Interventions with Drug-Eluting Stents for Unprotected Left Main Coronary Artery Stenosis are Associated with Reduced Stroke and Increased Repeat Revascularisation Risk Compared with Coronary Artery Bypass Graft Surgery: Results from a Contemporary Aggregate Data Meta-Analysis. Circulation. 2010; 122: A19671. ] identified 18 studies enrolling 5,483 patients (3,357 patients underwent CABG and 2,126 patients underwent PCI with DES) with ULMCA disease, and performed a meta-analysis of clinical outcomes. Baseline demographic variables, comorbidities and mean follow-up periods were comparable between both revascularisation modalities. At 12 months, both PCI and CABG were associated with similar risks in terms of death (PCI vs. CABG, OR=0.93; 95% CI, 0.65–1.33), MI (PCI vs. CABG, OR=1.18; 95% CI, 0.59–2.32), MACE (PCI vs. CABG, OR=1.54; 95% CI, 0.82–2.87), and MACCE (PCI vs. CABG, OR=1.35; 95% CI, 0.99–1.84). In addition, PCI had a significantly higher risk of repeat revascularisation (PCI vs. CABG, OR=6.47; 95% CI, 3.86–10.84) and a significantly lower risk of CVA (PCI vs. CABG, OR=0.32; 95% CI, 0.15–0.68) at 1 year.
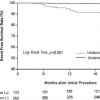
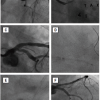
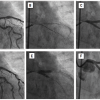
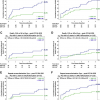
Naik et al (2010) [4343. Naik H, White AJ, Chakravarty T, Forrester J, Fontana G, Kar S, Shah PK, Weiss RE, Makkar R. A meta-analysis of 3, 773 patients treated with percutaneous coronary intervention or surgery for unprotected left main coronary artery stenosis. JACC Cardiovasc Interv. 2009;2:739-47. ] identified 10 studies (8 cohort studies and 2 RCTs), enrolling a total of 3,773 patients, which reported outcomes after PCI and CABG for the treatment of ULMCA disease. Similar incidences of death at 1, 2 and 3 (PCI vs. CABG OR: 1.11 [95% CI: 0.66 to 1.86]) years were evident ( Figure 6 ). Furthermore, the composite of death, MI, and CVA at 1, 2 and 3 (PCI vs. CABG OR: 1.16 [95% CI: 0.68 to 1.98]) years were also similar. TVR was, however, significantly higher in the PCI group at 1 year (OR: 4.36 [95% CI: 2.60 to 7.32]), 2 years (OR: 4.20 [95% CI: 2.21 to 7.97]), and 3 years (OR: 3.30 [95% CI: 0.96 to 11.33]).
Meta-analyses of randomised trials investigating unprotected left main PCI with DES
In the four randomised trials [2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 3030. Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, Lee JY, Kim WJ, Kang SJ, Lee SW, Lee CW, Park SW, Chung CH, Lee JW, Lim DS, Rha SW, Lee SG, Gwon HC, Kim HS, Chae IH, Jang Y, Jeong MH, Tahk SJ, Seung KB. Randomised trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364:1718-27. , 4444. Buszman PE, Kiesz SR, Bochenek A, Peszek-Przybyla E, Szkrobka I, Debinski M, Bialkowska B, Dudek D, Gruszka A, Zurakowski A, Milewski K, Wilczynski M, Rzeszutko L, Buszman P, Szymszal J, Martin JL, Tendera M. Acute and late outcomes of unprotected left main stenting in comparison with surgical Revascularisation. J Am Coll Cardiol. 2008;51:538-45. , 4545. Boudriot E, Thiele H, Walther T, Liebetrau C, Boeckstegers P, Pohl T, Reichart B, Mudra H, Beier F, Gansera B, Neumann FJ, Gick M, Zietak T, Desch S, Schuler G, Mohr FW. Randomised comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol. 2011;57:538-45. ] - enrolling 1, 611 patients - comparing PCI to CABG for the treatment of ULMCA disease, Ferrante et al [2929. Ferrante G, Presbitero P, Valgimigli M, Morice MC, Pagnotta P, Belli G, Corrada E, Onuma Y, Barlis P, Locca D, Eeckhout E, Di Mario C, Serruys PW. Percutaneous coronary intervention versus bypass surgery for left main coronary artery disease: a meta-analysis of randomised trials. EuroIntervention. 2011;7:738-46.
One of the first meta-analyses of randomised trials supporting the EXCEL hypothesis.] demonstrated similar incidences of 1-year mortality (PCI: 2.97%, CABG: 4.06%, OR 0.72, 95% CI [0.42 to 1.24], p=0.23), MI (PCI: 2.85%, CABG: 2.91%, OR 0.97, 95% CI [0.54 to 1.74], p=0.91), and MACCE (14.49% vs. 12.04%, OR 1.24, 95% CI [0.93 to 1.67], p=0.15). A significantly lower risk of CVA (PCI: 0.12%, CABG: 1.90%, OR 0.14, 95% CI [0.04 to 0.55], p=0.004) and a higher risk of TVR (PCI: 11.03%, CABG: 5.45%, OR 2.17, 95% CI [1.48 to 3.17], p <0.001) were evident with PCI ( Figure 7 ). Another published meta-analysis on the same 4 randomised trials has yielded broadly similar results [4646. Capodanno D, Stone GW, Morice MC, Bass TA, Tamburino C. Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of randomised clinical data. J Am Coll Cardiol. 2011;58:1426-32. ].
A more recent meta-analysis of randomised clinical trials from 2001 and 2017, pooled 4 trials with a total of 4394 patients comparing the long-term safety of PCI versus CABG for ULMCA disease [289289. Giacoppo D, Colleran R, Cassese S, Frangieh AH, Wiebe J, Joner M, Schunkert H, Kastrati A, Byrne RA. Percutaneous Coronary Intervention vs Coronary Artery Bypass Grafting in Patients With Left Main Coronary Artery Stenosis: A Systematic Review and Meta-analysis. JAMA Cardiol. 2017;2:1079-1088. ]. The primary endpoint was a composite of all-cause mortality, myocardial infarction, or stroke at long-term follow-up. Kaplan-Meier curve reconstruction did not show significant variations over time between the techniques, with a 5-year incidence of all-cause death, myocardial infarction, or stroke of 18.3% (319 events) in patients treated with PCI and 16.9% (292 events) in patients treated with CABG. However, repeat revascularization after PCI was increased (HR, 1.70; 95% CI, 1.42 to 2.05; p<0.001). Interestingly, the authors have shown that pooled estimates of trials with ULMCA disease tended to significantly differ overall from those of trials with multivessel coronary artery disease without ULMCA stenosis.
UNPROTECTED LEFT MAIN PCI IN THE SETTING OF ACUTE CORONARY SYNDROME
Several studies have only recently reported registry experience of clinical outcomes of ULM PCI in the setting of acute coronary syndrome (ACS) [4747. Pappalardo A, Mamas MA, Imola F, Ramazzotti V, Manzoli A, Prati F, El-Omar M. Percutaneous coronary intervention of unprotected left main coronary artery disease as culprit lesion in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2011;4:618-26.
One of the first multicentre registry studies demonstrating outcomes in patients with acute MI with the culprit lesion in the LMS undergoing emergency PCI., 4848. Pedrazzini GB, Radovanovic D, Vassalli G, Surder D, Moccetti T, Eberli F, Urban P, Windecker S, Rickli H, Erne P. Primary percutaneous coronary intervention for unprotected left main disease in patients with acute ST-segment elevation myocardial infarction the AMIS (Acute Myocardial Infarction in Switzerland) plus registry experience. JACC Cardiovasc Interv. 2011;4:627-33. , 4949. Puricel S, Adorjan P, Oberhansli M, Stauffer JC, Moschovitis A, Vogel R, Goy JJ, Muller O, Eeckhout E, Togni M, Wenaweser P, Meier B, Windecker S, Cook S. Clinical outcomes after PCI for acute coronary syndrome in unprotected left main coronary artery disease: insights from the Swiss Acute Left Main Coronary Vessel Percutaneous Management (SALVage) study. EuroIntervention. 2011;7:697-704. ]. Specifically, Pappalardo et al [4747. Pappalardo A, Mamas MA, Imola F, Ramazzotti V, Manzoli A, Prati F, El-Omar M. Percutaneous coronary intervention of unprotected left main coronary artery disease as culprit lesion in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2011;4:618-26.
One of the first multicentre registry studies demonstrating outcomes in patients with acute MI with the culprit lesion in the LMS undergoing emergency PCI.] retrospectively reported a 2-centre experience (Giovanni Hospital, Rome, Italy, and Manchester Royal Infirmary, Manchester, United Kingdom) over a period of almost 3 years. 48 of 5, 261 (0.9%) patients admitted with an acute MI (and treated with PCI) underwent emergency PCI to a culprit ULMCA lesion. Almost one half of patients (45%) presented with a ST-segment elevation myocardial infarction (STEMI) or new left bundle branch block (LBBB). Presentation with cardiogenic shock was present in almost one half (45%) of patients and distal LMCA disease was present in over two thirds (71%) of patients. The mean age of patients was 70 ± 12.5 years. Multivessel PCI was performed in almost one half (48%) of cases. Angiographic procedural success was achieved in 92% of patients. Intra-aortic balloon pump (IABP) support was used in over half of the cases (54%), orotracheal intubation with assisted ventilation in 20% of cases, and pharmacological inotropic support in over one third (37%) of cases; all cardiogenic shock patients received all 3 therapies. Clinical outcomes demonstrated an in-hospital mortality of 32% in patients presenting with cardiogenic shock and 11.5% in patients who were haemodynamically stable at presentation, due in all cases to refractory multiorgan failure (overall mortality 21%). In-hospital MACE was reported in a quarter of patients. At 1-year follow-up in-hospital survivors had a mortality rate of 10.5%, with an incidence of MACE of 18.4%.
Pedrazzini et al [4848. Pedrazzini GB, Radovanovic D, Vassalli G, Surder D, Moccetti T, Eberli F, Urban P, Windecker S, Rickli H, Erne P. Primary percutaneous coronary intervention for unprotected left main disease in patients with acute ST-segment elevation myocardial infarction the AMIS (Acute Myocardial Infarction in Switzerland) plus registry experience. JACC Cardiovasc Interv. 2011;4:627-33. ] demonstrated in 6,666 patients - enrolled in the AMIS (Acute Myocardial Infarction in Switzerland) Plus registry covering 76 hospitals in Switzerland over a 5-year period - who underwent primary PCI for STEMI, that 348 patients (5.2%) underwent LMS PCI, either isolated (n=208, [3.1%]) or concomitant to PCI for other vessel segments (n=140, [2.1%]). Mean age of patients was 63.5 +/- 12.6 years. Presentation with cardiogenic shock occurred in 12.2% of patients; in-hospital mortality was remarkably low at 11%, compared to 21% as reported by Pappalardo et al. Presentation for primary PCI may be the key reason for the lower mortality reported in this registry.
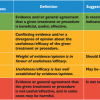
ANTIPLATELET THERAPY
Current guidelines support indefinite aspirin administration and at least 6-12 months dual antiplatelet therapy (DAPT) (with aspirin and clopidogrel) in patients receiving a DES (Class: I, Level of Evidence: B). These recommendations are, however, not specific for ULM PCI [3131. Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D, Vahanian A, Auricchio A, Bax J, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearney P, McDonagh T, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas PE, Widimsky P, Alfieri O, Dunning J, Elia S, Kappetein P, Lockowandt U, Sarris G, Vouhe P, von Segesser L, Agewall S, Aladashvili A, Alexopoulos D, Antunes MJ, Atalar E, Brutel de la Riviere A, Doganov A, Eha J, Fajadet J, Ferreira R, Garot J, Halcox J, Hasin Y, Janssens S, Kervinen K, Laufer G, Legrand V, Nashef SA, Neumann FJ, Niemela K, Nihoyannopoulos P, Noc M, Piek JJ, Pirk J, Rozenman Y, Sabate M, Starc R, Thielmann M, Wheatley DJ, Windecker S, Zembala M. Guidelines on myocardial Revascularisation: The Task Force on Myocardial Revascularisation of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501-55.
European Revascularisation Guidelines – an essential read!, 5050. Smith SC, Jr., Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pearson T, Pfeffer MA, Taubert KA. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47:2130-9. ].
Although the risk-benefit ratio of long-term DAPT is not well defined, many clinicians prolong DAPT long-term after ULM PCI with DES. Migliorini et al [5151. Migliorini A, Valenti R, Marcucci R, Parodi G, Giuliani G, Buonamici P, Cerisano G, Carrabba N, Gensini GF, Abbate R, Antoniucci D. High residual platelet reactivity after clopidogrel loading and long-term clinical outcome after drug-eluting stenting for unprotected left main coronary disease. Circulation. 2009;120:2214-21.
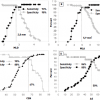
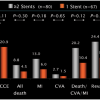
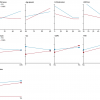
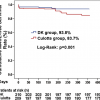
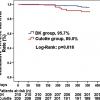
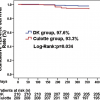
A pilot study associating long term clinical outcomes to platelet reactivity 12 hours after being loaded with clopidogrel prior to undergoing ULM PCI.] reported the outcomes of 215 patients who underwent ULM PCI with DES. All patients in this study had prospective platelet reactivity assessments by light transmittance aggregometry at least 12 hours after being administered a loading dose of 600 mg of clopidogrel. The incidence of high residual platelet reactivity (HRPR) at least 12 hours after being loaded with 600 mg clopidogrel was 18.6%. The 3-year cardiac mortality and stent thrombosis incidences were markedly higher in the high residual platelet reactivity (HRPR) group compared to the low residual platelet reactivity (LRPR) group ( Figure 8 ). Furthermore, HRPR after clopidogrel loading was demonstrated to be the only independent predictor of cardiac death (HR, 3.82; 95% CI, 1.38 to 10.54; p=0.010) and stent thrombosis (HR, 3.69; 95% CI, 1.12 to 12.09; p=0.031). Additional studies are required to resolve the role of platelet reactivity testing in patients undergoing ULM PCI thereby “tailoring” an antiplatelet regime to the individual and determining the optimal duration of DAPT administration.
SURVEILLANCE ANGIOGRAPHY POST LEFT MAIN PCI
Previous practice had been that routine surveillance angiography should be performed up to 6 months post ULM PCI based on historical registry data where BMS had been used in patients with extensive surgical risk [5252. Ellis SG, Tamai H, Nobuyoshi M, Kosuga K, Colombo A, Holmes DR, Macaya C, Grines CL, Whitlow PL, White HJ, Moses J, Teirstein PS, Serruys PW, Bittl JA, Mooney MR, Shimshak TM, Block PC, Erbel R. Contemporary percutaneous treatment of unprotected left main coronary stenoses: initial results from a multicenter registry analysis 1994-1996. Circulation. 1997;96:3867-72. , 5353. Tan WA, Tamai H, Park SJ, Plokker HW, Nobuyoshi M, Suzuki T, Colombo A, Macaya C, Holmes DR, Jr., Cohen DJ, Whitlow PL, Ellis SG. Long-term clinical outcomes after unprotected left main trunk percutaneous Revascularisation in 279 patients. Circulation. 2001;104:1609-14. ]. In the DES era this practice continued based on the continued assumption that the development of restenosis would peak between 2-4 months, potentially exposing patients to adverse clinical outcomes, including the risk of sudden death [5454. Valgimigli M, Chieffo A, Lefevre T, Colombo A, Morice MC, Serruys PW. Revisiting the incidence and temporal distribution of cardiac and sudden death in patients undergoing elective intervention for unprotected left main coronary artery stenosis in the drug eluting stent era. EuroIntervention. 2007;2:435-43. ].
Subsequently a pooled analysis of 340 patients treated at 3 European centres was undertaken to establish the rate and temporal distribution of cardiac and sudden death or out-of-hospital MI in patients undergoing elective ULMCA PCI with DES [5454. Valgimigli M, Chieffo A, Lefevre T, Colombo A, Morice MC, Serruys PW. Revisiting the incidence and temporal distribution of cardiac and sudden death in patients undergoing elective intervention for unprotected left main coronary artery stenosis in the drug eluting stent era. EuroIntervention. 2007;2:435-43. ]. Notably the rate of sudden death, cardiac death and stent thrombosis were shown to be very low and comparable to patients who underwent PCI for non-left main lesions. Moreover in the patient population at high surgical risk with extensive co-morbidity, the contribution to non-cardiac death was substantial. The findings from this study were one of the principle reasons that lead to the abandonment of the recommendation for routine 6 month angiographic follow in patients undergoing unprotected LM PCI in the DES era. Furthermore the results of this study were the primary reason the US FDA allowed for the SYNTAX trial to proceed in patients with ULMCA disease without the need for angiographic follow up.
Review of global evidence for unprotected left main intervention
- EXCEL trial has shown non-inferior outcomes (all-cause death, stroke or MI at 3-years) of PCI compared with CABG for patients with ULMCA and low or intermediate coronary artery anatomy complexity. NOBLE results comparing MACCE at 5-years between PCI with CABG showed that non-inferiority of PCI was not met, but mortality at 5-year was similar.
- Meta-analyses have consistently shown comparable mortality rates between CABG and PCI at at least 1 year in patients with ULMCA disease, with greater rates of CVA with CABG and repeat revascularisation with PCI. These meta-analyses have not looked at selecting patients by anatomical complexity or clinical comorbidity (discussed in the next section), which appears to enhance the appropriate identification of patients suitable for CABG or PCI
- ULM PCI in the setting of acute coronary syndrome or primary PCI have demonstrated in-hospital mortality rates of 21% and 11% respectively in registry studies, and lend support to the continued adoption of this practice
- A pilot study (n=215) has suggested a higher longer-term mortality and stent thrombosis-free survival in patients with a low residual platelet reactivity compared to patients with a high residual platelet reactivity undergoing ULM PCI. Further study is awaited
- Routine surveillance angiography post ULM PCI is no longer recommended, with comparable clinical events to patients who undergo PCI for non-left main lesions
Clinical Tools
The SYNTAX trial pioneered the Heart Team approach and has been incorporated as a class I recommendation in the latest myocardial revascularisation guidelines [5555. Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on myocardial Revascularisation. Eur J Cardiothorac Surg. 38 Suppl:S1-S52. , 246246. 246. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541-619 , 248248. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Marco J, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8 ]. A concise overview of the important established and evolving contemporary clinical tools for patients undergoing LMS revascularisation are detailed
Anatomical based scores
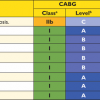
(ACC/AHA) lesion classification system
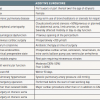
The ACC/AHA lesion classification system was one of the first angiographic scoring systems developed, comprising 11 angiographic variables with all lesions categorised into types (A, B1, B2, and C) [5656. Smith SC, Jr., Feldman TE, Hirshfeld JW, Jr., Jacobs AK, Kern MJ, King SB, 3rd, Morrison DA, O’Neill WW, Schaff HV, Whitlow PL, Williams DO, Antman EM, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol. 2006;47:e1-121. , 5757. Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM, Ritchie JL, Gibbons RJ, Cheitlin MD, Gardner TJ, Garson A, Jr., Russell RO, Jr., Ryan TJ, Smith SC, Jr. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345-57. ]. This system was predictive of the angiographic success of PCI with a subsequent prognostic effect on the early and late clinical outcomes in the pre-drug-eluting stent era ( Table 1 ) [5858. Krone RJ, Laskey WK, Johnson C, Kimmel SE, Klein LW, Weiner BH, Cosentino JJ, Johnson SA, Babb JD. A simplified lesion classification for predicting success and complications of coronary angioplasty. Registry Committee of the Society for Cardiac Angiography and Intervention. Am J Cardiol. 2000;85:1179-84. ]. Registry data from the drug-eluting stent era, however, has yielded conflicting results. The German Cypher registry (n=6,755) with approximately 8,000 lesions, 200 of which were ULM lesions, failed to show any significant association with clinical outcomes at 6 months; [5959. Khattab AA, Hamm CW, Senges J, Toelg R, Geist V, Bonzel T, Kelm M, Levenson B, Nienaber CA, Pfannebecker T, Sabin G, Schneider S, Tebbe U, Richardt G. Prognostic value of the modified American College of Cardiology/American Heart Association lesion morphology classification for clinical outcome after sirolimus-eluting stent placement (results of the prospective multicenter German Cypher Registry). Am J Cardiol. 2008;101:477-82. ] conversely, data from a small registry (n=255) was potentially predictive of mortality in unprotected LMS PCI at 1-year follow-up [6060. Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv. 2009;2:302-8. ].
SYNTAX score
The SYNTAX score (SYNTAX Score) is an anatomical tool that is calculated using dedicated software which integrates the number of lesions with their specific weighting factors, based on the amount of myocardium distal to the lesion and morphologic features of each single lesion ( Figure 9 ) [33. Sianos G, Morel MA, A.P. K, Morice MC, Colombo A, Dawkins K, van den Brand M, Dyck NV, Russell ME, Mohr FW, Serruys PW. (2005 ) The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-27. The birth of the SYNTAX Score. , 6161. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-6.
The SXscore methodology and its association with clinical outcomes from the SYNTAX trial., 6262. SYNTAX score calculator: http://www.syntaxscore.com. SYNTAX working-group. Launched 19th May 2009. ]. The SYNTAX Score was developed by combining the importance of a diseased coronary artery segment by vessel-segment weighting (modified Leaman score), [44. Leaman DM, Brower RW, Meester GT, Serruys P, van den Brand M. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation. 1981;63:285-99. ] adverse characteristics of such a lesion for revascularisation (ACC/AHA lesion classification), [5656. Smith SC, Jr., Feldman TE, Hirshfeld JW, Jr., Jacobs AK, Kern MJ, King SB, 3rd, Morrison DA, O’Neill WW, Schaff HV, Whitlow PL, Williams DO, Antman EM, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol. 2006;47:e1-121. , 5757. Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM, Ritchie JL, Gibbons RJ, Cheitlin MD, Gardner TJ, Garson A, Jr., Russell RO, Jr., Ryan TJ, Smith SC, Jr. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345-57. ] and the modified Duke/Institut Cardiovasculaire Paris Sud (ICPS) system [6363. Topol EJ. Textbook of Interventional Cardiology, 3rd ed. Philadelphia: WB Saunders 1999. , 6464. Lefevre T, Louvard Y, Morice MC, Dumas P, Loubeyre C, Benslimane A, Premchand RK, Guillard N, Piechaud JF. Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc Interv. 2000;49:274-83. ] classification for bifurcation lesions. The Medina classification system [6565. Medina A, Suarez de Lezo J, Pan M. [A new classification of coronary bifurcation lesions]. Rev Esp Cardiol. 2006;59:183. ] for bifurcation lesions was subsequently incorporated into the SYNTAX Score algorithm.
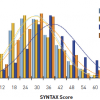
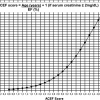
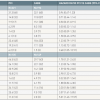
The tertiles of lesion complexity of the SYNTAX Score were derived from tertiles of the normal distribution of the SYNTAX Scores within the randomised population of the SYNTAX trial. Importantly, within the randomised surgical and PCI populations, there was no skewing of the data, with the normal distribution of the SYNTAX Score in the populations being superimposable on each other ( Figure 10 ) [6161. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-6.
The SXscore methodology and its association with clinical outcomes from the SYNTAX trial.]. Consequently, the upper boundary of the lowest tertile was 22 (low risk), the second tertile ranged from 23 to 32 (intermediate risk), and the highest tertile was equal to or greater than 33 (high risk).
Although the landmark Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) trial established that surgery was the standard of care for patients with LMS, several important findings from this study identified a subset of patients who could safely be treated with CABG or PCI, at up to 3 years follow-up. An important point to emphasise is that the LMS population of the SYNTAX trial involved a population of patients with isolated LMS disease, or associated with one, two or three vessel disease (3VD) [2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. , 6666. Ong AT, Serruys PW, Mohr FW, Morice MC, Kappetein AP, Holmes DR, Jr., Mack MJ, van den Brand M, Morel MA, van Es GA, Kleijne J, Koglin J, Russell ME. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J. 2006;151:1194-204. ].
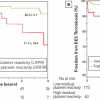
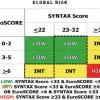
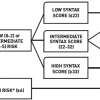
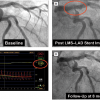
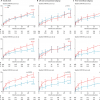
From the clinician’s perspective, the important findings of the SYNTAX trial include: tertiles for the SYNTAX Score (0-22, 32-32, ≥33) had a direct and significant effect on 3-year ( Figure 11 ) and 5-year ( Figure e2 ) outcomes in the LMS PCI group [6767. The Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery: The SYNTAX Study. The 4-year Outcomes of the SYNTAX trial in the Subset of Patients With Left Main Disease. Patrick W. Serruys, MD PhD Erasmus Medical Center. On behalf of the SYNTAX investigators. Tuesday, November 8th 11:46. Oral Abstract Sessions: Left Main and Bifurcation PCI. TCT 2011. San Francisco, United States. , 249249. Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR Jr, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629-38 , 250250. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Choi JW, Ruzyllo W, Religa G, Huang J, Roy K, Dawkins KD, Mohr F. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 2014;129:2388-94. ]. This, however, was not evident in the CABG population as the bypass grafts could be anastomosed distal to the proximal coronary disease, regardless of the disease complexity, provided there were suitable distal targets [2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. ].
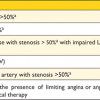
Within the LMS cohort of the SYNTAX trial, a low-intermediate SYNTAX Score (SYNTAX Score <33) was associated with similar surgical and percutaneous clinical outcomes (death and MACCE) at 3 and 5 years ( Figure 11 Figure e2 Figure e3 Table e2 ). Surgical revascularisation remained the standard of care in patients with a high SYNTAX Score (SYNTAX Score >32) [6767. The Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery: The SYNTAX Study. The 4-year Outcomes of the SYNTAX trial in the Subset of Patients With Left Main Disease. Patrick W. Serruys, MD PhD Erasmus Medical Center. On behalf of the SYNTAX investigators. Tuesday, November 8th 11:46. Oral Abstract Sessions: Left Main and Bifurcation PCI. TCT 2011. San Francisco, United States. , 249249. Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR Jr, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629-38 , 250250. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Choi JW, Ruzyllo W, Religa G, Huang J, Roy K, Dawkins KD, Mohr F. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 2014;129:2388-94. ]. This observation formed the basis of the on-going EXCEL randomised trial comparing the clinical outcomes between CABG and PCI for low-intermediate SYNTAX Scores (SYNTAX Score ≤32) [2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. , 6868. Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Stahle E, Dawkins KD, Mohr FW, Serruys PW, Colombo A. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125-34. ].
The concept of a high SYNTAX Score (>32) being able to identify a high-risk population within the LMS PCI population in the SYNTAX trial [2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. , 6161. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-6.
The SXscore methodology and its association with clinical outcomes from the SYNTAX trial.] has since been validated in multiple registries [77. Park DW, Kim YH, Yun SC, Song HG, Ahn JM, Oh JH, Kim WJ, Lee JY, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug-eluting stents or coronary artery bypass grafting. J Am Coll Cardiol. 2011;57:2152-9.
High quality registry information associating coronary artery disease complexity (as defined by the SXscore) in patients undergoing ULM PCI to long term (5 year) clinical outcomes. Currently subject to the ongoing EXCEL trial., 2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 6060. Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv. 2009;2:302-8. , 6969. Chakravarty T, Buch MH, Naik H, White AJ, Doctor N, Schapira J, Mirocha JM, Fontana G, Forrester JS, Makkar R. Predictive accuracy of SYNTAX score for predicting long-term outcomes of unprotected left main coronary artery Revascularisation. Am J Cardiol. 2011;107:360-6. , 7070. Kim Y-H, Park D-W, Kim W-J, Lee J-Y, Yun S-C, Kang S-J, Lee S-W, Lee CW, Park S-W, Park S-J. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score for Prediction of Outcomes After Unprotected Left Main Coronary Revascularisation. JACC Cardiovasc Interv. 2010;3:612-623. , 7171. Capodanno D, Capranzano P, Di Salvo ME, Caggegi A, Tomasello D, Cincotta G, Miano M, Patane M, Tamburino C, Tolaro S, Patane L, Calafiore AM. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc Interv. 2009;2:731-8. , 7272. Onuma Y, Girasis C, Piazza N, Garcia-Garcia HM, Kukreja N, Garg S, Eindhoven J, Cheng JM, Valgimigli M, van Domburg R, Serruys PW. Long-term clinical results following stenting of the left main stem: insights from RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital) and T-SEARCH (Taxus-Stent Evaluated at Rotterdam Cardiology Hospital) Registries. JACC Cardiovasc Interv. 2010;3:584-94. ]. A higher SYNTAX Score tertile has consistently been shown to be a correlate of a high-risk population with poorer outcomes at short and long-term follow-up compared to lower SYNTAX Score tertiles.
Within the 3-vessel disease (3VD) cohort of the SYNTAX trial, a low SYNTAX Score (<23) was associated with similar surgical and percutaneous clinical outcomes in terms of all-cause death and MACCE (major adverse cardiac and cerebrovascular events) at up to 5 years [6868. Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Stahle E, Dawkins KD, Mohr FW, Serruys PW, Colombo A. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125-34. , 249249. Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR Jr, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629-38 ] ( Figure e2 ).
Providing that a certain threshold of surgical risk is not exceeded, undergoing surgical revascularisation may confer a morbidity and possible mortality advantage in patients with a higher clinical comorbidity. Further study is required to confirm these exploratory findings from a post hoc analysis of the SYNTAX trial [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ].
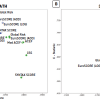
Importantly, it would appear that the outcomes in the LMS PCI population appear to be predominantly affected by the increasing presence of complex coronary disease, as defined by a higher SYNTAX Score, and its association with anatomical complexities, such as the increasing prevalence of 3VD (compared to isolated LMS disease, or LMS coupled with one or two vessel disease), multiple bifurcations and the presence of total occlusions ( Figure 12 ). Other factors such as clinical comorbidity also plays a significant role [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. , 1919. Farooq V, Brugaletta S, Serruys PW. Contemporary and evolving risk scoring algorithms for percutaneous coronary intervention. Heart. 2011;97:1902-13. , 251251. Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, Kappetein AP, Colombo A, Holmes DR Jr, Mack M, Feldman T, Morice MC, Ståhle E, Onuma Y, Morel MA, Garcia-Garcia HM, van Es GA, Dawkins KD, Mohr FW, Serruys PW. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639-50 , 252252. Farooq V, van Klaveren D, Steyerberg EW, Serruys PW. SYNTAX score II - Authors’ reply. Lancet. 2013;381:1899-900 ].
It has previously been suggested that the SYNTAX Score is a reflection of the underlying comorbidity of the patient [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]. This notion is supported by the 10-year predicted Framingham risk scores being recently shown to have a significant and direct relationship with the prevalence and magnitude of coronary artery calcium scores [1818. Okwuosa TM, Greenland P, Ning H, Liu K, Bild DE, Burke GL, Eng J, Lloyd-Jones DM. Distribution of Coronary Artery Calcium Scores by Framingham 10-Year Risk Strata in the MESA (Multi-Ethnic Study of Atherosclerosis) Potential Implications for Coronary Risk Assessment. J Am Coll Cardiol. 2011;57:1838-45. ]. Furthermore, the extent and severity of coronary artery disease have previously been shown to be associated with the ankle-brachial pressure index (ABPI)[88. Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Lee AJ, Price JF, d’Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodriguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197-208. , 1212. Papamichael CM, Lekakis JP, Stamatelopoulos KS, Papaioannou TG, Alevizaki MK, Cimponeriu AT, Kanakakis JE, Papapanagiotou A, Kalofoutis AT, Stamatelopoulos SF. Ankle-brachial index as a predictor of the extent of coronary atherosclerosis and cardiovascular events in patients with coronary artery disease. Am J Cardiol. 2000;86:615-8. ] and the common carotid intima-media thickness, [1313. Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262-9. , 1717. Korkmaz L, Bektas H, Korkmaz AA, Agac MT, Acar Z, Erkan H, Celik S. Increased Carotid Intima-Media Thickness is Associated With Higher SYNTAX Score. Angiology. 2011 Sep 22. [Epub ahead of print]. ] both markers of systemic atherosclerosis, which in turn have also been associated with cardiovascular mortality and coronary events, respectively.
Further support for these hypotheses comes from Park et al in the MAIN-COMPARE (Revascularisation for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascu-larisation) registry (n=1,146), in patients who underwent surgical (n=501) or percutaneous (n=645) revascularisation for ULMCA disease [77. Park DW, Kim YH, Yun SC, Song HG, Ahn JM, Oh JH, Kim WJ, Lee JY, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug-eluting stents or coronary artery bypass grafting. J Am Coll Cardiol. 2011;57:2152-9.
High quality registry information associating coronary artery disease complexity (as defined by the SXscore) in patients undergoing ULM PCI to long term (5 year) clinical outcomes. Currently subject to the ongoing EXCEL trial.]. Differences in long-term mortality (5-year) were evident dependent on the complexity of the concomitant coronary disease as defined by tertiles of the SYNTAX Score ( Figure 13 ).
PRECOMBAT trial
Within the Premier of Randomised Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT) trial (n=600), [3030. Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, Lee JY, Kim WJ, Kang SJ, Lee SW, Lee CW, Park SW, Chung CH, Lee JW, Lim DS, Rha SW, Lee SG, Gwon HC, Kim HS, Chae IH, Jang Y, Jeong MH, Tahk SJ, Seung KB. Randomised trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364:1718-27. ]. Park et al demonstrated that PCI with SES was non-inferior to CABG with respect to MACCE at 1 year. Notably, the non-inferiority margin of the study was wide, making the results of the study non-clinically directive. In addition, an unexpectedly low event rate occurred within this study compared to previous randomised and non-randomised trials: this contributed significantly to the trial being underpowered.
Furthermore, there were no statistically significant differences in the incidence of MACCE at 1-year based upon the SYNTAX Score: this in part may be a reflection of the less complex disease (mean SYNTAX Score: SYNTAX LEMANS (left main population) 30; PRECOMBAT 25) and the lower clinical risk profile (mean EuroSCORE: SYNTAX LEMANS (left main population) 30 3.8; PRECOMBAT 2.7) of the patients in PRECOMBAT compared to the left main population of the SYNTAX trial; noting that the low to moderate SYNTAX Scores in the left main population of the SYNTAX trial had comparable outcomes to surgical or percutaneous revascularisation [2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial.].
Drug Eluting stent for LefT main coronary Artery disease: the DELTA Registry
Within the DELTA registry (n=2,775), [7373. Chieffo A, Meliga E, Latib A, Park SJ, Onuma Y, Capranzano P, Valgimigli M, Jegere S, Makkar R, Palacios I, Kim YH, Buszman P, Chakravarty T, Sheiban I, Mehran R, Naber C, Margey R, Agnihotri A, Marra S, Capodanno D, Leon M, Moses J, Fajadet J, Lefevre T, Morice MC, Erglis A, Tamburino C, Alfieri O, Serruys PW, Colombo A. Drug Eluting stent for LefT main coronary Artery disease: the DELTA Registry A Multicenter Registry Evaluating PCI vs. CABG for Left Main Treatment. JACC Cardiovasc Interv. In Press 2012. ] a multicentre, multinational registry evaluating PCI with first-generation DES (n=1,874, PES or SES) against CABG (n=901) for ULMCA disease, no differences in the primary composite endpoint of all-cause death, CVA and MI were seen (HR 1.11; 95% CI 0.85-1.42; p=0.47). An advantage of CABG over PCI was observed in the composite secondary endpoint of MACCE (unadjusted HR 1.58; 95% CI 1.32-1.90; p<0.0001; adjusted HR 1.64; 95% CI 1.33-2.03; p<0.0001). The results of this study were affected by significant differences in SYNTAX Scores between the PCI and CABG groups (28.6±14.3 vs. 38.9±13.2; p<0.01), reflecting the contemporary practice of patients with higher SYNTAX Scores undergoing CABG. Notably, despite the imbalances in baseline characteristics and more complex coronary disease in the CABG population, the SYNTAX Score was shown to be an independent predictor of the primary endpoint.
Within the LEMAX Pilot study (n=173), investigating ULM PCI with the second generation XIENCE V Everolimus Eluting Stent, both a high SYNTAX Score and a high EuroSCORE were associated with adverse clinical outcomes at one year ( Figure 14 ).
French Left Main Taxus (FLM Taxus) and the Left Main Xience (LEMAX) registries.
A subsequent study from the French Left Main Taxus (FLM Taxus) and the Left Main with Xience (LEMAX) registries, comparing 2-year outcomes using either EES or PES, demonstrated a reduction in target lesion failure (TLF) – a composite of cardiac death, target vessel MI, and clinically driven TLR – with PES, by 53% at 2 years (EES: 7.6% vs. PES: 16.3%, p=0.01) [7474. Moynagh A, Salvatella N, Harb T, Darremont O, Boudou N, Dumonteil N, Lefèvre T, Carrié D, Louvard Y, Leymarie JL, Chevalier B, Morice MC. Two-year outcomes of Everolimus Vs. Paclitaxel-eluting stent for the treatment of unprotected left main lesions. A matched comparison of patients included in the French Left Main Taxus (FLM Taxus) and the LEft MAin Xience (LEMAX) registries. EuroIntervention. 2011 ;7:689-96. ]. Significant differences in target vessel MI (PES: 9.9% vs. EES: 4.1%, p=0.04) and target vessel failure (PES: 16.3% vs. EES: 7.6%, p=0.01) were associated with EES at 2 years. Furthermore higher SYNTAX Score groups (intermediate-high) demonstrated a trend towards improved clinical benefit in patients treated with EES compared to PES ( Figure 15 ).
Functional SYNTAX score
The Fractional Flow Reserve (FFR) versus Angiography for Guiding PCI in Patients with Multivessel Evaluation study (FAME) determined the potential prognostic impact of PCI guided by FFR measurements to determine the functional significance of an individual coronary lesion before intervention [7575. Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, Maccarthy PA, Van’t Veer M, Pijls NH. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816-21. , 7676. Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, van’t Veer M, Klauss V, Manoharan G, Engstrom T, Oldroyd KG, Ver Lee PN, MacCarthy PA, De Bruyne B. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol. 2010;56:177-84. ]. The newly dubbed “Functional SYNTAX score” (Functional SXscore) essentially incorporates FFR measurements into the SYNTAX Score calculation, and was recently shown potentially to improve the stratification of low and high risk patients, when compared to the conventional visual-based angiographic approach [7777. Nam CW, Mangiacapra F, Entjes R, Chung IS, Sels JW, Tonino PA, De Bruyne B, Pijls NH, Fearon WF. Functional SYNTAX Score for Risk Assessment in Multivessel Coronary Artery Disease. J Am Coll Cardiol. 2011;58:1211-8.
The novel concept of improving the predictive ability of the SXscore with pressure wire assessment of lesions (Functional SXscore).].
In a retrospective sub-analysis of almost 500 patients with multivessel disease from the FFR-guided arm of the FAME study, the primary benefit appeared in reclassifying higher-risk groups into lower-risk categories without any adverse sequelae, in terms of MACE and death or MI at 1 year [7777. Nam CW, Mangiacapra F, Entjes R, Chung IS, Sels JW, Tonino PA, De Bruyne B, Pijls NH, Fearon WF. Functional SYNTAX Score for Risk Assessment in Multivessel Coronary Artery Disease. J Am Coll Cardiol. 2011;58:1211-8.
The novel concept of improving the predictive ability of the SXscore with pressure wire assessment of lesions (Functional SXscore).]. It should however be emphasised that subjects in the FAME Study had substantially less complex coronary artery disease (mean SYNTAX Score 14.8±6.0) compared to the PCI arm of the SYNTAX Trial (mean SYNTAX Score 28.4±11.5), and that subjects with left main coronary artery disease were not investigated. Prospective validation studies of the functional SYNTAX Score in complex coronary artery disease are at the time of writing ongoing (SYNTAX II Trial - ClinicalTrials.gov Identifier: NCT02015832; FAME 3 Trial - ClinicalTrials.gov Identifier: NCT02100722).
One further caveat to the functional SYNTAX Score approach is that QCA, and even 3-dimensional QCA, have been shown to be more reliable than visual estimation of vessel size [7878. Yong ASC, Ng ACC, Brieger D, Lowe HC, Ng MKC, Kritharides L. Three-dimensional and two-dimensional quantitative coronary angiography, and their prediction of reduced fractional flow reserve. Eur Heart J. 2011; 2011;32:345-53. , 7979. Onuma Y, Girasis C, Aben JP, Sarno G, N. P, Lokkerbol C, Morel MA, Serruys PW. A novel dedicated 3-dimensional quantitative coronary analysis methodology for bifurcation lesions. EuroIntervention. 2011;7:629-35. , 8080. Reiber JH, Serruys PW. Quantitative Coronary Angiography: Methodologies. In. Quantitative Coronary Angiography. Dordrecht, The Netherlands: Kluwer Academic Publishers. 1991, 98-102. ]. If QCA measurements of vessel size had been used to calculate the SYNTAX Score - instead of visual estimation - this may have reduced the benefits of the functional SYNTAX Score compared to the SYNTAX Score derived from visual estimation. Non-invasive calculation of the functional SYNTAX Score has recently been proposed (HeartFlow Inc., Redwood City, CA, USA) [8282. Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79(6 Pt 2):I3-12. ]. This allows for the simultaneous assessment of anatomy and measurement of the haemodynamic significance of lesions – to permit the non-invasive computation of FFR – utilising computational fluid dynamic techniques applied to coronary computed tomographic (CT) angiography. Additionally, the potential use of “virtual PCI” further adds to the appeal of this rapidly developing technology ( Figure 16 ).
Validation data of the non-invasive fractional flow reserve computed tomography (FFRCT) technique was reported in the DISCOVER FLOW trial [8181. Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, Dunning A, Defrance T, Lansky A, Leipsic J, Min JK. Diagnosis of Ischemia-Causing Coronary Stenoses by Noninvasive Fractional Flow Reserve Computed From Coronary Computed Tomographic Angiograms Results From the Prospective Multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) Study. J Am Coll Cardiol. 2011;58:1989-97.
Perhaps the future of the SXscore? A non-invasive functional assessment of the SXscore.]. Within this study it was demonstrated that FFRCT could dramatically improve the diagnostic accuracy of CT imaging without the need for invasive FFR imaging. In 159 vessels - with at least a 50% stenosis - in 103 patients at 5 hospitals, a high correlation between FFRCT and invasive FFR measurements was demonstrated. Consequently, this allowed for a marked improvement in the accuracy of the reporting of CT coronary angiograms, with the potential to improve the selection of patients for invasive angiography and revascularisation. Further validation was undertaken in the larger multicentre DeFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography) trial. Among 407 vessels from 252 patients treated from 17 centers, in 5 countries, FFRCT was associated with improved diagnostic accuracy and discrimination (area under the receiver operating characteristic curve [AUC], 0.81; 95% CI, 0.75-0.86; P < .001) compared to obstructive coronary artery disease diagnosed by CT alone (AUC, 0.68; 95% CI, 0.62-0.74).[253253. Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, Erglis A, Lin FY, Dunning AM, Apruzzese P, Budoff MJ, Cole JH, Jaffer FA, Leon MB, Malpeso J, Mancini GB, Park SJ, Schwartz RS, Shaw LJ, Mauri L. JAMA. 2012;308:1237-45 ]
Clinical based tools
The Parsonnet
The Parsonnet score is an operative risk score, published in 1989, which consists of 14 clinical variables [8282. Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79(6 Pt 2):I3-12. ]. In 2005 Valgimigli et al demonstrated that the Parsonnet score was an independent long-term (approximately 3-year) predictor of MACE after ULM PCI from the Rotterdam RESEARCH and T-SEARCH registries [8383. Valgimigli M, van Mieghem CAG, Ong ATL, Aoki J, Granillo GAR, McFadden EP, Kappetein AP, de Feyter PJ, Smits PC, Regar E, Van der Giessen WJ, Sianos G, de Jaegere P, Van Domburg RT, Serruys PW. Short- and Long-Term Clinical Outcome After Drug-Eluting Stent Implantation for the Percutaneous Treatment of Left Main Coronary Artery Disease: Insights From the Rapamycin-Eluting and Taxus Stent Evaluated At Rotterdam Cardiology Hospital Registries (RESEARCH and T-SEARCH). Circulation. 2005;111:1383-1389. ]. Subsequently, Lee et al further demonstrated the Parsonnet score to be an independent predictor of MACCE in patients with ULMCA disease undergoing percutaneous revascularisation with DES [8484. Lee MS, Kapoor N, Jamal F, Czer L, Aragon J, Forrester J, Kar S, Dohad S, Kass R, Eigler N, Trento A, Shah PK, Makkar RR. Comparison of coronary artery bypass surgery with percutaneous coronary intervention with drug-eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2006;47:864-70. ]. More recently, Chakravarty et al demonstrated that by adding the Parsonnet score as a covariate to the SYNTAX Score this improved the long-term (approximately 4-year) predictive ability of the score in predicting MACCE after LMS PCI [7070. Kim Y-H, Park D-W, Kim W-J, Lee J-Y, Yun S-C, Kang S-J, Lee S-W, Lee CW, Park S-W, Park S-J. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score for Prediction of Outcomes After Unprotected Left Main Coronary Revascularisation. JACC Cardiovasc Interv. 2010;3:612-623. ].
EuroSCORE (European System for Cardiac Operative Risk Evaluation)
The EuroSCORE is an established risk score, utilising 17 clinical variables, within cardiothoracic surgical practice for predicting operative mortality. It has been validated in many populations around the world [8585. Gogbashian A, Sedrakyan A, Treasure T. EuroSCORE: a systematic review of international performance. Eur J Cardiothorac Surg. 2004;25:695-700. , 8686. Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9-13. , 8787. Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881-2. ]. In use since 1999, the score was derived from almost 20,000 consecutive patients from 128 hospitals in 8 European countries. The additive EuroSCORE assigns an individual score to 17 clinical variables ( Table 2 ), with a low EuroSCORE risk tertile ranging from 1-2, intermediate risk tertile from 3-5, and a high risk tertile of 6+.
The subsequently developed logistic EuroSCORE has been suggested to allow for a more accurate risk prediction within the CABG cohort, in particular for the high-risk population, where the additive model was found to lead to a potential underestimation of risk [8585. Gogbashian A, Sedrakyan A, Treasure T. EuroSCORE: a systematic review of international performance. Eur J Cardiothorac Surg. 2004;25:695-700. , 8686. Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9-13. , 8787. Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881-2. , 8888. Bhatti F, Grayson AD, Grotte G, Fabri BM, Au J, Jones M, Bridgewater B. The logistic EuroSCORE in cardiac surgery: how well does it predict operative risk? Heart. 2006;92:1817-20. ]. Conversely, the logistic EuroSCORE has been shown potentially to overestimate observed mortality, with its accuracy at predicting risk varying in different surgical subgroups [8888. Bhatti F, Grayson AD, Grotte G, Fabri BM, Au J, Jones M, Bridgewater B. The logistic EuroSCORE in cardiac surgery: how well does it predict operative risk? Heart. 2006;92:1817-20. , 8989. Grant SW, Grayson AD, Jackson M, Au J, Fabri BM, Grotte G, Jones M, Bridgewater B. Does the choice of risk-adjustment model influence the outcome of surgeon-specific mortality analysis? A retrospective analysis of 14, 637 patients under 31 surgeons. Heart 2008;94:1044-9. ].
Kim et al first demonstrated that a high-risk tertile of the additive EuroSCORE was an independent predictor of death/MI after ULM PCI with SES [9090. Kim YH, Ahn JM, Park DW, Lee BK, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. EuroSCORE as a predictor of death and myocardial infarction after unprotected left main coronary stenting. Am J Cardiol. 2006;98:1567-70. ]. Subsequently, the SYNTAX trial further established the utility of the EuroSCORE within both the surgical and the percutaneously revascularised patient with ULMCA disease ( Table 3 ) [2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. ]. Ensuing studies have since confirmed the additional clinical utility of the EuroSCORE in patients with ULMCA disease [7070. Kim Y-H, Park D-W, Kim W-J, Lee J-Y, Yun S-C, Kang S-J, Lee S-W, Lee CW, Park S-W, Park S-J. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score for Prediction of Outcomes After Unprotected Left Main Coronary Revascularisation. JACC Cardiovasc Interv. 2010;3:612-623. , 7272. Onuma Y, Girasis C, Piazza N, Garcia-Garcia HM, Kukreja N, Garg S, Eindhoven J, Cheng JM, Valgimigli M, van Domburg R, Serruys PW. Long-term clinical results following stenting of the left main stem: insights from RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital) and T-SEARCH (Taxus-Stent Evaluated at Rotterdam Cardiology Hospital) Registries. JACC Cardiovasc Interv. 2010;3:584-94. , 9090. Kim YH, Ahn JM, Park DW, Lee BK, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. EuroSCORE as a predictor of death and myocardial infarction after unprotected left main coronary stenting. Am J Cardiol. 2006;98:1567-70. , 9191. Min SY, Park DW, Yun SC, Kim YH, Lee JY, Kang SJ, Lee SW, Lee CW, Kim JJ, Park SW, Park SJ. Major predictors of long-term clinical outcomes after coronary Revascularisation in patients with unprotected left main coronary disease: analysis from the MAIN-COMPARE study. Circ Cardiovasc Interv. 2010;3:127-33. , 9292. Rekik S, Brunet J, Bayet G, Hager FX, Meille L, Quatre JM, Sainsous J. EuroSCORE is a good global predictor of long-term outcomes in high-risk but not in low-risk patients after unprotected left main angioplasty. Catheter Cardiovasc Interv. 2011;77:625-32. , 9393. Capodanno D, Miano M, Cincotta G, Caggegi A, Ruperto C, Bucalo R, Sanfilippo A, Capranzano P, Tamburino C. EuroSCORE refines the predictive ability of SYNTAX score in patients undergoing left main percutaneous coronary intervention. Am Heart J. 2010;159:103-9. , 9494. Capodanno D, Caggegi A, Miano M, Cincotta G, Dipasqua F, Giacchi G, Capranzano P, Ussia G, Di Salvo ME, La Manna A, Tamburino C. Global Risk Classification and Clinical SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) Score in Patients Undergoing Percutaneous or Surgical Left Main Revascularisation. J Am Coll Cardiol Intv. 2011;4:287-297. , 9595. Luz A, Hughes C, Magalhaes R, Bisceglia T, Descoutures F, Tamamm K, Tchetche D, Sauguet A, Farah B, Fajadet J. Stent implantation in aorto-ostial lesions: long-term follow-up and predictors of outcome. EuroIntervention. 2011;7:1069-76. , 9696. Rodes-Cabau J, Deblois J, Bertrand OF, Mohammadi S, Courtis J, Larose E, Dagenais F, Dery JP, Mathieu P, Rousseau M, Barbeau G, Baillot R, Gleeton O, Perron J, Nguyen CM, Roy L, Doyle D, De Larochelliere R, Bogaty P, Voisine P. Nonrandomised comparison of coronary artery bypass surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease in octogenarians. Circulation. 2008;118:2374-81. ]. Only one study has examined the logistic EuroSCORE in PCI patients; however, few differences were found in stratifying risk when compared to the additive EuroSCORE [9797. Romagnoli E, Burzotta F, Trani C, Siviglia M, Biondi-Zoccai GG, Niccoli G, Leone AM, Porto I, Mazzari MA, Mongiardo R, Rebuzzi AG, Schiavoni G, Crea F. EuroSCORE as predictor of in-hospital mortality after percutaneous coronary intervention. Heart. 2009;95:43-8. ]. Within the SYNTAX population the additive EuroSCORE has been demonstrated to be superior to the logistic EuroSCORE in predicting outcomes after PCI [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]. Despite these findings, it should be emphasised that as the EuroSCORE was developed to predict in-hospital operative mortality following cardiac surgery, certain components of the EuroSCORE, such as operative factors ( Table 2 ), are not likely to be applicable to clinical outcomes after undergoing PCI [9898. Park SJ. Prediction of outcomes after percutaneous coronary intervention for unprotected left main coronary artery stenosis using the EuroSCORE. Catheter Cardiovasc Interv. 2011;77:633. ].
EuroSCORE II
More recently the EuroSCORE II was developed to improve the risk predictions of the EuroSCORE I. The EuroSCORE II was developed on newer data to reflect more contemporary surgical practice given that cardiac surgical mortality has significantly reduced in the last 15 years despite older and sicker patients, and that the previous additive and logistic EuroSCORE models were suggested to be representative of outdated surgical practice. [274274. Nashef SA, Roques F, Sharples LD et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734-44; discussion 744-5. , 275275. Nashef SA, Sharples LD. Editorial comment: Pride without prejudice: EuroSCORE II, the STS score and the high-risk patient subset. Eur J Cardiothorac Surg. 2013;44:1012. , 276276. Nashef SA, Sharples LD, Roques F, Lockowandt U. EuroSCORE II and the art and science of risk modelling. Eur J Cardiothorac Surg. 2013;43:695-6. , 277277. Guida P, Mastro F, Scrascia G, Whitlock R, Paparella D. Performance of the European System for Cardiac Operative Risk Evaluation II: A meta-analysis of 22 studies involving 145,592 cardiac surgery procedures. J Thorac Cardiovasc Surg. 2014. ]
The EuroSCORE II was shown to be better calibrated (actual mortality: 4.18%; predicted: 3.95%) compared to the original EuroSCORE model (actual: 3.9%; additive predicted: 5.8%; logistic predicted: 7.57%) whilst preserving discrimination (area under the receiver operating characteristic curve of 0.8095). It should however be noted that regular revalidation of EuroSCORE II will need to be continued to identify calibration drift or clinical inconsistencies as seen in previous versions. [277277. Guida P, Mastro F, Scrascia G, Whitlock R, Paparella D. Performance of the European System for Cardiac Operative Risk Evaluation II: A meta-analysis of 22 studies involving 145,592 cardiac surgery procedures. J Thorac Cardiovasc Surg. 2014. , 278278. Grant SW, Hickey GL, Dimarakis I et al. How does EuroSCORE II perform in UK cardiac surgery; an analysis of 23 740 patients from the Society for Cardiothoracic Surgery in Great Britain and Ireland National Database. Heart. 2012;98:1568-72. ]
Combined (anatomical and clinical) risk scores
Criticism has emerged that clinical factors are not taken into account in the risk stratification of patients with ULMCA disease, with the sole reliance on anatomical factors, namely the anatomical SYNTAX Score [7070. Kim Y-H, Park D-W, Kim W-J, Lee J-Y, Yun S-C, Kang S-J, Lee S-W, Lee CW, Park S-W, Park S-J. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score for Prediction of Outcomes After Unprotected Left Main Coronary Revascularisation. JACC Cardiovasc Interv. 2010;3:612-623. , 9090. Kim YH, Ahn JM, Park DW, Lee BK, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. EuroSCORE as a predictor of death and myocardial infarction after unprotected left main coronary stenting. Am J Cardiol. 2006;98:1567-70. , 9797. Romagnoli E, Burzotta F, Trani C, Siviglia M, Biondi-Zoccai GG, Niccoli G, Leone AM, Porto I, Mazzari MA, Mongiardo R, Rebuzzi AG, Schiavoni G, Crea F. EuroSCORE as predictor of in-hospital mortality after percutaneous coronary intervention. Heart. 2009;95:43-8. , 9999. Applegate RJ. Toward better stratification of patients with left main disease: value of clinical and angiographic-derived risk scores. JACC Cardiovasc Interv. 2011;4:298-9. ]. Consequently, potentially important prognostic and morbidity information may be missing in risk stratifying patients with ULMCA disease electing to undergo surgical or percutaneous revascularisation. The following combined (anatomical and clinical) risk scores have been investigated in an attempt to overcome some of these limitations.
Clinical SYNTAX score
Ranucci et al [100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 101101. Ranucci M, Castelvecchio S. The ACEF score one year after: a skeleton waiting for muscles, skin, and internal organs. EuroIntervention. 2010;6:549-53. ] demonstrated using only three clinical variables, namely age, preoperative serum creatinine value and left ventricular ejection fraction (LVEF) - a relatively simple risk model for assessing operative mortality risk in elective cardiac operations (ACEF score) ( Figure e4 ). Notably, despite the simplicity of the ACEF model, its clinical performance appeared to be comparable to either the additive or the logistic EuroSCORE in predicting in-hospital mortality after CABG.
The underlying rationale for the clinical SYNTAX score was to combine the anatomical SYNTAX Score with a variant of the ACEF score (modified ACEF score, using creatinine clearance assessment instead of the serum creatinine), the latter having proven to be comparable to the EuroSCORE in patients undergoing elective CABG [100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 101101. Ranucci M, Castelvecchio S. The ACEF score one year after: a skeleton waiting for muscles, skin, and internal organs. EuroIntervention. 2010;6:549-53. ]. The modified ACEF score was used instead of the ACEF score as the creatinine clearance had previously been demonstrated potentially to allow for a more accurate assessment of the underlying renal function, and it had subsequently improved the accuracy of cardiac prediction models such as the EuroSCORE in CABG patients [102102. Walter J, Mortasawi A, Arnrich B, Albert A, Frerichs I, Rosendahl U, Ennker J. Creatinine clearance versus serum creatinine as a risk factor in cardiac surgery. BMC surgery 2003;3:4. , 103103. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31-41. , 104104. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, Serruys PW. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv. 2010;3:317-26. ]. The modified ACEF score is calculated by using the formula: age/ejection fraction+1 point for every 10 ml/min reduction in creatinine clearance below 60 ml/min/1.73m2 (up to a maximum of 6 points).
Within the ARTS II population, treated with SES for multivessel (two or three vessel) coronary artery disease, it was demonstrated that the clinical SYNTAX Score was more predictive of MACCE and death at 5 years compared to the SYNTAX Score or modified ACEF scores alone [104104. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, Serruys PW. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv. 2010;3:317-26. , 105105. Serruys PW, Ong AT, Morice MC, De Bruyne B, Colombo A, Macaya C, Richardt G, Fajadet J, Hamm C, Dawkins K, O’Malley AJ, Bressers M, Donohoe D. Arterial Revascularisation Therapies Study Part II - Sirolimus-eluting stents for the treatment of patients with multivessel de novo coronary artery lesions. EuroIntervention. 2005;1:147-56. ]. Despite being potentially able to predict events more accurately in the high-risk tertile, the limiting factor of the clinical SYNTAX Score is that the risk model was unable to differentiate between the clinical events for the low and intermediate risk tertiles because of limited predictive power [104104. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, Serruys PW. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv. 2010;3:317-26. ]. Subsequently, the clinical SYNTAX Score was applied to patients undergoing ULM PCI in a registry study of similar size, where similar results were also found [9494. Capodanno D, Caggegi A, Miano M, Cincotta G, Dipasqua F, Giacchi G, Capranzano P, Ussia G, Di Salvo ME, La Manna A, Tamburino C. Global Risk Classification and Clinical SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) Score in Patients Undergoing Percutaneous or Surgical Left Main Revascularisation. J Am Coll Cardiol Intv. 2011;4:287-297. ].
Logistic Clinical SYNTAX score
The logistic clinical SYNTAX Score was devised to give patients at 1-year a more personalised risk assessment after undergoing PCI. The logistic clinical SYNTAX Score was developed from 7 contemporary coronary stent trials (LEADERS, RESOLUTE, SIRTAX, SYNTAX, ARTS II, STRATEGY and MULTI-STRATEGY in over 6,000 patients) by combining the anatomical SYNTAX Score with clinical variables using a logistic regression model, in order to ensure that all components within the score were given balanced weighting to each other. A Core Model (composed of the SYNTAX Score, age, creatinine clearance and left ventricular ejection fraction) and Extended Model (incorporating the Core Model and the best performing clinical variables) of the newly devised score demonstrated substantially increased predictive ability compared to the SYNTAX Score alone, for predicting the outcome of 1-year all-cause death (c statistics: Core Model 0.752, Extended Model 0.791, SYNTAX Score 0.660 for the SYNTAX Score) ( Figure 17 ). Within the Logistic Clinical SYNTAX Score, “SYNTAX-like” patients, i.e., with LMS (isolated or associated with 1, 2 or 3VD) or 3VD alone, were specifically accounted for. Notably, the logistic clinical SYNTAX Score demonstrated similar predictive abilities for 1-year MACE (c statistics: Core Model 0.609 Extended Model 0.618, SYNTAX Score 0.605) secondary to the SYNTAX Score alone being the predominant determinant of 1-year all-cause revascularisation. Studies applying the newly devised logistic clinical SYNTAX Score to risk stratify LMS (and 3VD) patients undergoing surgical or percutaneous revascularisation are forthcoming.
The New Risk Classification Score (NERS)
The New Risk Classification Score (NERS) [107107. Chen S-L, Chen JP, Mintz G, Xu B, Kan J, Ye F, Zhang J, Sun X, Xu Y, Jiang Q, Zhang A, Stone GW. Comparison Between the NERS (New Risk Stratification) Score and the SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) Score in Outcome Prediction for Unprotected Left Main Stenting. JACC Cardiovasc Interv. 2010;3:632-641. ] is a risk score developed to predict long-term outcomes for ULM PCI from 4 centres in China (n=260). Reflecting the long time period over which this registry was performed (approximately 10 years), the patients included had either BMS or DES implantation. The score was subsequently tested (internally validated) in a different consecutive group of patients within the same registry all treated with DES (n=337).
The NERS risk score consists of 54 variables (17 clinical, 4 procedural and 33 angiographic features). A substantially higher c-statistic was evident for the NERS compared to the SYNTAX Score (NERS: 0.89 vs. SYNTAX Score: 0.69) indicating that it had an excellent discriminatory ability. When the NERS score was separated into 2 groups of risk (high and low) and clinical outcomes were assessed, the NERS score was able to identify a high-risk population for MACE, at 30 days and at over 5 years follow-up. Furthermore, the high-risk NERS group was demonstrated to be significantly more predictive of MACE compared to the intermediate or high SYNTAX Score tertiles.
Conversely, in the low-risk NERS group, outcomes were similar to the low SYNTAX Score group, suggesting at least from this study that anatomical variables alone may be sufficient to be predictive of clinical outcomes in the low-risk group.
One of the main limitations of the NERS score is that patient comorbidity in the NERS patient population was significantly less prevalent compared to the All-Comers SYNTAX population, [2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. , 6666. Ong AT, Serruys PW, Mohr FW, Morice MC, Kappetein AP, Holmes DR, Jr., Mack MJ, van den Brand M, Morel MA, van Es GA, Kleijne J, Koglin J, Russell ME. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J. 2006;151:1194-204. ] the latter having been designed to overcome many of the limitations/selection biases inherent in small registries. Validation of the NERS risk model in a much larger 'all-Comers' population of patients is required to overcome many of these issues.
A more simplified NERS II score, consisting of 16 variables (7 clinical and 9 angiographic) variables, has recently been reported with a reported predictive accuracy similar to NERS I in a multicenter, prospective registry study in China [254254. Chen SL, Han YL, Zhang YJ et al. The anatomic- and clinical-based NERS (new risk stratification) score II to predict clinical outcomes after stenting unprotected left main coronary artery disease: results from a multicenter, prospective, registry study. JACC Cardiovasc Interv. 2013;6:1233-41. ].
Amalgamation of the additive EuroSCORE and SYNTAX score
Given that the EuroSCORE has been shown to be an independent predictor of MACE in patients undergoing surgical or percutaneous revascularisation as previously described ( Table 3 ), [9191. Min SY, Park DW, Yun SC, Kim YH, Lee JY, Kang SJ, Lee SW, Lee CW, Kim JJ, Park SW, Park SJ. Major predictors of long-term clinical outcomes after coronary Revascularisation in patients with unprotected left main coronary disease: analysis from the MAIN-COMPARE study. Circ Cardiovasc Interv. 2010;3:127-33. , 9696. Rodes-Cabau J, Deblois J, Bertrand OF, Mohammadi S, Courtis J, Larose E, Dagenais F, Dery JP, Mathieu P, Rousseau M, Barbeau G, Baillot R, Gleeton O, Perron J, Nguyen CM, Roy L, Doyle D, De Larochelliere R, Bogaty P, Voisine P. Nonrandomised comparison of coronary artery bypass surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease in octogenarians. Circulation. 2008;118:2374-81. ] the need to combine the EuroSCORE with the SYNTAX Score into one single approach has become evident [108108. Serruys P.W. Integrating lessons from recent clinical trials into practice: beyond the SYNTAX score. Presented at: Transcatheter Therapeutics Asia Pacific; April 29, 2010; Seoul, South Korea; 2010. ]. One of the main advantages of combining the EuroSCORE and the SYNTAX Score to give a “Global Risk” assessment is that the same clinical tool can potentially be used in patients during the Heart Team approach in selecting the optimal revascularisation modality for the patient. Capodanno et al demonstrated the feasibility of this approach within their registry populations using differing tertiles of the SYNTAX Score and additive EuroSCOREs that reflected their study population (Global Risk Classification, or GRC), [9393. Capodanno D, Miano M, Cincotta G, Caggegi A, Ruperto C, Bucalo R, Sanfilippo A, Capranzano P, Tamburino C. EuroSCORE refines the predictive ability of SYNTAX score in patients undergoing left main percutaneous coronary intervention. Am Heart J. 2010;159:103-9. , 9494. Capodanno D, Caggegi A, Miano M, Cincotta G, Dipasqua F, Giacchi G, Capranzano P, Ussia G, Di Salvo ME, La Manna A, Tamburino C. Global Risk Classification and Clinical SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) Score in Patients Undergoing Percutaneous or Surgical Left Main Revascularisation. J Am Coll Cardiol Intv. 2011;4:287-297. ] and demonstrated that it improved the predictive ability of the SYNTAX Score .
Subsequently, the “Global Risk” approach ( Figure 18 ) – utilising the historically accepted cut-offs for the level of risk (low, intermediate and high) for the additive EuroSCORE [33. Sianos G, Morel MA, A.P. K, Morice MC, Colombo A, Dawkins K, van den Brand M, Dyck NV, Russell ME, Mohr FW, Serruys PW. (2005 ) The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-27. The birth of the SYNTAX Score. , 6161. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-6.
The SXscore methodology and its association with clinical outcomes from the SYNTAX trial., 6262. SYNTAX score calculator: http://www.syntaxscore.com. SYNTAX working-group. Launched 19th May 2009. , 8686. Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9-13. , 8787. Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881-2. ] and the broadly accepted SYNTAX trial defined tertiles of the SYNTAX Score [33. Sianos G, Morel MA, A.P. K, Morice MC, Colombo A, Dawkins K, van den Brand M, Dyck NV, Russell ME, Mohr FW, Serruys PW. (2005 ) The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-27. The birth of the SYNTAX Score. , 6161. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-6.
The SXscore methodology and its association with clinical outcomes from the SYNTAX trial.] – has been applied to the SYNTAX population [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]. The Global Risk was shown to enhance substantially the identification of low-risk patients who could safely and efficaciously be treated with CABG or PCI compared to the SYNTAX Score alone ( Figure 19 ). Furthermore, the Global Risk demonstrated at least comparable clinical outcomes (all-cause death and MACCE) in low Global Risk (GRCLOW) patients with ULMCA disease undergoing CABG or PCI at three years, in the randomised and “All-Comers” SYNTAX population ( Figure 20 ) [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]. Based on these findings from the SYNTAX trial a simple treatment algorithm was proposed ( Figure 21 ). [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]
Further analyses indicated that high EuroSCORE patients with ULMCA disease (regardless of the SYNTAX score) appeared to gain at least a morbidity advantage (in terms of reduced MACCE) by undergoing surgical revascularisation compared to PCI. Hypotheses to explain these latter findings were proposed, and concerned the observation that CABG potentially protects the entire treated coronary vessel from future cardiac events for the lifespan of the graft, compared to PCI which would treat the individual lesion. Based on these findings from the SYNTAX trial a simple treatment algorithm was proposed ( Figure 21 ). Validation of these findings are further required in unselected registries [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ].
One of the unexpected findings from the Global Risk was that higher risk subjects (high additive EuroSCORE ≥6) in all tertiles of the SYNTAX Score (low, intermediate or high), were shown to have a potential prognostic benefit from undergoing CABG compared to PCI, irrespective of the baseline SYNTAX Score, provided an acceptable threshold of operative risk was not exceeded ( Figure 21 ). For example in the 3VD cohort of the SYNTAX Trial, subjects with a low SYNTAX Score (<23) and a high EuroSCORE (≥6) had a doubling of 3-year mortality when undergoing PCI (15.9%) compared to CABG (8.2%). Hypotheses to explain these findings included the bypass graft would potentially ‘protect’ the entire treated coronary vessel from future cardiac events for the lifespan of the graft in high risk subjects, compared to PCI which would treat the individual lesion [55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. ]. Based on these observations, it was hypothesised by the investigators that low (or high) risk subjects were potentially concealed by high (or low) risk subjects in all tertiles of the SYNTAX Score. This hypothesis is what prompted the investigators to develop a more individualized approach to decision making between CABG and PCI, and subsequently lead to the development of the SYNTAX Score II [251251. Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, Kappetein AP, Colombo A, Holmes DR Jr, Mack M, Feldman T, Morice MC, Ståhle E, Onuma Y, Morel MA, Garcia-Garcia HM, van Es GA, Dawkins KD, Mohr FW, Serruys PW. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639-50 , 252252. Farooq V, van Klaveren D, Steyerberg EW, Serruys PW. SYNTAX score II - Authors’ reply. Lancet. 2013;381:1899-900 , 279279. Farooq V, Head SJ, Kappetein AP, Serruys PW. Widening clinical applications of the SYNTAX Score. Heart. 2014;100:276-87 , 280280. Head SJ, Farooq V, Serruys PW, Kappetein AP.The SYNTAX score and its clinical implications. Heart. 2014;100:169-77 ], as detailed below.
Augmenting the anatomical SYNTAX score with clinical factors and the personalisation of decision making - The SYNTAX SCORE II
Since the anatomical SYNTAX Score was developed, limitations of this scoring system to aid decision-making between CABG and PCI became evident. Namely, the lack of clinical variables and lack of a personalised approach to decision-making. The SYNTAX Score II was designed to overcome these limitations.
The combination of the anatomical SYNTAX Score with ACEF has been shown to provide most of the prognostic information in predicting mortality after CABG (excluding the anatomical SYNTAX Score or PCI (including the anatomical SYNTAX Score.[55. Serruys PW, Farooq V, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-317: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 1: The Randomised Population. J Am Coll Cardiol. 2011;58;B87 doi:10.1016/ j.jacc. 2011.10.323.
The association between the SXscore, clinical variables and systemic atherosclerotic disease to explain the findings of the LMS (and 3VD) populations from the SYNTAX trial. Currently In Press., 66. Farooq V, Serruys PW, Vrancx P, Brugaletta S, Holmes DR, Kappetein AP, Mack M, Feldman T, Morice MC, Ståhle E, Colombo A, Pereda P, Huang J, Morel MA, Van Es GA, Dawkins KD, Mohr FW, Steyerberg EW. TCT-211: The SYNTAX trial at 3 Years: A Global Risk Approach to Identify Patients With 3-Vessel &/or Left Main Stem Disease Who Could Safely & Efficaciously Be Treated With Percutaneous Coronary Intervention Part 2: The All-Comers SYNTAX Population. J Am Coll Cardiol. 2011;58;B57 doi:10.1016/j.jacc.2011.10.215. , 100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 101101. Ranucci M, Castelvecchio S. The ACEF score one year after: a skeleton waiting for muscles, skin, and internal organs. EuroIntervention. 2010;6:549-53. , 281281. Ranucci M, Castelvecchio S, Conte M et al. The easier, the better: age, creatinine, ejection fraction score for operative mortality risk stratification in a series of 29,659 patients undergoing elective cardiac surgery. J Thorac Cardiovasc Surg. 2011;142:581-6. , 282282. Serruys PW, Farooq V, Vranckx P et al. A global risk approach to identify patients with left main or 3-vessel disease who could safely and efficaciously be treated with percutaneous coronary intervention: the SYNTAX Trial at 3 years. JACC Cardiovasc Interv. 2012;5:606-17. , 283283. Farooq V, Vergouwe Y, Raber L et al. Combined anatomical and clinical factors for the long-term risk stratification of patients undergoing percutaneous coronary intervention: the Logistic Clinical SYNTAX score. Eur Heart J. 2012;33:3098-104. , 284284. Farooq V, Vergouwe Y, Généreux P, Bourantas CV, Palmerini T, Caixeta A, Garcìa-Garcìa HM, Diletti R, Morel MA, McAndrew TC, Kappetein AP, Valgimigli M, Windecker S, Dawkins KD, Steyerberg EW, Serruys PW, Stone GW. Prediction of 1-year mortality in patients with acute coronary syndromes undergoing percutaneous coronary intervention: validation of the logistic clinical SYNTAX (Synergy Between Percutaneous Coronary Interventions With Taxus and Cardiac Surgery) score. JACC Cardiovasc Interv. 2013;6:737-45 ]
As previously descried, Ranucci et al first demonstrated in a relatively simple risk model ( Figure e4 ) consisting of only three clinical variables, namely age, preoperative serum creatinine value and left ventricular ejection fraction, a risk model for assessing operative mortality risk in elective cardiac operations. Based on the “law of parsimony” or “the Ockham razor” concept, whereby a simple model can explain a phenomenon with the same level of accuracy as complex models, ACEF was shown to be least comparable to the EuroSCORE (composed of 17 variables) in predicting in-hospital mortality after CABG. [100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 101101. Ranucci M, Castelvecchio S. The ACEF score one year after: a skeleton waiting for muscles, skin, and internal organs. EuroIntervention. 2010;6:549-53. ] The three risk factors used in ACEF are natural continuous variables that are objectively defined, and not subject to personal estimation (e.g. is the patient diabetic? does the patient have extra cardiac arteriopathy?). In addition, the variables of ACEF were known independent risk factors for mortality and it was subsequently shown that the end organ manifestations of the risk factor (as identified in ACEF) were more important for predicting long-term prognosis, rather than the actual presence of the risk factor. [100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 255255. Farooq V, Serruys PW, Bourantas C et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur Heart J. 2012;33:3105-13. , 256256. Tonelli M, Muntner P, Lloyd A et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380:807-14. , 257257. Fox CS, Matsushita K, Woodward M et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet. 2012;380:1662-73. ]
The SYNTAX score II [100100. Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation. 2009;119:3053-61. , 101101. Ranucci M, Castelvecchio S. The ACEF score one year after: a skeleton waiting for muscles, skin, and internal organs. EuroIntervention. 2010;6:549-53. ] augments the purely anatomical SYNTAX score with anatomical and clinical factors that were shown to alter the threshold value of the anatomical SYNTAX Score in order for equipoise to be achieved between CABG and PCI for long-term mortality. This was achieved through building the SYNTAX Score II on the ACEF ‘skeleton,’ with the addition of risk factors that were shown to directly affect decision making between CABG and PCI through interaction effects; i.e. a risk factor being more predictive of mortality in patients undergoing PCI compared to CABG, or vice versa ( Figure e5 ). For example, the anatomical SYNTAX Score aids decision-making between CABG and PCI because it is more predictive of clinical outcomes in patients undergoing PCI, compared to patients undergoing CABG (where it is not predictive). Based on this principle, younger age, female gender and reduced LVEF favored CABG compared to PCI on long-term prognostic grounds ( Figure e6 ). Thus, in such patients a LOWER anatomical SYNTAX Score would be required in order for the long-term mortality risk to be similar between CABG and PCI. By contrast, older age, chronic obstructive pulmonary disease or ULMCA disease favored PCI compared to CABG ( Figure e6 ) and thus, in this type of patient, a HIGHER anatomical SYNTAX Score would be needed for the long-term mortality risks to be similar.
By adopting the individualized approach of the SYNTAX Score II, augmented by clinical variables, it was shown that subsets of patients existed in all tertiles of the SYNTAX Score in which CABG or PCI would confer a mortality benefit, or offer similar long term prognosis (Fig. e7). A nomogram was developed (Fig. e8) that allowed for an accurate individualized prediction of 4-year mortality in patients proposing to undergo CABG or PCI, to objectively aid decision making. For example, a 60 year old male with an anatomical SYNTAX Score of 30, ULMCA disease, CrCl 60 ml/min, a LVEF of 50%, and COPD, would have 41 points (predicted 4-year mortality: 16·3%) and 33 points (predicted 4-year mortality: 8·7%) to undergo CABG and PCI respectively. The same example, without COPD included, would lead to identical points (29 points) and identical 4-year mortality predictions (6.3%) for CABG and PCI. An online version of the SYNTAX Score II will soon appear alongside the original SYNTAX Score calculator (www.syntaxscore.com).
Notably, diabetes was not included in the final SYNTAX Score II, despite medically treated diabetes being pre-stratified at randomization as a powered subgroup in the SYNTAX Trial, and present in over a quarter of the study patients (26%). This in spite of diabetes being perceived as a specific high risk group potentially warranting a differing treatment strategy compared to other risk factors. [3232. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
2011 American Revascularisation Guidelines – a further essential read! Notably the recommendations to support ULM PCI in selected patients was increased from Class IIB in the 2009 guidelines to Class IIA in the present guidelines., 109109. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM, Jr., Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e123-210. , 246246. 246. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541-619 , 258258. Farkouh ME, Domanski M, Sleeper LA et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375-84. ]The primary reason was that diabetes was shown not to be important for decision-making between CABG and PCI, since it lacked an interaction effect, i.e. was equally predictive of mortality in the CABG and PCI arms after adjustment for other risk factors (Fig. e5). As previously discussed in ACEF, the end organ manifestations of diabetes are what affected long term mortality in CABG and PCI populations. The findings of the lack of inclusion of diabetes in the SYNTAX Score II are supported by epidemiological data, in which non-diabetics with chronic kidney disease and proteinuria had a stronger association with the risk of MI, and a higher rate of mortality, compared to diabetics, and that the relative risk of long-term mortality associated with chronic kidney disease was “much the same irrespective of the presence or absence of diabetes.” [256256. Tonelli M, Muntner P, Lloyd A et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380:807-14. , 257257. Fox CS, Matsushita K, Woodward M et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet. 2012;380:1662-73. ] Also worthy of mentioning is a recent study, comprising 3280 patients with both LM disease and three-vessel disease randomised to undergo PCI or CABG in a pooled analysis of the BEST, PRECOMBAT and SYNTAX trials. In that work, investigators tested the impact of both anatomical SYNTAX score and SYNTAX score II on 5 year outcomes in patients with diabetes. Mainly, their findings were that differences in 5 year outcomes following PCI and CABG for patients with MVD and diabetes were influenced by anatomical complexity as measured by the anatomical SYNTAX score. The SYNTAX score II mortality prediction model showed similar performance regardless of the diabetes status. [299299. Cavalcante R, Sotomi Y, Mancone M, Whan Lee C, Ahn JM, Onuma Y, Lemos PA, van Geuns RJ, Park SJ, Serruys PW. Impact of the SYNTAX scores I and II in patients with diabetes and multivessel coronary disease: a pooled analysis of patient level data from the SYNTAX, PRECOMBAT, and BEST trials. Eur Heart J. 2017;38:1969-1977. ]
Validation of the SYNTAX Score II
As compared to existing revascularisation guidelines using the anatomical SYNTAX Score, [3232. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
2011 American Revascularisation Guidelines – a further essential read! Notably the recommendations to support ULM PCI in selected patients was increased from Class IIB in the 2009 guidelines to Class IIA in the present guidelines., 109109. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM, Jr., Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e123-210. , 246246. 246. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541-619 ] it was shown that if CABG or PCI was selected based on a higher or lower expected survival (irrespective of the margin of difference) with the SYNTAX Score II in the SYNTAX Trial, the SYNTAX Score II would only need to be used in 110 patients to have one more patient alive at 4 years. [252252. Farooq V, van Klaveren D, Steyerberg EW, Serruys PW. SYNTAX score II - Authors’ reply. Lancet. 2013;381:1899-900 ] External validation of the SYNTAX Score II was performed in the multinational Drug Eluting stent for Left main coronary Artery disease (DELTA) Registry (14 centres in Europe, US and South Korea), [251251. Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, Kappetein AP, Colombo A, Holmes DR Jr, Mack M, Feldman T, Morice MC, Ståhle E, Onuma Y, Morel MA, Garcia-Garcia HM, van Es GA, Dawkins KD, Mohr FW, Serruys PW. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639-50 ] composed of subjects with ULMCA disease associated with or without multivessel disease (26% of the study population had 3VD). All variables in the SYNTAX Score II interacted in a similar way, and therefore influenced decision making between CABG and PCI, in the SYNTAX Trial and DELTA Registry, with the exception of age and LVEF, which had minimal interactions in the DELTA Registry. Findings which may relate to the unavoidable selection bias inherent to all registries, since decision making between CABG and PCI has already been made and would be difficult to control for. [259259. Farooq V, Serruys PW. Observations from the CREDO-Kyoto three-vessel disease registry: can one adjust for the unadjustable? EuroIntervention. 2013;9:419-21 ] Further retrospective validation of the SYNTAX Score II has recently been undertaken in 3,896 patients with 3-vessel and/or ULMCA disease undergoing PCI (n=2,190) or CABG (n=1,796) from the Japanese Coronary REvascularization Demonstrating Outcome Study in Kyoto (CREDO-Kyoto) PCI/CABG multicenter registry.[261261. Campos CM, van Klaveren D, Iqbal J et al. Predictive Performance of SYNTAX Score II in Patients With Left Main and Multivessel Coronary Artery Disease. Circ J. 2014;78:1942-9. ]
Prospective validation of the SYNTAX Score II in EXCEL
Prospective validation of the SYNTAX Score II is currently occurring in the international multicenter EXCEL Trial (Evaluation of XIENCE PRIME™ or XIENCE V® Everolimus Eluting Stent System Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) Trial (ClinicalTrials.gov Identifier: NCT01205776), having recently completely recruitment of patients. EXCEL recruited 1905 patients with ULMCA disease and a investigator reported SYNTAX Scores <33, randomised to CABG (n=957) or PCI with contemporary stents (n=948). The Primary Endpoint is a composite measure of all-cause death, MI, or stroke at 3 years post revascularisation. As part of the prospective validation of the SYNTAX Score II, the SYNTAX Score II was used to forecast and compare 4-year mortality in the PCI and CABG arms of EXCEL[260260. Campos CM, van Klaveren D, Farooq V, Simonton CA, Kappetein AP, Sabik JF 3rd, Steyerberg EW, Stone GW, Serruys PW; On Behalf of the EXCEL Trial Investigators. Long-term forecasting and comparison of mortality in the Evaluation of the Xience Everolimus Eluting Stent vs. Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial: prospective validation of the SYNTAX Score II. Eur Heart J. 2015. [Epub ahead of print] ]. Within EXCEL, the SYNTAX Score II indicated at least an equipoise for long-term mortality between CABG and PCI in subjects with ULMCA disease up to an intermediate anatomical complexity (SYNTAX Score <33, with a predicted 77.9% chance of a lower 4-year mortality in the PCI arm of the EXCEL trial, and a 40% chance that this will achieve statistical significance in favour of PCI ( Figure e9 ). Specifically, the 4-year predicted mortalities were 8.5 and 10.5% in the PCI and CABG arms respectively [odds ratios (OR) 0.79; 95% PI 0.43–1.50). As expected, anatomical complexity (modified by clinical factors) were shown to affect predicted mortality, namely, that in subjects with low (≤22) anatomical SYNTAX scores, the predicted OR was 0.69 (95% PI 0.34–1.45) and in intermediate anatomical SYNTAX scores [24730,24731,24732,24733,24734,24735,24736,24737,24738,24739], the predicted OR was 0.93 (95% PI 0.53–1.62).
International guidelines
EUROPEAN SOCIETY OF CARDIOLOGY (ESC) AND THE EUROPEAN ASSOCIATION FOR CARDIO-THORACIC SURGERY (EACTS) GUIDELINES
“Significant LM stenosis and significant proximal LAD disease, especially in the presence of multivessel coronary artery disease, are strong indications for revascularisation. In the most severe patterns of coronary artery disease, CABG appears to offer a survival advantage as well as a marked reduction in the need for repeat revascularisation, albeit at a higher risk of CVA, especially in LM disease”[3131. Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D, Vahanian A, Auricchio A, Bax J, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearney P, McDonagh T, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas PE, Widimsky P, Alfieri O, Dunning J, Elia S, Kappetein P, Lockowandt U, Sarris G, Vouhe P, von Segesser L, Agewall S, Aladashvili A, Alexopoulos D, Antunes MJ, Atalar E, Brutel de la Riviere A, Doganov A, Eha J, Fajadet J, Ferreira R, Garot J, Halcox J, Hasin Y, Janssens S, Kervinen K, Laufer G, Legrand V, Nashef SA, Neumann FJ, Niemela K, Nihoyannopoulos P, Noc M, Piek JJ, Pirk J, Rozenman Y, Sabate M, Starc R, Thielmann M, Wheatley DJ, Windecker S, Zembala M. Guidelines on myocardial Revascularisation: The Task Force on Myocardial Revascularisation of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501-55.
European Revascularisation Guidelines – an essential read!].
( Table 4 and Table 5 ) forms the basis of recommendations ( Table e3a and Table e3b ) by the Heart Team in informing patients and guiding the approach to informed consent.The presence of an ostial and/or shaft lesion is considered as a Class IIa indication for PCI, level of evidence B. A distal isolated LM lesion, or being associated with single-vessel disease, is considered as a Class IIb indication. Left main lesion associated with two-vessel or three-vessel disease and a low or intermediate SYNTAX Score is considered as a Class IIb indication. Left main lesion associated with two-vessel or three-vessel disease and a high SYNTAX Score is considered as a Class III indication.
SYNTAX Score II
Currently the ESC/EACTS Guidelines on myocardial revascularization give the SYNTAX Score II a recommendation of IIa (weight of evidence/opinion is in favour of usefulness/efficacy – should be considered), level of evidence B, to aid in decision making between CABG and PCI in patients with complex coronary artery disease [246246. 246. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541-619 ].
AMERICAN COLLEGE OF CARDIOLOGY (ACC)/AMERICAN HEART ASSOCIATION (AHA)/ SOCIETY FOR CARDIOVASCULAR ANGIOGRAPHY AND INTERVENTIONS (SCAI) GUIDELINES
The 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery both support the consideration of ULM PCI in patients with anatomical conditions that are associated with a low risk of PCI procedural complications and a high likelihood of good long-term outcome. Notably, the guidelines also suggested the use of a low SYNTAX Score to aid in this process ( Table 6 ) [3232. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
2011 American Revascularisation Guidelines – a further essential read! Notably the recommendations to support ULM PCI in selected patients was increased from Class IIB in the 2009 guidelines to Class IIA in the present guidelines., 109109. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM, Jr., Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e123-210. ]. In addition, clinical characteristics that predict a significantly increased risk of adverse surgical outcomes were also suggested. Furthermore, the US guidelines now give surgical revascularisation for unprotected left main coronary disease a class 1B recommendation, [3232. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
2011 American Revascularisation Guidelines – a further essential read! Notably the recommendations to support ULM PCI in selected patients was increased from Class IIB in the 2009 guidelines to Class IIA in the present guidelines., 109109. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM, Jr., Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e123-210. ]. compared to a class 1A recommendation in previous guidelines [110110. Kushner FG, Hand M, Smith SC, Jr., King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr., Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205-41. , 111111. Kushner FG, Hand M, Smith SC, Jr., King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr., Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271-306. ].
Coronary imaging/adjunctive coronary devices
QUANTITATIVE CORONARY ANGIOGRAPHY (QCA)
Of all the coronary segments, the LMS has the greatest angiographic variability, a concept that was first proved by Fisher et al in the Coronary Artery Surgery Study (CASS) study in 1982 [112112. Fisher LD, Judkins MP, Lesperance J, Cameron A, Swaye P, Ryan T, Maynard C, Bourassa M, Kennedy JW, Gosselin A, Kemp H, Faxon D, Wexler L, Davis KB. Reproducibility of coronary arteriographic reading in the coronary artery surgery study (CASS). Catheter Cardiovasc Interv. 1982;8:565-75. ]. Abizaid et al [113113. Abizaid AS, Mintz GS, Abizaid A, Mehran R, Lansky AJ, Pichard AD, Satler LF, Wu H, Kent KM, Leon MB. One-year follow-up after intravascular ultrasound assessment of moderate left main coronary artery disease in patients with ambiguous angiograms. J Am Coll Cardiol. 1999;34:707-15. ] in 1999 demonstrated in 122 patients with moderate LMS disease that ( Figure 22 ):
- the QCA reference diameter (3.91 ± 0.76 mm, mean ± 1 SD) moderately correlated with the IVUS reference diameter (4.25 ± 0.78 mm, r=0.492, p=0.0001);
- the QCA-derived minimum lumen diameter (MLD) (2.26 ± 0.82 mm) at the lesion site correlated less well with IVUS (2.81 ± 0.82 mm, r=0.364, p=0.0005);
- the QCA-derived diameter stenosis (DS) (42 ± 16%) did not correlate with IVUS (35 ± 15%) (r=0.106).
Risk Stratification
- The SYNTAX Score has proven to be a clinically useful anatomical scoring system to aid decision making for the optimal revascularisation modality in patients with ULMCA disease
- A low to moderate SYNTAX Score (<33) in patients with ULMCA disease has been shown to have similar outcomes in terms of efficacy and safety in the SYNTAX trial at up to 5 years in patients undergoing surgical or percutaneous revascularisation. This has been validated in several registries at short and longer-term follow-up, and is now subject to the ongoing EXCEL trial
- The outcomes of patients undergoing ULM PCI appears to be affected by a higher SYNTAX Score and its association with anatomical complexities and clinical comorbidity
- Within the general population a higher SYNTAX Score has been associated with markers of systemic atherosclerosis (higher carotid intima-media thickness, ankle-brachial pressure index)
- The “Functional SYNTAX Score” (a fractional flow reserve-derived SYNTAX Score) may improve decision making in patients with ULMCA disease. Further study is on-going
- Clinical based scores, such as the Parsonnet score and EuroSCORE, or clinical variables per se have been shown to improve the predictive ability of the SYNTAX Score in patients with ULMCA disease. No clear consensus currently exists on the most appropriate combined anatomical and clinical based score
- The European and American Revascularisation guidelines regard ULM PCI as a Class IIa indication in appropriately selected patients with suitable anatomical conditions. Both guidelines suggest the use of the SYNTAX Score in guiding decision making
- The SYNTAX Score II augments the purely anatomical SYNTAX score with anatomical and clinical factors that were shown to alter the threshold value of the anatomical SYNTAX Score in order for equipoise to be achieved between CABG and PCI for long-term mortality.
By adopting the individualized approach of the SYNTAX Score II, augmented by clinical variables, it was shown that subsets of patients existed in all tertiles of the SYNTAX Score in which CABG or PCI would confer a mortality benefit, or offer similar long term prognosis. The European Revascularisation guidelines regard use of the SYNTAX Score II as a class IIa indication (level of evidence B).
INTRAVASCULAR ULTRASOUND (AND MULTISLICE COMPUTED TOMOGRAPHY)
Intravascular ultrasound (IVUS) is a particularly useful technique in imaging the LMS before, during and after intervention. Recently, the new consensus statement from European Bifurcation Club (EBC) have published and endorsed the use of IVUS during most of LM interventions [290290. Mintz GS, Lefèvre T, Lassen JF, Testa L, Pan M, Singh J, Stankovic G, Banning AP. Intravascular ultrasound in the evaluation and treatment of left main coronary artery disease: a consensus statement from the European Bifurcation Club. EuroIntervention. 2018;14:e467-e474. ].
Pre-implantation IVUS
IVUS imaging provides a high tissue penetration that allows for a visualisation of the entire vessel wall and thus the assessment of vessel remodelling and total atheroma burden. The applications of IVUS pre intervention most importantly includes the identification of LMS lesions that would benefit from undergoing revascularisation, the characterisation of plaque morphology and plaque distribution which may subsequently influence the decision-making process with regard to lesion preparation, and allowing for adequate stent diameter and length sizing.
With respect to the identification of LMS lesions that would benefit from undergoing revascularisation, the cut-off values of the IVUS-derived parameters were first determined by Jasti et al [114114. Jasti V, Ivan E, Yalamanchili V, Wongpraparut N, Leesar MA. Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation. 2004;110:2831-6.
A study that first determined the optimum cut off for the IVUS derived MLA in the LMS – in terms of the need for revascularisation – compared to FFR.]. In a study of 55 patients with angiographically ambiguous LMS lesions, the IVUS-derived LMS minimum lumen diameter (MLD) and minimum lumen area (MLA) were found to be strongly correlated with FFR haemodynamic measurements. The cut-off values of the IVUS parameters were thus determined by the corresponding FFR measurements, with an FFR of 0.75 used as a measurement of the haemodynamic significance of a LMS lesion ( Figure 23 ). An IVUS-derived MLA and MLD of 5.9 mm2 (sensitivity 93%, specificity 95%) and 2.8 mm (sensitivity 93%, specificity 98%) respectively were shown to be strongly predictive of the physiological significance of a LMS lesion. In addition, a MLA value <6.0 mm2 has since been prospectively validated in the multicentre LITRO study [115115. De la Torre Hernandez JM, Hernandez Hernandez F, Alfonso F, Rumoroso JR, Lopez-Palop R, Sadaba M, Carrillo P, Rondan J, Lozano I, Ruiz Nodar JM, Baz JA, Fernandez Nofrerias E, Pajin F, Garcia Camarero T, Gutierrez H. Prospective application of pre-defined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions results from the multicenter LITRO study. J Am Coll Cardiol. 2011;58:351-8. ] recruiting patients with intermediate left main stenoses (n=354): a MLA value ≥6.0 mm2 identified patients at low risk for adverse events who could safely be candidates for deferred revascularisation.
Conversely, Kang et al [116116. Kang SJ, Lee JY, Ahn JM, Song HG, Kim WJ, Park DW, Yun SC, Lee SW, Kim YH, Mintz GS, Lee CW, Park SW, Park SJ. Intravascular ultrasound-derived predictors for fractional flow reserve in intermediate left main disease. JACC Cardiovasc Interv. 2011;4:1168-74. ] recently demonstrated in a study of 55 patients with isolated LMS disease that an IVUS-derived MLA of 4.8 mm2 best predicted a FFR <0.80 (89% sensitivity, 83% specificity) and <4.1 mm2 (95% sensitivity, 83% specificity) for predicting FFR <0.75. Furthermore, Park et al demonstrated in a study of 112 patients with isolated ostial and shaft intermediate LMCA stenosis (angiographic diameter stenosis of 30% to 80%) that an IVUS-derived MLA of ≤4.5 mm2 to be a useful index of an FFR of ≤0.80 (77% sensitivity, 82% specificity, 84% positive predictive value, 75% negative predictive value, area under the curve: 0.83, 95% CI: 0.76 to 0.96) [262262. Park SJ, Ahn JM, Kang SJ, Yoon SH, Koo BK, Lee JY, Kim WJ, Park DW, Lee SW, Kim YH, Lee CW, Park SW. Intravascular ultrasound-derived minimal lumen area criteria for functionally significant left main coronary artery stenosis. JACC Cardiovasc Interv. 2014 Aug;7:868-74. ]. Notably, a FFR >0.80 was evident in 10/58 (17.2%) lesions with an MLA of ≤4.5 mm2 (“mismatch”), and 13/54 (24.1%) lesions with an MLA of >4.5 mm2 (“reverse mismatch”) ( Figure e10 ). Adjustment for the body surface area, body mass index, and left ventricular mass was not shown to improve the diagnostic accuracy of the IVUS MLA.
Given the above discrepancies it has recently been proposed that a FFR or non-invasive stress testing should be performed if the IVUS-derived MLA is <6.0 mm2 pre-intervention [117117. McDaniel MC, Eshtehardi P, Sawaya FJ, Douglas JS, Jr., Samady H. Contemporary clinical applications of coronary intravascular ultrasound. JACC Cardiovasc Interv. 2011;4:1155-67. ].
Post-implantation IVUS
Post-implantation IVUS allows for the assessment of stent expansion, stent apposition, and side-branch (SideB) compromise, and for the presence of coronary dissections. To date, no single randomised controlled trial (RCT) has observed superiority in terms of clinical outcome with an IVUS-guided PCI strategy for the left main or the coronary tree [118118. Jakabcin J, Spacek R, Bystron M, Kvasnak M, Jager J, Veselka J, Kala P, Cervinka P. Long-term health outcome and mortality evaluation after invasive coronary treatment using drug eluting stents with or without the IVUS guidance. Randomised control trial. HOME DES IVUS. Catheter Cardiovasc Interv. 2010;75:578-83. , 119119. Colombo A. AVIO: a prospective randomised trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions. Presented at: Transcatheter Cardiovascular Therapeutics; September 21 to 25, 2010; Washington, DC. ]. Evidence from registries has, however, suggested that the IVUS-guided approach may lead to clinical benefit with ULM PCI as detailed [120120. Park SJ, Kim YH, Park DW, Lee SW, Kim WJ, Suh J, Yun SC, Lee CW, Hong MK, Lee JH, Park SW. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009;2:167-77.
A propensity matched study demonstrating the longer term (2 year) mortality benefit of an IVUS guided ULM PCI approach compared to an angiographic approach., 121121. Kang SJ, Ahn JM, Song H, Kim WJ, Lee JY, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Mintz GS, Park SW, Park SJ. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv. 2011;4:562-9.
A study that elegantly demonstrated IVUS predictors of angiographic restenosis post ULM PCI within the LMS and its side branches.].
In non-LMS lesions, larger propensity-matched studies have potentially associated IVUS-guided PCI with DES to improved clinical outcomes, compared to an angiographically-guided strategy [122122. Claessen BE, Mehran R, Mintz GS, Weisz G, Leon MB, Dogan O, de Ribamar Costa J, Jr., Stone GW, Apostolidou I, Morales A, Chantziara V, Syros G, Sanidas E, Xu K, Tijssen JG, Henriques JP, Piek JJ, Moses JW, Maehara A, Dangas GD. Impact of intravascular ultrasound imaging on early and late clinical outcomes following percutaneous coronary intervention with drug-eluting stents. JACC Cardiovasc Interv. 2011;4:974-81. , 123123. Roy P, Steinberg DH, Sushinsky SJ, Okabe T, Pinto Slottow TL, Kaneshige K, Xue Z, Satler LF, Kent KM, Suddath WO, Pichard AD, Weissman NJ, Lindsay J, Waksman R. The potential clinical utility of intravascular ultrasound guidance in patients undergoing percutaneous coronary intervention with drug-eluting stents. Eur Heart J. 2008;29:1851-7. ]. Within the LMS, Park et al demonstrated in the MAIN-COMPARE registry of 145 propensity-matched pairs of patients with ULMCA disease implanted with DES that IVUS guidance led to a substantial long-term (3-year) mortality benefit compared to conventional angiography guidance ( Figure 24 ) [120120. Park SJ, Kim YH, Park DW, Lee SW, Kim WJ, Suh J, Yun SC, Lee CW, Hong MK, Lee JH, Park SW. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009;2:167-77.
A propensity matched study demonstrating the longer term (2 year) mortality benefit of an IVUS guided ULM PCI approach compared to an angiographic approach.].
Colombo et al have previously advocated a stent area not inferior to 70% of area of the media to media (vessel size) at the ostium of the SideB in non-left main bifurcation lesions [124124. Colombo A. Innovations in bifurcations. Catheter Cardiovasc Interv 2008;71:E7-8. ]. Within the context of the left main, Kang et al demonstrated the IVUS predictors of angiographic restenosis in ULM PCI implanted with SES in a single-site observational study [121121. Kang SJ, Ahn JM, Song H, Kim WJ, Lee JY, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Mintz GS, Park SW, Park SJ. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv. 2011;4:562-9.
A study that elegantly demonstrated IVUS predictors of angiographic restenosis post ULM PCI within the LMS and its side branches.]. Within this study (n=403), 13% of patients undergoing PCI had ostial/midshaft lesions and 87% bifurcation lesions. Two thirds of the bifurcation lesions were treated with a 1-stent strategy, and one third with a 2-stent strategy (crush or T-stent). The criteria for post-stent-implantation minimal stent areas (MSA) were determined to be <8.2 mm2 in the proximal LMS, <7.2 mm2 in the polygon of confluence (POC [125125. Kang SJ, Mintz GS, Oh JH, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Intravascular ultrasound assessment of distal left main bifurcation disease: The importance of the polygon of confluence of the left main, left anterior descending, and left circumflex arteries. Catheter Cardiovasc Interv. 2011 Jul 29. [Epub ahead of print]. ]), <6.3 mm2 in the ostial LAD, and <5.0 mm2 in the ostial LCx ( Figure 25 ). By utilising these MSA cut-off criteria, over one third (133 patients, 33.8%) of the study population were demonstrated to have stent underexpansion of at least 1 stent segment. Nine-month angiographic outcomes demonstrated ISR (at any location) more frequently in lesions with stent “underexpansion” of at least 1 segment compared to lesions with “adequate expansion” of the stent (24.1% versus 5.4%, p<0.001). Importantly, these findings were correlated to 2-year clinical outcomes, with freedom from MACE being significantly higher in patients with adequate stent expansion compared to stent underexpansion ( Figure 26 ). Validation of this concept in other populations is required.
Tips and tricks in performing IVUS in the left main
- JL4 guiding catheters are usually recommended to prevent deep intubation of the LMS.
- Coaxial positioning of the guide catheter tip is essential to allow appropriate visualisation of all layers of the vessel wall, in particular LMS with a large diameter.
- Decannulation of the guide catheter from the LMS is usually required to allow for appropriate imaging of the LMS ostium.
- An automatic pullback of 0.5 mm/s is generally adopted; faster pullbacks may be required (1.0 mm/s) in a very long LMS to limit procedural time and potential ischaemia.
- In cases of tight lesions, the IVUS probe may potentially occlude the LMS and cause ischaemia/haemodynamic instability - predilatation with a small diameter balloon prior to IVUS examination may be necessary.
- Ensure the image depth is increased to the maximum prior to undertaking IVUS due to the large size of the LMS.
- For LMS bifurcation analyses:
ensure the LAD and LCx have a coronary wire passed. This will potentially allow for the appropriate visualisation of the carina/ostia (by reducing the bifurcation angle) as it would appear after implantation with a metallic stent; furthermore the coronary wires can act as a point of reference for the LAD and LCx vessels when analysing the pull-backs.
LCx ostial measurements cannot be reliably assessed obliquely from the LAD to LMS on IVUS pullback. When performed this way the LCx ostial measurements are only moderately reliable, consequently the evaluation of the LCx ostium by direct LCx pullback is recommended [126126. Oviedo C, Maehara A, Mintz GS, Tsujita K, Kubo T, Doi H, Castellanos C, Lansky AJ, Mehran R, Dangas G, Leon MB, Stone GW, Templin B, Araki H, Ochiai M, Moses JW. Is accurate intravascular ultrasound evaluation of the left circumflex ostium from a left anterior descending to left main pullback possible? Am J Cardiol. 2010;105:948-54. ].
MULTISLICE COMPUTED TOMOGRAPHY
In the era when routine surveillance coronary angiography was recommended after ULM PCI with DES as previously discussed, van Mieghem et al [127127. Van Mieghem CA, Cademartiri F, Mollet NR, Malagutti P, Valgimigli M, Meijboom WB, Pugliese F, McFadden EP, Ligthart J, Runza G, Bruining N, Smits PC, Regar E, van der Giessen WJ, Sianos G, van Domburg R, de Jaegere P, Krestin GP, Serruys PW, de Feyter PJ. Multislice spiral computed tomography for the evaluation of stent patency after left main coronary artery stenting: a comparison with conventional coronary angiography and intravascular ultrasound. Circulation. 2006;114:645-53. ] demonstrated the feasibility of fulfilling this role non-invasively with the use of cardiac multislice computed tomography (MSCT). In the 70 patients prospectively studied, MSCT correctly identified all patients with ISR (10 of 70), but misclassified 5 patients without ISR (false-positives). Overall, the accuracy of MSCT for detection of angiographic ISR was 93%. The sensitivity, specificity, and positive and negative predictive values were 100%, 91%, 67%, and 100%, respectively. Furthermore, MSCT demonstrated a good correlation with IVUS for stent area (r=0.73) and an IVUS threshold value of ≥1 mm was shown to detect in-stent neointimal hyperplasia with MSCT reliably. In addition, in a comparative study with IVUS/IVUS-VH, MSCT has been shown potentially both to identify and to quantify calcium (as illustrated in ( Figure 27 ) [128128. Pundziute G, Schuijf JD, Jukema JW, Decramer I, Sarno G, Vanhoenacker PK, Reiber JH, Schalij MJ, Wijns W, Bax JJ. Head-to-head comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv. 2008;1:176-82. ].
QCA/IVUS/MSCT
- Of all the coronary segments the LMS has the greatest angiographic variability
- IVUS is superior to QCA in terms of assessing reference diameter, MLD and diameter stenosis of the LMS
- IVUS provides a high tissue penetration that allows for a visualisation of the entire vessel wall and thus the assessment of vessel remodelling and total atheroma burden
- To date, no single RCT has observed superiority in terms of clinical outcome with an IVUS-guided PCI strategy. One propensity-matched study has suggested a substantial long-term (3-year) mortality benefit for this approach compared to conventional angiography
- In angiographically ambiguous LMS lesions, an IVUS-derived MLA cut-off of 5.9 mm2 has been associated with an FFR of 0.75
- Due to the discrepancies in the best IVUS MLA cut-off that correlates with FFR, the undertaking of FFR or non-invasive stress testing has been suggested if the IVUS derived MLA is <6.0 mm2 pre-intervention. Revascularisation can be safely deferred if the MLA value ≥6.0 mm2
- The criteria for the minimum stent areas (MSA) post ULM PCI have been shown to be approximately 8 mm2, 7 mm2, 6 mm2 and 5 mm2 in the proximal LMS, polygon of confluence, ostial LAD, and ostial LCx, respectively These cut-off values have been associated with reduced ISR at 9 months and freedom from MACE at 2 years
- LCx ostial measurements cannot be reliably assessed obliquely from the LAD to LMS on IVUS pullback. Evaluation of the LAD and LCx ostia is recommended by the pull-back in the respective vessels
- If clinically indicated, MSCT can allow for reliable non-invasive evaluation after LMCA stenting and can safely exclude significant left main in stent restenosis
FRACTIONAL FLOW RESERVE
Principles of FFR in the left main
Fractional flow reserve (FFR) is a physiological parameter that reflects both the severity of epicardial stenosis and the amount of myocardium supplied. FFR is defined as the ratio of maximal hyperaemic myocardial blood flow through a stenotic artery to the theoretical maximal hyperaemic myocardial blood flow in the absence of stenosis. FFR is calculated by measuring distal mean coronary and aortic pressures during maximal hyperaemia with a 0.014-inch pressure-sensor angioplasty guidewire - thereby reflecting the influence of a coronary stenosis on maximal perfusion of the subtended myocardium [129129. Park SJ, Ahn JM, Kang SJ. Paradigm shift to functional angioplasty: new insights for fractional flow reserve- and intravascular ultrasound-guided percutaneous coronary intervention. Circulation. 2011;124:951-7.
An essential read to understand the concept of Functional Angioplasty.].
The FAME (Fractional flow reserve versus Angiography for Multivessel Evaluation) study demonstrated that treatment decisions based on systematic assessment of FFR improved clinical outcomes in patients with coronary artery disease [7575. Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, Maccarthy PA, Van’t Veer M, Pijls NH. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816-21. , 7676. Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, van’t Veer M, Klauss V, Manoharan G, Engstrom T, Oldroyd KG, Ver Lee PN, MacCarthy PA, De Bruyne B. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol. 2010;56:177-84. , 130130. Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’t Veer M, Klauss V, Manoharan G, Engstrom T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-24. ]. Consequently, the use of FFR has been incorporated into the current PCI guidelines for patients with coronary artery disease (US guidelines: recommendation IIa, level of evidence A; European guidelines: recommendation I, level of evidence A for FFR without objective evidence of ischaemia) [3131. Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D, Vahanian A, Auricchio A, Bax J, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearney P, McDonagh T, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas PE, Widimsky P, Alfieri O, Dunning J, Elia S, Kappetein P, Lockowandt U, Sarris G, Vouhe P, von Segesser L, Agewall S, Aladashvili A, Alexopoulos D, Antunes MJ, Atalar E, Brutel de la Riviere A, Doganov A, Eha J, Fajadet J, Ferreira R, Garot J, Halcox J, Hasin Y, Janssens S, Kervinen K, Laufer G, Legrand V, Nashef SA, Neumann FJ, Niemela K, Nihoyannopoulos P, Noc M, Piek JJ, Pirk J, Rozenman Y, Sabate M, Starc R, Thielmann M, Wheatley DJ, Windecker S, Zembala M. Guidelines on myocardial Revascularisation: The Task Force on Myocardial Revascularisation of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501-55.
European Revascularisation Guidelines – an essential read!, 111111. Kushner FG, Hand M, Smith SC, Jr., King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr., Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271-306. ].
The presence of intermediate grade left main stem (LMS) disease is not infrequent and angiographic evaluation may be challenging. Assessment using pressure-derived FFR is more challenging in comparison with non-LMS stenosis due to the requirement for disengagement of the guiding catheter and an inability to administer intracoronary adenosine. Some observational data exist to support the use of FFR in order to decide if revascularization should be deferred or performed [291291. Mallidi J, Atreya AR, Cook J, Garb J, Jeremias A, Klein LW, Lotfi A. Long-term outcomes following fractional flow reserve-guided treatment of angiographically ambiguous left main coronary artery disease: A meta-analysis of prospective cohort studies. Catheter Cardiovasc Interv. 2015;86:12-8. ].
Within the context of angiographically intermediate ULM lesions, a FFR value ≥0.75 (treated with medical therapy alone) has previously been associated with similar 3-year event-free survival compared to lesions with FFR < 0.75 managed by CABG (n=54) [131131. Bech GJ, Droste H, Pijls NH, De Bruyne B, Bonnier JJ, Michels HR, Peels KH, Koolen JJ. Value of fractional flow reserve in making decisions about bypass surgery for equivocal left main coronary artery disease. Heart. 2001;86:547-52. ]. Furthermore, Hamilos et al [132132. Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E, Barbato E, Heyndrickx GR, Wijns W, De Bruyne B. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 2009;120:1505-12.
A study demonstrating the long term safety of deferring LMS revascularisation if the FFR value ≥0.75.] demonstrated comparable mortality rates at up to 5 years follow-up in patients with angiographically equivocal LMS disease with FFR ≥0.80 treated medically (with other lesions treated with PCI if needed), and patients with LMS stenosis and FFR < 0.80 treated with CABG (n=213) [132132. Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E, Barbato E, Heyndrickx GR, Wijns W, De Bruyne B. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 2009;120:1505-12.
A study demonstrating the long term safety of deferring LMS revascularisation if the FFR value ≥0.75.]. In addition, although the percentage diameter stenosis at QCA correlated significantly with FFR (r=-0.38, p<0.001), a large scatter was evident with almost one quarter (23%) of patients with a LMS diameter stenosis of <50% being shown to have a haemodynamically significant FFR ( Figure 28 ) [132132. Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E, Barbato E, Heyndrickx GR, Wijns W, De Bruyne B. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 2009;120:1505-12.
A study demonstrating the long term safety of deferring LMS revascularisation if the FFR value ≥0.75.].
More recently, a pooled meta-analysis of 6 prospective cohort studies (n=525), in which 217 patients (41%) underwent revascularization based on the FFR results, no statistically significant difference between the groups in the rates of primary end point (a composite of all-cause death, non- fatal myocardial infarction and subsequent revascularizations) (p = 0.15), all- cause mortality (p=0.06) or non-fatal myocardial infarctions (p=0.76), with a significant significant increase in the rate of subsequent revascularizations in the deferred patients (p=0.002). Notably, the mode of revascularization was CABG in 94% of all the revascularized patients and a cut off value for FFR of <0.75 was used in five of the six studies investigated [263263. Mallidi J, Atreya AR, Cook J, Garb J, Jeremias A, Klein LW, Lotfi A. Long term outcomes following fractional flow reserve guided treatment of angiographically ambiguous left main coronary artery disease: A meta-analysis of prospective cohort studies. Catheter Cardiovasc Interv. 2015. [Epub ahead of print] ].
Tips and tricks in performing FFR in the left main
The use of FFR in assessing the significance of LMS lesions should be performed with certain principles in mind to avoid false positives or false negatives, where the additional role of other intravascular imaging techniques, such as IVUS as previously discussed, may need to be adopted ( Figure 29 ).
Functional approach for the assessment of the distal LMS bifurcation post PCI
Angiographic appearances of the SideB ostium after MainB stenting have previously been demonstrated to be unreliable, [133133. Koh JS, Koo BK, Kim JH, Yang HM, Park KW, Kang HJ, Kim HS, Oh BH, Park YB. Relationship Between Fractional Flow Reserve and Angiographic and Intravascular Ultrasound Parameters in Ostial Lesions: Major Epicardial Vessel vs. Side Branch Ostial Lesions. JACC Cardiovasc Interv. In Press 2012. ] with only a quarter (27%) of cases with a residual angiographic narrowing of ≥75% in the SideB being found to have a functionally significant narrowing in pressure wire studies [134134. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB, Choi YS, Tahk SJ. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633-7. ]. Within the context of the distal LMS bifurcation this also appears evident ( Figure 30 and Figure 31 ) [135135. Nam CW, Hur SH, Koo BK, Doh JH, Cho YK, Park HS, Yoon HJ, Kim H, Chung IS, Kim YN, Fearon WF, Tahk SJ, Kim KB. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ J. 2011;41:304-7. , 136136. Farooq V, Heo JH, Raber L, Brugaletta S, Radu M, Gogas BD, Diletti R, Onuma Y, Garcia-Garcia HM, Serruys PW. Tools & techniques: risk stratification and diagnostic tools in left main stem intervention. EuroIntervention. 2011;7:747-53. , 137137. Kang SJ, Mintz GS, Kim WJ, Lee JY, Oh JH, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Changes in left main bifurcation geometry after a single-stent crossover technique: an intravascular ultrasound study using direct imaging of both the left anterior descending and the left circumflex coronary arteries before and after intervention. Circ Cardiovasc Interv. 2011;4:355-61. ]. Reasons for this apparent paradox have been proposed relating the ellipsoid or oval appearances of the SideB opening secondary to carina shift, which is especially notable after MainB stenting ( Figure 31 ) [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. ]. It has previously been hypothesised that, during coronary angiography, the plane of the angiography cuts the SideB in the narrower segment of the ellipsoid opening rather than the longer segment given its oval shape, erroneously giving the impression of angiographic SideB compromise [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. ].
Discrepancies between the angiographic percentage diameter stenosis and FFR in jailed LCx lesions after LMS-to-LAD cross-over stenting have been reported [135135. Nam CW, Hur SH, Koo BK, Doh JH, Cho YK, Park HS, Yoon HJ, Kim H, Chung IS, Kim YN, Fearon WF, Tahk SJ, Kim KB. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ J. 2011;41:304-7. , 136136. Farooq V, Heo JH, Raber L, Brugaletta S, Radu M, Gogas BD, Diletti R, Onuma Y, Garcia-Garcia HM, Serruys PW. Tools & techniques: risk stratification and diagnostic tools in left main stem intervention. EuroIntervention. 2011;7:747-53. , 137137. Kang SJ, Mintz GS, Kim WJ, Lee JY, Oh JH, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Changes in left main bifurcation geometry after a single-stent crossover technique: an intravascular ultrasound study using direct imaging of both the left anterior descending and the left circumflex coronary arteries before and after intervention. Circ Cardiovasc Interv. 2011;4:355-61. ]. After bifurcation stenting of the distal LMS, pressure wire assessment of the SideB (LCx) appears to be beneficial, if a single cross-over (LMS to LAD) stent technique is utilised ( Figure 30 and Figure 32 ). Potential limitations of the use of FFR include the risk of dissecting the SideB ostium with a less flexible, less torquable, and less hydrophilic pressure wire as well as an increase in procedural time in rewiring the SideB through the MainB stent. Within the distal LMS, the risk may theoretically be less due to the larger vessel size.
Other pressure derived indices
Recently, there has been renewed interest in resting indices derived from resting gradients alone [distal coronary to aortic pressure (Pd/ Pa) or instantaneous wave-free ratio (iwFR)]. The DEFINE-FLAIR [292292. Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, Bhindi R, Lehman SJ, Walters D, Sapontis J, Janssens L, Vrints CJ, Khashaba A, Laine M, Van Belle E, Krackhardt F, Bojara W, Going O, Härle T, Indolfi C, Niccoli G, Ribichini F, Tanaka N, Yokoi H, Takashima H, Kikuta Y, Erglis A, Vinhas H, Canas Silva P, Baptista SB, Alghamdi A, Hellig F, Koo BK, Nam CW, Shin ES, Doh JH, Brugaletta S, Alegria-Barrero E, Meuwissen M, Piek JJ, van Royen N, Sezer M, Di Mario C, Gerber RT, Malik IS, Sharp ASP, Talwar S, Tang K, Samady H, Altman J, Seto AH, Singh J, Jeremias A, Matsuo H, Kharbanda RK, Patel MR, Serruys P, Escaned J. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017;376:1824-1834. ] and iFR-SWEDEHEART [293293. Götberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, Olsson SE, Öhagen P, Olsson H, Omerovic E, Calais F, Lindroos P, Maeng M, Tödt T, Venetsanos D, James SK, Kåregren A, Nilsson M, Carlsson J, Hauer D, Jensen J, Karlsson AC, Panayi G, Erlinge D, Fröbert O; iFR-SWEDEHEART Investigators. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017;376:1813-1823. ] showed non-inferiority of iFR-guided PCI to FFR-guided PCI.
To date, randomised trials comparing iFR-guided revascularization with angiography-guided revascularization or medical therapy are not available. The iFR has not been extensively validated for patients with LMS stenosis and will be tested in the LM dedicated trials. (POLBOS LM: NCT03508219)
FFR
- Fractional flow reserve (FFR) is a physiological parameter that reflects both the severity of epicardial stenosis and the amount of myocardium supplied, i.e., the influence of a coronary stenosis on the maximal perfusion of the subtended myocardium
- Within angiographically intermediate ULM lesions a number of studies have shown that revascularisation of the LMS can safely be deferred if the FFR value ≥0.75, with similar mortality rates to patients with significant ULM stenoses treated with CABG at up to 5 years follow-up
- When performing FFR in LMS lesions certain principles should be adhered to in order to prevent false positives or false negatives ( Figure 29), the operator may need to utilise IVUS imaging if the FFR results cannot be reliably interpreted
- Angiographic appearances of the SideB ostium after MainB stenting have previously been demonstrated to be unreliable with only a quarter (27%) of cases with a residual angiographic narrowing of ≥75% in the SideB being found to have a functionally significant narrowing in pressure wire studies. This is probably equally relevant in the distal LMS
- Pressure wire assessment of the jailed SideB may be necessary with the single stent approach, such as with cross-over stenting from the LMS–LAD
OPTICAL COHERENCE TOMOGRAPHY
Principles of OCT in the left main
In the current European guideline for myocardial revascularisation [294294. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, Group ESCSD. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. ], OCT is not considered for LM intervention. The use of OCT guidance in the LMS is limited by the reduced penetration of the OCT light, precluding the assessment of the media to media distance to aid in stent sizing. Given the high resolution of OCT, its role in assessing the MLD/MLA/MSA, stent sizing (diameter and length), lesion complexity, calcification, stent apposition and arterial wall response of DES are all potential clinical applications of this technology.
Parodi et al [139139. Parodi G, Maehara A, Giuliani G, Kubo T, Mintz GS, Migliorini A, Valenti R, Carrabba N, Antoniucci D. Optical coherence tomography in unprotected left main coronary artery stenting. EuroIntervention. 2010;6:94-9. ] first demonstrated the potential safety and feasibility of this technology with the previous generation M3 OCT Imaging System (LightLab Imaging Inc., Westford, MA, USA) in assessing DES implantation post LMS stenting at baseline and 6-month follow-up. Because this OCT system utilised the occlusive balloon technique, only approximately two thirds of the implanted LMS stent could be visualised. Newer, current generation frequency-domain OCT (FD-OCT) systems are capable of rapid pullbacks, do not require the use of occlusion balloons and have been shown to potentially allow for greater visualisation of the LMS [264264. Fujino Y, Attizzani GF, Bezerra HG, Wang W, Tahara S, Yamamoto H, Chamie D, Kanaya T, Mehanna E, Takagi K, Nakamura S, Costa MA. Serial assessment of vessel interactions after drug-eluting stent implantation in unprotected distal left main coronary artery disease using frequency-domain optical coherence tomography. JACC Cardiovasc Interv. 2013;6:1035-45 , 265265. Taglieri N, Ghetti G, Saia F, Moretti C, Gallo P, Dall’Ara G, Palmerini T, Marrozzini C, Rapezzi C, Marzocchi A. Biolimus-a9 eluting stent implantion for unprotected left main coronary artery stenosis: 9-month strut coverage as assessed by optical coherence tomography. J Invasive Cardiol. 2015;27:70-7. , 266266. Burzotta F, Dato I, Trani C, Pirozzolo G, De Maria GL, Porto I, Niccoli G, Leone AM, Schiavoni G, Crea F. Frequency domain optical coherence tomography to assess non-ostial left main coronary artery. EuroIntervention. 2015;10:e1-8 ]. There are, however, no reported experiences as to the success rate for visualising the aorto-ostium with new generation FD-OCT systems, (which is potentially more technically difficult to perform as detailed below).
Tips and tricks in performing OCT in the left main
- In order to visualise the LMS ostium fully, the key is to ensure that the catheter tip is sufficiently disengaged from the coronary ostium to allow visualisation with the OCT imaging wire during the pullback, but close enough to allow injection of contrast for blood clearance. This will cause inevitable over-spilling of contrast into the aortic cusps but, provided adequate injection of contrast into the LMS occurs to allow for blood clearance, this should not be of concern. From an anecdotal perspective this technique is technically more challenging but can be grasped with experience – reported success rates in the literature are awaited.
- As for IVUS, separate pullbacks of the LAD and LCx are advised to allow visualisation and measurements of geometrical parameters such as the MLD, MLA and MSA as previously discussed.
Three-dimensional optical coherence tomography (OCT)
It is the authors’ opinion that the potential for 3-dimensional OCT (3D-OCT) in visualising the LMS bifurcation, to assess the effects of LMS bifurcation stenting, carina shift ( Figure 32 ), plaque shift and SideB compromise, are areas of real potential for this rapidly developing technology. At the time of writing, although both off-line (requiring post-processing of the OCT pullbacks) and online (i.e., available immediately in the catheterisation laboratory) systems exist, a commercially available online system of adequate resolution is still awaited [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. , 140140. Farooq V, Serruys PW, Heo JH, Gogas BD, Okamura T, Gomez-Lara J, Brugaletta S, Garcìa-Garcìa HM, van Geuns RJ. New Insights Into the Coronary Artery Bifurcation. Hypothesis-Generating Concepts Utilizing 3-Dimensional Optical Frequency Domain Imaging. JACC Cardiovasc Interv. 2011;4:921-931. , 141141. Farooq V, Gogas BD, Okamura T, Heo JH, Magro M, Gomez-Lara J, Onuma Y, Radu MD, Brugaletta S, van Bochove G, van Geuns RJ, Garcia-Garcia HM, Serruys PW. Three-dimensional optical frequency domain imaging in conventional percutaneous coronary intervention: the potential for clinical application. Eur Heart J. 2011 Nov 21. [Epub ahead of print] , 142142. Gogas BD, van Geuns RJ, Farooq V, Regar E, Heo JH, Ligthart J, Serruys PW. Three-Dimensional Reconstruction of the Post-Dilated ABSORB Everolimus-Eluting Bioresorbable Vascular Scaffold in a True Bifurcation Lesion for Flow Restoration. JACC Cardiovasc Interv. 2011;4:1149-50. , 143143. Farooq V, Okamura T, Gogas BD, Heo JH, Magro M, Gomez-Lara J, Brugaletta S, Onuma Y, Radu M, Garcia-Garcia HM, Serruys PW. 3D reconstructions of optical frequency domain imaging to improve understanding of conventional PCI. JACC Cardiovasc Imaging. 2011;4:1044-6. , 144144. Okamura T, Onuma Y, Garcia-Garcia HM, Regar E, Wykrzykowska JJ, Koolen J, Thuesen L, Windecker S, Whitbourn R, McClean DR, Ormiston JA, Serruys PW. 3-Dimensional optical coherence tomography assessment of jailed side branches by bioresorbable vascular scaffolds: a proposal for classification. JACC Cardiovasc Interv. 2010;3:836-44. ].
OCT may have particular value in the treatment of bifurcation PCI [295295. Onuma Y, Katagiri Y, Burzotta F, Holm NR, Amabile N, Okamura T, Mintz GS, Darremont O, Lassen JF, Lefèvre T, Louvard Y, Stankovic G, Serruys PW. Joint consensus on the use of OCT in coronary bifurcation lesions by the European and Japanese bifurcation clubs. EuroIntervention. 2019;14:e1568-e1577. ], without the limitations of conventional angiography such as foreshortening or overlap, thus the LMS distal bifurcation can be exceptional candidate for OCT guidance. Recently, 3D reconstruction has become feasible online (ILUMIENTMTM OptisTM system (Abbott Vascular), OFDI (Lunawave® system; Terumo, Tokyo, Japan). So far, there are no dedicated trials to evaluate the feasibility of OCT to treat LMS bifurcation, trials of OCT for bifurcation (OCTOBER: NCT03171311; OPTIMUM: NCT02972489; DOCTOR Recross: NCT02234804) are undergoing to add the evidence of OCT utility over angio-guided PCI.
OCT
- The high resolution of OCT may have an application in assessing stent sizing (diameter and length), lesion complexity, calcification, stent apposition and arterial wall response of DES
- OCT guidance in the LMS is limited by the reduced penetration of the OCT light, precluding the assessment of the media to media distance to aid in stent sizing
- The role of 2D (and 3D-OCT) technology remains to be fully defined in the context of the LMS – initial studies have proved to be promising
- The use of OCT in visualising the aorto-ostium is technically more difficult to perform - reported success rates in the literature are awaited
ANATOMICAL VS. FUNCTIONAL APPROACH IN ASSESSING DISTAL LEFT MAIN BIFURCATIONS
New imaging techniques to assess SideB compromise include 3D-OCT as previously described [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. , 140140. Farooq V, Serruys PW, Heo JH, Gogas BD, Okamura T, Gomez-Lara J, Brugaletta S, Garcìa-Garcìa HM, van Geuns RJ. New Insights Into the Coronary Artery Bifurcation. Hypothesis-Generating Concepts Utilizing 3-Dimensional Optical Frequency Domain Imaging. JACC Cardiovasc Interv. 2011;4:921-931. , 141141. Farooq V, Gogas BD, Okamura T, Heo JH, Magro M, Gomez-Lara J, Onuma Y, Radu MD, Brugaletta S, van Bochove G, van Geuns RJ, Garcia-Garcia HM, Serruys PW. Three-dimensional optical frequency domain imaging in conventional percutaneous coronary intervention: the potential for clinical application. Eur Heart J. 2011 Nov 21. [Epub ahead of print] , 142142. Gogas BD, van Geuns RJ, Farooq V, Regar E, Heo JH, Ligthart J, Serruys PW. Three-Dimensional Reconstruction of the Post-Dilated ABSORB Everolimus-Eluting Bioresorbable Vascular Scaffold in a True Bifurcation Lesion for Flow Restoration. JACC Cardiovasc Interv. 2011;4:1149-50. , 143143. Farooq V, Okamura T, Gogas BD, Heo JH, Magro M, Gomez-Lara J, Brugaletta S, Onuma Y, Radu M, Garcia-Garcia HM, Serruys PW. 3D reconstructions of optical frequency domain imaging to improve understanding of conventional PCI. JACC Cardiovasc Imaging. 2011;4:1044-6. , 144144. Okamura T, Onuma Y, Garcia-Garcia HM, Regar E, Wykrzykowska JJ, Koolen J, Thuesen L, Windecker S, Whitbourn R, McClean DR, Ormiston JA, Serruys PW. 3-Dimensional optical coherence tomography assessment of jailed side branches by bioresorbable vascular scaffolds: a proposal for classification. JACC Cardiovasc Interv. 2010;3:836-44. ]. As illustrated, cross-over stenting from the LMS to LAD may pinch and even compromise the circumflex ostium (or other SideB), depending on the magnitude of the carina shift
( Figure 32A ). This is consistent with the findings from an IVUS study from Kang et al [137137. Kang SJ, Mintz GS, Kim WJ, Lee JY, Oh JH, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Changes in left main bifurcation geometry after a single-stent crossover technique: an intravascular ultrasound study using direct imaging of both the left anterior descending and the left circumflex coronary arteries before and after intervention. Circ Cardiovasc Interv. 2011;4:355-61. ] where the main mechanism of lumen loss at the LCx - after cross-over LMS-LAD stenting - was shown to be carina shift associated with a narrow angle between the LAD and the LCx ( Figure 32B ), with a lesser contribution of plaque shift. Furthermore, a shallower angle between the MainB and SideB has been linked to an increased likelihood of carina shift occurring, [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. , 145145. Vassilev D, Gil RJ. Relative dependence of diameters of branches in coronary bifurcations after stent implantation in main vessel-importance of carina position. Kardiologia polska. 2008;66:371-8; discussion 379. , 146146. Gil RJ, Vassilev D, Formuszewicz R, Rusicka-Piekarz T, Doganov A. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol. 2009;22:E1-E10. , 147147. Asakaura Y, Takagi S, Ishikawa S, Asakura K, Sueyoshi K, Sakamoto M, Takatsuki S, Oda T, Nakagawa M, Furukawa Y, Oyamada K, Iwanaga S, Ogawa S, Hinohara T. Favorable strategy for the ostial lesion of the left anterior descending coronary artery: influence on narrowing of circumflex coronary artery. Cathet Cardiovasc Diagn. 1998;43:95-100. , 148148. Suarez de Lezo J, Medina A, Martin P, Novoa J, Pan M, Caballero E, Melian F, Mazuelos F, Quevedo V. Predictors of ostial side branch damage during provisional stenting of coronary bifurcation lesions not involving the side branch origin: an ultrasonographic study. EuroIntervention. 2012 Feb 20;7:1147-54. , 149149. Farooq V, Serruys PW, Heo JH, Gogas BD, Okamura T, Gomez-Lara J, Brugaletta S, Garcia-Garcia HM, van Geuns RJ. New insights into the coronary artery bifurcation hypothesis-generating concepts utilizing 3-dimensional optical frequency domain imaging. JACC Cardiovasc Interv. 2011;4:921-31. ] the clinical implications being that the potential risk of SideB closure secondary to carina shift may be more prevalent with shallower bifurcation angles, and that the operator should potentially protect the SideB with a coronary wire.
Consequently, kissing balloon post dilatation (KBPD) is required to reposition the carina endoluminally so that pinching/compromise of the SideB ostium is restored. In the clinical case from ( Figure 30 ), no KBPD was carried out after cross-over stenting from the LMS to LAD, as the SideB was not compromised on subsequent FFR analysis (FFR 0.95).
Two alternative views to this approach are worth considering:
1) Despite the lack of haemodynamic compromise to the LCx on the pressure wire study, 3D-OCT demonstrated that varying degrees of carina shift ( Figure 32 A ) (numbers 1-3) may cause differing magnitudes of pinching and potential haemodynamic compromise. In a situation with no haemodynamic compromise (i.e., with a normal pressure study), the SideB orifice area (minimal stent area [MSA]) may potentially be reduced. The “bigger-is-better” paradigm would suggest that a larger SideB ostial area may be less susceptible to the expected neointimal response and risk of binary restenosis, compared to a SideB with a smaller orifice area [150150. Romagnoli E, Sangiorgi GM, Cosgrave J, Guillet E, Colombo A. Drug-Eluting Stenting: The Case for Post-Dilation. JACC Cardiovasc Interv. 2008;1:22-31. , 151151. McDaniel MC, Douglas JS, Jr. Stent area by intravascular ultrasound and outcomes in left main intervention with drug-eluting stents: small stents, more events. Circ Cardiovasc Interv. 2011;4:542-4. ]. As previously discussed. LAD ostial area of approximately 6 mm2 and LCx ostial area (minimal stent area [MSA]) of 5 mm2 determined by IVUS ( Figure 25 ) were associated with a significantly lower freedom from MACE at 2 years ( Figure 26 ) compared to patients with MSA below these values [121121. Kang SJ, Ahn JM, Song H, Kim WJ, Lee JY, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Mintz GS, Park SW, Park SJ. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv. 2011;4:562-9.
A study that elegantly demonstrated IVUS predictors of angiographic restenosis post ULM PCI within the LMS and its side branches.].
2) The presence of “floating struts” at the SideB of a coronary bifurcation with MainB stent implantation have been reported to be more prevalent and associated with a reduced incidence of strut coverage [152152. Gutierrez-Chico JL, Regar E, Nuesch E, Okamura T, Wykrzykowska J, di Mario C, Windecker S, van Es GA, Gobbens P, Juni P, Serruys PW. Delayed coverage in malapposed and side-branch struts with respect to well-apposed struts in drug-eluting stents: in vivo assessment with optical coherence tomography. Circulation. 2011;124:612-23. ]. Conversely, struts over a SideB orifice area may act as a focus for neointimal bridges which may potentially compromise the SideB ostium [153153. Foin N, Viceconte N, Chan PH, Lindsay AC, Krams R, Di Mario C. Jailed side branches: fate of unapposed struts studied with 3D frequency-domain optical coherence tomography. J Cardiovasc Med (Hagerstown). 2011;12:581-2. ]. The incorporation of final KBPD is recommended by the authors with bifurcation stenting incorporating the one or two-stent approach to limit the presence of floating struts, the long term clinical impact of this approach is however yet to be determined. [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. , 154154. Niemela M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Kumsars I, Jegere S, Dombrovskis A, Gunnes P, Stavnes S, Steigen TK, Trovik T, Eskola M, Vikman S, Romppanen H, Makikallio T, Hansen KN, Thayssen P, Aberge L, Jensen LO, Hervold A, Airaksinen J, Pietila M, Frobert O, Kellerth T, Ravkilde J, Aaroe J, Jensen JS, Helqvist S, Sjogren I, James S, Miettinen H, Lassen JF, Thuesen L. Randomised comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123:79-86. , 155155. Hoye A, Iakovou I, Ge L, van Mieghem CA, Ong AT, Cosgrave J, Sangiorgi GM, Airoldi F, Montorfano M, Michev I, Chieffo A, Carlino M, Corvaja N, Aoki J, Rodriguez Granillo GA, Valgimigli M, Sianos G, van der Giessen WJ, de Feyter PJ, van Domburg RT, Serruys PW, Colombo A. Long-term outcomes after stenting of bifurcation lesions with the crush technique: predictors of an adverse outcome. J Am Coll Cardiol. 2006;47:1949-58. , 156156. Hildick-Smith D, Lassen JF, Albiero R, Lefevre T, Darremont O, Pan M, Ferenc M, Stankovic G, Louvard Y. Consensus from the 5th European Bifurcation Club meeting. EuroIntervention. 2010;6:34-8. , 157157. Stankovic G, Darremont O, Ferenc M, Hildick-Smith D, Louvard Y, Albiero R, Pan M, Lassen JF, Lefevre T. Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention. 2009;5:39-49. ].
PRACTICAL GUIDELINES ON IMPLEMENTING THE USE OF CORONARY ANGIOGRAPHY AND INTRAVASCULAR IMAGING/ADJUNCTIVE DEVICES
The implementation of angiographic criteria, IVUS and FFR assessments in determining the significance of left main lesions in the EXCEL trial is detailed in an algorithm below ( Figure 33 ) [287287. Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, Kandzari DE, Morice MC, Lembo N, Brown WM 3rd, Taggart DP, Banning A, Merkely B, Horkay F, Boonstra PW, van Boven AJ, Ungi I, Bogáts G, Mansour S, Noiseux N, Sabaté M, Pomar J, Hickey M, Gershlick A, Buszman P, Bochenek A, Schampaert E, Pagé P, Dressler O, Kosmidou I, Mehran R, Pocock SJ, Kappetein AP; EXCEL Trial Investigators. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med. 2016;375::2223-2235. ]. Highlighted areas of the algorithm pertain to the use of IVUS and FFR in intermediate lesions. Although the evidence of iFR for left main lesion is scarce, iFR can be used instead of FFR according to the current ESC guidelines [294294. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, Group ESCSD. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. ].
Left main bifurcation
- The predominant mechanism of SideB compromise (LCx) after LMS-LAD cross-over stenting is secondary to carina shift, with a smaller contribution from plaque shift
- A shallower bifurcation angle appears to be associated with a greater likelihood of carina shift occurring with the subsequent risk of potential SideB compromise
- Kissing balloon post dilatation (KBPD) will potentially reposition the carina endoluminally if carina (or plaque shift) occurs, thereby reducing the pinching/compromise of the SideB ostium
- Practical guidelines on implementing intravascular imaging/adjunctive devices are detailed in ( Figure 33 )
VULNERABLE PLAQUE, INTRAVASCULAR IMAGING AND POTENTIAL TREATMENT
Introduction
The use of intravascular imaging modalities to identify vulnerable plaque and lipid-rich regions are innovative areas of on-going research, in potentially guiding stent placement and “plaque sealing” or “shielding” of vulnerable plaque. At present, despite case reports and pilot trials suggesting a possible benefit in using intravascular imaging modalities in non-left main lesions, [158158. Rodes-Cabau J, Bertrand OF, Larose E, Dery J-P, Rinfret S, Bagur R, Proulx G, Nguyen CM, Cote M, Landcop M-C, Boudreault J-R, Rouleau J, Roy L, Gleeton O, Barbeau G, Noel B, Courtis J, Dagenais GR, Despres J-P, DeLarochelliere R. Comparison of Plaque Sealing With Paclitaxel-Eluting Stents Versus Medical Therapy for the Treatment of Moderate Nonsignificant Saphenous Vein Graft Lesions: The Moderate VEin Graft LEsion Stenting With the Taxus Stent and Intravascular Ultrasound (VELETI) Pilot Trial. Circulation 2009;120:1978-1986. , 159159. Ramcharitar S, Gonzalo N, van Geuns RJ, Garcia-Garcia HM, Wykrzykowska JJ, Ligthart JM, Regar E, Serruys PW. First case of stenting of a vulnerable plaque in the SECRITT I trial-the dawn of a new era? Nature reviews. Cardiology. 2009;6:374-8. , 160160. Wykrzykowska J, Diletti R, Gutierrez-Chico JL, Van Geuns RJ, Van der Giessen WJ, Ramcharitar S, Duckers HE, Schultz C, de Feyter P, Van der Ent M, Regar E, de Jaeger P, Garcia-Garcia HM, Pawar R, Gonzalo N, Ligthart J, de Schepper J, Van den Berg N, Milewski K, Granada J, Serruys PW. Plaque sealing and passivation with a mechanical self-expanding low outward force nitinol vShield device for the treatment of IVUS and OCT-derived thin cap fibroatheromas (TCFAs) in native coronary arteries. Report of the pilot study vShield Evaluated at Cardiac hospital in Rotterdam for Investigation and Treatment of TCFA (SECRITT). In Press. EuroIntervention. 2012 in press. ] the adoption of such an approach remains hypothetical and should probably be avoided. Within the context of the left main, the concept of plaque sealing is at present completely hypothetical.
Location of vulnerable plaque
Valgimigli [161161. Valgimigli M, Rodriguez-Granillo GA, Garcia-Garcia HM, Malagutti P, Regar E, de Jaegere P, de Feyter P, Serruys PW. Distance from the ostium as an independent determinant of coronary plaque composition in vivo: an intravascular ultrasound study based radiofrequency data analysis in humans. Eur Heart J. 2006;27:655-63. , 162162. Valgimigli M, Rodriguez-Granillo GA, Garcia-Garcia HM, Vaina S, De Jaegere P, De Feyter P, Serruys PW. Plaque composition in the left main stem mimics the distal but not the proximal tract of the left coronary artery: influence of clinical presentation, length of the left main trunk, lipid profile, and systemic levels of C-reactive protein. J Am Coll Cardiol. 2007;49:23-31. ] et al have previously shown that plaque composition favouring propensity to vulnerability – in particular volume of necrotic core as assessed by the radio-frequency information of IVUS (IVUS-virtual histology [IVUS-VH]) – is more commonly located in the proximal coronary vasculature compared to the LMS, with a progressive decline in necrotic core content more distally. Within the LMS itself, the necrotic core appears to be minimal, thus mimicking the distal (and not the proximal) left coronary artery. Yet, when plaque rupture does occur in the LMS, it is more likely to occur in the distal LMS – findings that can be explained by the distal LMS tending to harbour a greater necrotic core content compared to the proximal half of the LMS, and being especially evident with a long LMS as illustrated in the case study demonstrating plaque rupture on 2D- and 3D-OCT imaging ( Figure 34 ) [161161. Valgimigli M, Rodriguez-Granillo GA, Garcia-Garcia HM, Malagutti P, Regar E, de Jaegere P, de Feyter P, Serruys PW. Distance from the ostium as an independent determinant of coronary plaque composition in vivo: an intravascular ultrasound study based radiofrequency data analysis in humans. Eur Heart J. 2006;27:655-63. , 162162. Valgimigli M, Rodriguez-Granillo GA, Garcia-Garcia HM, Vaina S, De Jaegere P, De Feyter P, Serruys PW. Plaque composition in the left main stem mimics the distal but not the proximal tract of the left coronary artery: influence of clinical presentation, length of the left main trunk, lipid profile, and systemic levels of C-reactive protein. J Am Coll Cardiol. 2007;49:23-31. , 163163. Cheruvu PK, Finn AV, Gardner C, Caplan J, Goldstein J, Stone GW, Virmani R, Muller JE. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. Am J Cardiol. 2007;50:940-9. , 164164. Tyczynski P, Pregowski J, Mintz GS, Witkowski A, Kim SW, Waksman R, Satler L, Pichard A, Kalinczuk L, Maehara A, Weissman NJ. Intravascular ultrasound assessment of ruptured atherosclerotic plaques in left main coronary arteries. Am J Cardiol. 2005;96:794-8. ].
The most plausible theory to explain these findings is that of the well-established role shear stress modulation has at the coronary bifurcations – distally in the LMS and more proximally in the coronary vasculature, due to these locations being the sites of the major coronary bifurcations. The sites of coronary bifurcations have been shown to lead to flow turbulences generated by high-velocity blood impacting against the anatomical flow dividers (carina), which subsequently exposes the opposing vessel walls of the carina to low-oscillatory shear stress, and consequent risk of unfavourable plaque progression, plaque vulnerability and rupture [165165. Farooq V, Gogas BD, Serruys PW. Restenosis: delineating the numerous causes of drug-eluting stent restenosis. Circ Cardiovasc Interv. 2011;4:195-205. , 166166. Rodriguez-Granillo GA, Garcia-Garcia HM, Wentzel J, Valgimigli M, Tsuchida K, van der Giessen W, de Jaegere P, Regar E, de Feyter PJ, Serruys PW. Plaque composition and its relationship with acknowledged shear stress patterns in coronary arteries. Am J Cardiol. 2006;47:884-5. , 167167. Kimura BJ, Russo RJ, Bhargava V, McDaniel MB, Peterson KL, DeMaria AN. Atheroma morphology and distribution in proximal left anterior descending coronary artery: in vivo observations. Am J Cardiol. 1996;27:825-31. ].
Components of vulnerable plaque
Histologically, the main components of vulnerable plaques are a thin fibrous cap (<65 microns) and a core of necrotic tissue. Additionally, other plaque vulnerability criteria include factors such as the presence of positive remodelling, haemorrhages, microchannels or calcified nodules [168168. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. Am J Cardiol. 2006;47(8 Suppl):C13-8. , 169169. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262-75. , 170170. Michel JB, Virmani R, Arbustini E, Pasterkamp G. Intraplaque haemorrhages as the trigger of plaque vulne-rability. Eur Heart J. 2011;32:1977-85. ]. Importantly, the severity of the coronary stenosis has not emerged as a criterion for plaque vulnerability, thereby diminishing the value of both angiography and FFR measurements in the detection of vulnerable lesions that may be responsible for future cardiac events [163163. Cheruvu PK, Finn AV, Gardner C, Caplan J, Goldstein J, Stone GW, Virmani R, Muller JE. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. Am J Cardiol. 2007;50:940-9. , 171171. Glaser R, Selzer F, Faxon DP, Laskey WK, Cohen HA, Slater J, Detre KM, Wilensky RL. Clinical progression of incidental, asymptomatic lesions discovered during culprit vessel coronary intervention. Circulation. 2005;111:143-9. , 172172. Burke AP, Farb A, Malcom GT, Liang YH, Smialek J, Virmani R. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. N Engl J Med. 1997;336:1276-82. ].
IVUS imaging provides a high tissue penetration which allows for the visualisation of the entire vessel wall. Furthermore, IVUS-VH provides information about the tissue composition of atherosclerotic lesions that are displayed as four categories (fibrous, fibro-fatty, calcium, necrotic core) [173173. Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002;106:2200-6. , 174174. Garcia-Garcia HM, Gonzalo N, Regar E, Serruys PW. Virtual histology and optical coherence tomography: from research to a broad clinical application. Heart 2009;95:1362-74. , 175175. Garcia-Garcia HM, Gogas BD, Serruys PW, Bruining N. IVUS-based imaging modalities for tissue characterization: similarities and differences. Int J Cardiovasc Imaging. 2011;27:215-24. ]. Conversely, OCT provides a superior resolution (x10 higher axial resolution), which potentially allows for the visualisation of the plaque fibrous cap, erosions, ruptures, adjacent thrombi, calcified nodules and microchannels. However, the higher resolution of OCT is at the cost of limited tissue penetration, which potentially makes the combined use of IVUS and OCT vital in the comprehensive assessment of vulnerability criteria of plaque ( Figure 35 ).
“Treatment” of vulnerable plaque
How should the presence of vulnerable plaques - as assessed by intracoronary imaging - impact on our treatment strategy? PROSPECT [176176. Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP, Parise H, Templin B, White R, Zhang Z, Serruys PW. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 364:226-35. ] is to date the only large-scale clinical trial which investigated the prognostic value of IVUS-VH-derived plaque parameters. It should, however, be emphasised that the PROSPECT trial did not enrol patients with vulnerable plaque in the left main: consequently, any application of the findings of PROSPECT to the left main at present remains entirely theoretical. Within the PROSPECT trial the presence of IVUS-VH-derived TCFAs was demonstrated to be one of the main predictors (HR 3.31, 95% CI 1.77–6.36, p <0.001) of the occurrence of major cardiovascular events at three years follow-up. Expressed in terms of absolute numbers: of 51 non-culprit-lesion-related recurrent events occurring in the imaged segments, 26 (51%) occurred at sites with TCFAs. However, considering that a total of 595 TCFAs were identified in the total PROSPECT study population, the lack of specificity precludes us from deriving any clinical recommendations on how to proceed with vulnerable plaques. Although the visualisation of vulnerable plaques is feasible and a “preventive invasive treatment” may appear appealing (e.g., plaque sealing), there is currently insufficient supportive evidence to justify such an invasive approach. As to whether the identification of additional morphological plaque vulnerability criteria by OCT, such as the cap thickness, or non-morphology-related vulnerability criteria, such as inflammatory activity, will further improve its specificity to identify vulnerable plaques responsible for future events is the subject of on-going research.
Furthermore, the relatively low event rates in the PROSPECT study should remind us of the paramount importance of secondary prevention, namely the induction and surveillance of state-of-the-art cardiovascular medication and secondary prevention measures. Studies specifically assessing the effects of medical treatment (e.g., statins) and how this treatment impacts upon the evolution of the cap thickness and plaque composition over time are expected.
Vulnerable plaque
- The severity of the coronary stenosis has not emerged as a criterion for plaque vulnerability, thereby diminishing the value of both angiography and FFR measurements in the detection of vulnerable lesions that may be responsible for future cardiac events
- Shear stress modulation at major coronary bifurcations influences necrotic core content in the LMS and coronary vasculature
- Necrotic core content is more commonly located in the proximal coronary vasculature compared to the LMS, with a progressive decline in volume more distally. Within the LMS necrotic core content appears minimal and is more commonly located in the distal LMS
- The use of intravascular imaging modalities to identify vulnerable plaque in order to “plaque seal” or “shield” remains entirely hypothetical and should probably be avoided
Interventional techniques
BACKGROUND
By definition, the distal LMS always ends in a bifurcation or even a trifurcation, giving rise to the left anterior descending (LAD) and left circumflex (LCx), and often an intermediate vessel. Consequently, every effort should be made to ensure that all importantly sized branches are appropriately revascularised and remain patent post procedure. Although carina shift is the predominant mechanism of SideB closure as previously discussed, [134134. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB, Choi YS, Tahk SJ. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633-7. , 177177. Colombo A, Al-Lamee R. Bifurcation lesions: an inside view. Circ Cardiovasc Interv. 2010;3:94-6. , 178178. Vassilev D, Gil R, Kwan T, Nguyen T, Nanjundappa A, Doganov A. Extension distance mismatch--an unrecognized factor for suboptimal side branch ostial coverage in bifurcation lesion stenting. Int J Cardiol. 2010;23:305-18. , 179179. Medina A, Martin P, Suarez de Lezo J, Amador C, Pan M, Melian F, Hernandez E, Burgos L, Ojeda S, Ortega JR, Garcia A. Vulnerable carina anatomy and ostial lesions in the left anterior descending coronary artery after floating-stent treatment. Revista espanola de cardiologia. 2009;62:1240-9. , 180180. Koo BK, Waseda K, Kang HJ, Kim HS, Nam CW, Hur SH, Kim JS, Choi D, Jang Y, Hahn JY, Gwon HC, Yoon MH, Tahk SJ, Chung WY, Cho YS, Choi DJ, Hasegawa T, Kataoka T, Oh SJ, Honda Y, Fitzgerald PJ, Fearon WF. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010;3:113-9. , 181181. Van der Giessen AG, Wentzel JJ, Meijboom WB, Mollet NR, van der Steen AF, van de Vosse FN, de Feyter PJ, Gijsen FJ. Plaque and shear stress distribution in human coronary bifurcations: a multislice computed tomography study. EuroIntervention. 2009;4:654-61. ] given that the LMS is a large vessel and, when diseased, is associated with a high plaque volume, [3939. Oviedo C, Maehara A, Mintz GS, Araki H, Choi SY, Tsujita K, Kubo T, Doi H, Templin B, Lansky AJ, Dangas G, Leon MB, Mehran R, Tahk SJ, Stone GW, Ochiai M, Moses JW. Intravascular ultrasound classification of plaque distribution in left main coronary artery bifurcations: where is the plaque really located? Circ Cardiovasc Interv. 2010;3:105-12.
Plaque distribution at the left main - an essential read!] plaque shift and incomplete stent expansion are further important technical issues that must be considered.
Proximal MainB lesions (i.e., the left main) can often be underestimated by referring to the distal SideB (LAD and LCx) size. The true size of the proximal MainB (left main) is dictated by the scaling laws, such as Murray’s law and Finet’s law, which use the law of conservation of mass, namely that the sum of the outflows from a bifurcation equals the inflow. These important principles should be borne in mind whenever undertaking left main PCI in order to ascertain the true vessel size of the left main angiographically ( Figure 36 ) [182182. Finet G, Huo Y, Rioufol G, Ohayon J, Guerin P, Kassab GS. Structure-function relation in the coronary artery tree: from fluid dynamics to arterial bifurcations. EuroIntervention 2010;6 Suppl J:J10-15. ]. Murray’s law is also known as the cube law and states that the sum of the cubes of the daughter vessel diameters (the LAD and LCx in the context of the left main) is equal to the cube of the mother vessel diameter (LMS). The formula in the context of the left main is as follows: [Left Main]3= [LAD]3+ [LCx]3. The more refined HK model and the simplified law of Finet (0.678 x [LAD+LCx]) as illustrated ( Figure 36 ), are more accurate ways of assessing the left main diameter in the context of the SideBs (LAD and LCx) [182182. Finet G, Huo Y, Rioufol G, Ohayon J, Guerin P, Kassab GS. Structure-function relation in the coronary artery tree: from fluid dynamics to arterial bifurcations. EuroIntervention 2010;6 Suppl J:J10-15. , 183183. Girasis C, van Geuns RJ, Onuma Y, Serruys PW. Essentials of quantitative angiography for bifurcation lesions. EuroIntervention. 2010;6 Suppl J:J36-43. ].
A detailed overview of the different methods of undertaking ULM PCI is discussed follows, ranging from ostial and mid vessel disease, to undertaking bifurcation stenting in the distal LMS: illustrative examples in performing these various procedures are provided where necessary. The use of adjunctive intravascular imaging devices/adjunctive tools has previously been described and will not be discussed further.
AORTO-OSTIAL AND MID VESSEL LESIONS
Aorto-ostial ( Figure 37 ) and mid vessel ( Figure 38 ) lesions should be treated with a single stent strategy. The treatment of these lesion subsets comprises approximately 30% of ULM PCI [184184. Mehilli J, Kastrati A, Byrne RA, Bruskina O, Iijima R, Schulz S, Pache J, Seyfarth M, Massberg S, Laugwitz KL, Dirschinger J, Schomig A. Paclitaxel- versus sirolimus-eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2009;53:1760-8. ]. From a technical perspective, mid vessel lesions are the least difficult to perform in the LMS – appropriate sizing of the stent is, however, crucial.
The following “tips and tricks” should be taken into account when performing ULM PCI in the aorto-ostial lesion subset.
- Careful imaging must be performed to ensure adequate visualisation of the ostium and adjacent aorta. Appropriate working views should be selected, usually from AP-cranial to LAO-cranial.
- A short-tip 6 Fr or 7 Fr guide catheter with side holes can be used for severe ostial lesions - the operator should, however, be aware of the lack of damping effect with this catheter and exercise caution.
- The passage of a coronary wire into the distal vessel to obtain a distal loop in the vessel periphery is useful to allow appropriate repositioning of the guide catheter. Careful withdrawal and pushing of the looped coronary wire leads to the advancement or retraction of the guide catheter, respectively, without any significant risk of distal perforation ( Figure 39 ). This is especially useful if the LMS stenosis is severe and the guide catheter causes transient occlusion of the vessel, or to determine the exact location of the ostium when positioning the stent.
- Other tips to facilitate ostial stent placement include the passage of a second coronary wire into the aortic root to prevent selective engagement of the guide catheter into the coronary ostium ( Figure 40 ) or the Szabo (stent tail wire) [185185. Kern MJ, Ouellette D, Frianeza T. A new technique to anchor stents for exact placement in ostial stenoses: the stent tail wire or Szabo technique. Catheter Cardiovasc Interv. 2006;68:901-6. , 186186. Gutierrez-Chico JL, Villanueva-Benito I, Villanueva-Montoto L, Vazquez-Fernandez S, Kleinecke C, Gielen S, Iniguez-Romo A. Szabo technique versus conventional angiographic placement in bifurcations 010-001 of Medina and in aorto-ostial stenting: angiographic and procedural results. EuroIntervention. 2010;5:801-8. ] technique ( Figure 41 ). In brief, the Szabo technique uses a second coronary wire positioned in the aorta to anchor the stent at the ostial location by passing the proximal end of the anchor wire through the last cell of the stent; however, this approach is complex and has recently been shown potentially to damage the stent or risk stent dislodgement [187187. Ferrer-Gracia MC, Sanchez-Rubio J, Calvo-Cebollero I. Stent dislodgement during Szabo technique. Int J Cardiol. 2011;147:e8-9. , 188188. Vaquerizo B, Serra A, Ormiston J, Miranda-Guardiola F, Webber B, Fantuzzi A, Delgado G, Brugera J. Bench top evaluation and clinical experience with the szabo technique: New Questions for a Complex Lesion. Catheter Cardiovasc Interv: Feb 15;79:378-89 ].
- Preparation of left main ostial lesions with predilatation is frequently required: cutting balloons [189189. Okura H, Hayase M, Shimodozono S, Kobayashi T, Sano K, Matsushita T, Kondo T, Kijima M, Nishikawa H, Kurogane H, Aizawa T, Hosokawa H, Suzuki T, Yamaguchi T, Bonneau HN, Yock PG, Fitzgerald PJ. Mechanisms of acute lumen gain following cutting balloon angioplasty in calcified and noncalcified lesions: an intravascular ultrasound study. Catheter Cardiovasc Interv. 2002;57:429-36. ] may be considered, particularly for calcified lesions. The limited data in the available literature has suggested that this approach is safe and effective [190190. Erglis A, Narbute I, Kumsars I, Jegere S, Mintale I, Zakke I, Strazdins U, Saltups A. A randomised comparison of paclitaxel-eluting stents versus bare-metal stents for treatment of unprotected left main coronary artery stenosis. J Am Coll Cardiol. 2007;50:491-7. , 191191. Nassar H, Gotsman I, Gerganski P, Moseri M, Lotan C, Gotsman M. Cutting balloon angioplasty and stent implantation for aorto-ostial lesions: clinical outcome and 1-year follow-up. Clinical cardiology. 2009;32:183-6. ]. In addition, the previously described DELTA registry reported the use of cutting balloons in 8.9% (n=167/1, 874) of patients who underwent PCI for ULMCA disease, with no reported adverse sequelae [7474. Moynagh A, Salvatella N, Harb T, Darremont O, Boudou N, Dumonteil N, Lefèvre T, Carrié D, Louvard Y, Leymarie JL, Chevalier B, Morice MC. Two-year outcomes of Everolimus Vs. Paclitaxel-eluting stent for the treatment of unprotected left main lesions. A matched comparison of patients included in the French Left Main Taxus (FLM Taxus) and the LEft MAin Xience (LEMAX) registries. EuroIntervention. 2011 ;7:689-96. ].
- For an ostial lesion the stent usually needs to be implanted with slight protrusion (using the radiopaque markers of the deploying stent balloon) into the aorta to ensure adequate lesion coverage; any longer than this may compromise catheter re-engagement if a repeat procedure is performed. After stent deployment, the deploying balloon should be withdrawn slightly into the ascending aorta and the proximal part of the stent “flared” to ensure good stent apposition at the ostium ( Figure 37 ).
- The guide catheter needs to be completely disengaged from the LMS ostium before stent deployment to avoid being trapped by the stent, whilst simultaneously keeping the guide catheter close to the ostium to allow for contrast injection into the LMS ostium. Ensure that the stent position is not altered by guide catheter manipulation. Be aware that immediately after stent implantation the guide catheter may be sucked into the deployed stent during balloon deflation – the operator should take appropriate measures to control for this phenomenon and even use it to their advantage to allow reintubation of the left main ostium with the guide catheter in the knowledge that it would be unlikely to damage the ostial stent struts during reintubation.
- The LMS ostium is composed predominantly of elastic fibres which places it at a greater risk of recoil [3636. Farinha JB, Kaplan MA, Harris CN, Dunne EF, Carlish RA, Kay JH, Brooks S. Disease of the left main coronary artery. Surgical treatment and long-term follow up in 267 patients. Am J Cardiol. 1978;42:124-8. ]. If recoil occurs at the ostium, either post-dilatation with a non-compliant balloon or overlap stenting to cover the region may need to be undertaken. Be aware that excessive or overly aggressive dilatation at the ostium may induce dissection of the ascending aorta ( Figure 42 ).
- If a repeat procedure is performed after previous LMS ostial stenting, care should be taken to avoid damaging the ostial placed stent. Tips to avoid this complication include ensuring co-axial alignment of the guide catheter when intubating the LMS and/or passage of a (looped) coronary wire into the distal vessel before full cannulation of the LMS ostium ( Figure 43 ). In emergency situations, the coronary wire can be passed through an ostial placed stent cell and subsequently crushed to allow subsequent rapid access ( Figure 44 ).
Management of complications
Geographical miss of the LMS ostium invariably requires implantation of an overlapping stent at the LMS ostium to cover the LMS ostium ( Figure 45 ).
Proximal stent dislodgement (into the aortic root) of a left main stent can occur if not adequately deployed and it adheres to the deploying balloon during removal. A technique to overcome this problem is illustrated ( Figure 46 ).
Distal stent dislodgement (to the LMS distal bifurcation) can also occur immediately after implantation of ostial or mid LMS placed stents, thus uncovering the treated lesion. If this occurs, coverage of the more proximal LMS lesion with an overlapping stent can be undertaken along with more adequate KBPD into the distal LMS bifurcation ( Figure 47 ).
DISTAL (BIFURCATION) LMS LESIONS
Background
Approximately two thirds of significant ULM disease involves the distal bifurcation based on previous registry data [184184. Mehilli J, Kastrati A, Byrne RA, Bruskina O, Iijima R, Schulz S, Pache J, Seyfarth M, Massberg S, Laugwitz KL, Dirschinger J, Schomig A. Paclitaxel- versus sirolimus-eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2009;53:1760-8. ]. Recently, the distal bifurcation was noted in 81% and 88% of ULM disease treated with PCI in the EXCEL (including trifurcation) and NOBLE trial, respectively [287287. Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, Kandzari DE, Morice MC, Lembo N, Brown WM 3rd, Taggart DP, Banning A, Merkely B, Horkay F, Boonstra PW, van Boven AJ, Ungi I, Bogáts G, Mansour S, Noiseux N, Sabaté M, Pomar J, Hickey M, Gershlick A, Buszman P, Bochenek A, Schampaert E, Pagé P, Dressler O, Kosmidou I, Mehran R, Pocock SJ, Kappetein AP; EXCEL Trial Investigators. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med. 2016;375::2223-2235. , 288288. Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, Trovik T, Eskola M, Romppanen H, Kellerth T, Ravkilde J, Jensen LO, Kalinauskas G, Linder RB, Pentikainen M, Hervold A, Banning A, Zaman A, Cotton J, Eriksen E, Margus S, Sorensen HT, Nielsen PH, Niemela M, Kervinen K, Lassen JF, Maeng M, Oldroyd K, Berg G, Walsh SJ, Hanratty CG, Kumsars I, Stradins P, Steigen TK, Frobert O, Graham AN, Endresen PC, Corbascio M, Kajander O, Trivedi U, Hartikainen J, Anttila V, Hildick-Smith D, Thuesen L, Christiansen EH, investigators Ns. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388:2743-2752. ]. A meta-analysis of early, predominantly single-centre studies has previously confirmed that MACE and TVR were more prevalent in the distal LMS compared to the ostium or shaft of the LMS [192192. Biondi-Zoccai GG, Lotrionte M, Moretti C, Meliga E, Agostoni P, Valgimigli M, Migliorini A, Antoniucci D, Carrie D, Sangiorgi G, Chieffo A, Colombo A, Price MJ, Teirstein PS, Christiansen EH, Abbate A, Testa L, Gunn JP, Burzotta F, Laudito A, Trevi GP, Sheiban I. A collaborative systematic review and meta-analysis on 1278 patients undergoing percutaneous drug-eluting stenting for unprotected left main coronary artery disease. Am Heart. 2008;155:274-83. ].
Within the LMS PCI subset from the SYNTAX trial, the finding of two thirds of LMS disease affecting the distal bifurcation was confirmed, with Medina Classification 1.1.1, 1.0.0 and 1.1.0 being the most common patterns of disease ( Figure 48 and Figure 49 and Figure 50 ) [2727. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-53.
The analysis from the randomised SYNTAX trial demonstrating comparable clinical outcomes in patients with ULMCA disease - with low-moderate SXscores - who under-went surgical or percutaneous revascualrisation. This ultimately formed the basis for the EXCEL hypo-thesis and the subsequent ongoing EXCEL trial., 193193. Mohr Friedrich SP, Hamm Christian & Robert Jones. The SYNergy between Percutaneous Coronary Intervention and Cardiac Surgery (SYNTAX) Study. ESC Congress 2008. Munich, Germany. European Society of Cardiology. ]. Within the SYNTAX trial, over one half of the patients with distal LMS bifurcation disease were treated with the provisional T-stenting approach, with a one-stent treatment being successfully performed in 89% of these cases ( Figure 50 ) [2828. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. ]. In addition, a non-significant trend towards a greater incidence of MACCE was evident with the 2-stent compared to the one-stent approach ( Figure 51 ). Supporting these latter findings, Palmerini et al [194194. Palmerini T, Marzocchi A, Tamburino C, Sheiban I, Margheri M, Vecchi G, Sangiorgi G, Santarelli A, Bartorelli A, Briguori C, Vignali L, Di Pede F, Ramondo A, Inglese L, De Carlo M, Falsini G, Benassi A, Palmieri C, Filippone V, Sangiorgi D, Barlocco F, De Servi S. Impact of bifurcation technique on 2-year clinical outcomes in 773 patients with distal unprotected left main coronary artery stenosis treated with drug-eluting stents. Circ Cardiovasc Interv. 2008;1:185-92. ] demonstrated in a retrospective, observational, multicentre registry of 773 patients in 19 high-volume centres in Italy, who underwent PCI to distal ULMCA disease with DES, that the provisional strategy limited to one stent was associated with improved event-free survival at 2 years, compared to a 2-stent strategy. Furthermore, other studies have also confirmed the “simple is better” approach to be safer, with centres using dedicated 2-stent techniques being shown to have higher MACE and TLR rates compared to centres using the provisional or single-stent approach [195195. Chieffo A, Stankovic G, Bonizzoni E, Tsagalou E, Iakovou I, Montorfano M, Airoldi F, Michev I, Sangiorgi MG, Carlino M, Vitrella G, Colombo A. Early and mid-term results of drug-eluting stent implantation in unprotected left main. Circulation. 2005;111:791-5. , 196196. Price MJ, Cristea E, Sawhney N, Kao JA, Moses JW, Leon MB, Costa RA, Lansky AJ, Teirstein PS. Serial angiographic follow-up of sirolimus-eluting stents for unprotected left main coronary artery Revascularisation. J Am Coll Cardiol. 2006;47:871-7. , 197197. Valgimigli M, Malagutti P, Rodriguez-Granillo GA, Garcia-Garcia HM, Polad J, Tsuchida K, Regar E, Van der Giessen WJ, de Jaegere P, De Feyter P, Serruys PW. Distal left main coronary disease is a major predictor of outcome in patients undergoing percutaneous intervention in the drug-eluting stent era: an integrated clinical and angiographic analysis based on the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated At Rotterdam Cardiology Hospital (T-SEARCH) registries. J Am Coll Cardiol. 2006;47:1530-7. , 198198. Valgimigli M, Malagutti P, Rodriguez Granillo GA, Tsuchida K, Garcia-Garcia HM, van Mieghem CA, Van der Giessen WJ, De Feyter P, de Jaegere P, Van Domburg RT, Serruys PW. Single-vessel versus bifurcation stenting for the treatment of distal left main coronary artery disease in the drug-eluting stenting era. Clinical and angiographic insights into the Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated at Rotterdam Cardiology Hospital (T-SEARCH) registries. Am Heart J. 2006;152:896-902. , 199199. Park SJ, Kim YH, Lee BK, Lee SW, Lee CW, Hong MK, Kim JJ, Mintz GS, Park SW. Sirolimus-eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005;45:351-6. , 200200. Vaquerizo B, Lefevre T, Darremont O, Silvestri M, Louvard Y, Leymarie JL, Garot P, Routledge H, de Marco F, Unterseeh T, Zwahlen M, Morice MC. Unprotected left main stenting in the real world: two-year outcomes of the French left main taxus registry. Circulation. 2009;119:2349-56. , 201201. Price MJ, Kandzari DE, Teirstein PS. Change we can believe in: the hyper-evolution of percutaneous coronary intervention for unprotected left main disease with drug-eluting stents. Circ Cardiovasc Interv. 2008;1:164-6. ]. In the recent EXCEL trial, among 529 patients undergoing planned distal LM PCI, 344 (65.0%) and 185 (35.0%) were treated with intended 1-stent provisional and planned 2-stent techniques, respectively. Three-year adverse outcomes were worse with planned 2-stent treatment compared with a provisional 1-stent approach in line with previous reports [296296. Kandzari DE, Gershlick AH, Serruys PW, Leon MB, Morice MC, Simonton CA, Lembo NJ, Banning AP, Merkely B, van Boven AJ, Ungi I, Kappetein AP, Sabik JF, 3rd, Genereux P, Dressler O, Stone GW. Outcomes Among Patients Undergoing Distal Left Main Percutaneous Coronary Intervention. Circ Cardiovasc Interv 2018;11:e007007. ].
Conversely, a large single centre Chinese registry study examining comparisons between one- (n = 661) and two-stent (n = 372) strategies for distal unprotected left main coronary bifurcation disease and low-intermediate SYNTAX scores (i.e. <33), demonstrated similar MACE (a composite of death, MI, and target vessel revascularization) at a mean 4 year follow-up (one stent: 9.2% vs. two stents: 11.6%, P = 0.23). [267267. Gao Z, Xu B, Yang Y, Qiao S, Wu Y, Chen T, Xu L, Yuan J, Chen J, Gao RL.
Comparison between one-stent versus two-stent technique for treatment of left main bifurcation lesions: A large single-center data. Catheter Cardiovasc Interv. [Epub ahead of print]] Moreover, the two stent technique was shown not to be an independent risk predictor of MACE. Furthermore, propensity matching of 198 matched patients demonstrated similar outcomes of death (4.6% vs. 2.5%, P = 0.29), MI (6.1% vs. 10.6%, P = 0.08), and definite and probable stent thrombosis (3.0% vs. 2.0%, P = 0.52), with a significantly higher incidence of TVR in the two-stent technique group (5.6% vs. 10.6%, P = 0.05).
Currently, DKCRUSH-V trial directly compared a double-kissing crush two-stent strategy with provisional stenting of the main branch in 482 patients with distal LM bifurcation disease. Double-kissing crush resulted in a lower risk of target lesion failure at 1 year compared with provisional stenting [297297. Chen SL, Zhang JJ, Han Y, Kan J, Chen L, Qiu C, Jiang T, Tao L, Zeng H, Li L, Xia Y, Gao C, Santoso T, Paiboon C, Wang Y, Kwan TW, Ye F, Tian N, Liu Z, Lin S, Lu C, Wen S, Hong L, Zhang Q, Sheiban I, Xu Y, Wang L, Rab TS, Li Z, Cheng G, Cui L, Leon MB, Stone GW. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol. 2017;70::2605-2617. ].
Choice of strategy to perform unprotected left main PCI
The choice of strategy in performing ULM PCI is based on vessel and lesion characteristics as well operator experience. In particular, important consideration of the anatomy of the SideB is required, such as the presence of significant SideB stenosis, the presence of significant SideB disease beyond the ostium, SideB angulation and size of LAD with respect to the LCx. In most cases, a single-stent approach is required. Guidance as to when to use a 2-stent approach and which technique to use is illustrated in a simplified treatment algorithm ( Figure 52 ). Furthermore, the choice of which 2-stent strategy to use in ULM PCI – namely T-stent, crush or V stenting – has not been shown to affect 2-year survival or MACE in the same Italian registry described in the last section (Palmerini et al) [194194. Palmerini T, Marzocchi A, Tamburino C, Sheiban I, Margheri M, Vecchi G, Sangiorgi G, Santarelli A, Bartorelli A, Briguori C, Vignali L, Di Pede F, Ramondo A, Inglese L, De Carlo M, Falsini G, Benassi A, Palmieri C, Filippone V, Sangiorgi D, Barlocco F, De Servi S. Impact of bifurcation technique on 2-year clinical outcomes in 773 patients with distal unprotected left main coronary artery stenosis treated with drug-eluting stents. Circ Cardiovasc Interv. 2008;1:185-92. ]. Conversely, the recent reported double kissing crush technique (described below) has been reported to be associated with significantly reduced MACE, predominantly secondary to reduced TVR ( Figure e11a Figure e11b and Figure e11c ), when compared to culotte stenting and provisional stenting in the multicenter, randomised, prospective DKCRUSH-III and DKCRUSH-V trial, respectively. [268268. Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, Kwan TW, Paiboon C, Zhou YJ, Lv SZ, Dangas GD, Xu YW, Wen SY, Hong L, Zhang RY, Wang HC, Jiang TM, Wang Y, Chen F, Yuan ZY, Li WM, Leon MB. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61:1482-8 , 297297. Chen SL, Zhang JJ, Han Y, Kan J, Chen L, Qiu C, Jiang T, Tao L, Zeng H, Li L, Xia Y, Gao C, Santoso T, Paiboon C, Wang Y, Kwan TW, Ye F, Tian N, Liu Z, Lin S, Lu C, Wen S, Hong L, Zhang Q, Sheiban I, Xu Y, Wang L, Rab TS, Li Z, Cheng G, Cui L, Leon MB, Stone GW. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol. 2017;70::2605-2617. ]
A more evidence-based classification system in undertaking PCI of coronary bifurcations is the MADS classification proposed by the European Bifurcation Club ( Figure 53 ) [202202. Louvard Y, Thomas M, Dzavik V, Hildick-Smith D, Galassi AR, Pan M, Burzotta F, Zelizko M, Dudek D, Ludman P, Sheiban I, Lassen JF, Darremont O, Kastrati A, Ludwig J, Iakovou I, Brunel P, Lansky A, Meerkin D, Legrand V, Medina A, Lefevre T. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008;71:175-83. , 203203. Louvard Y, Medina A, Stankovic G. Definition and classification of bifurcation lesions and treatments. EuroIntervention. 2010;6 Suppl J:J31-5. , 204204. Thomas M, Hildick-Smith D, Louvard Y, Albiero R, Darremont O, Stankovic G, Pan M, Legrand V, Debruyne B, Lefevre T. Percutaneous coronary intervention for bifurcation disease.A consensus view from the first meeting of the European Bifurcation Club. EuroIntervention. 2006;2:149-53. ]. This practical-based classification system describes the strategy implemented by the operator after implantation of the first stent, and the subsequent potential implantation of additional stents in accordance with the proposed treatment plan and the results/difficulties encountered. In GLOBAL LEADERS trial, 22,921 lesions treated at the index and staged procedure were available for analysis and 2,757 of these lesions were bifurcations and 7 were trifurcation lesions. The e-CRF-based MADS classification was achieved in 2,757 of these lesions (100%). [298298. Katsikis A, Chichareon P, Cavalcante R, Collet C, Modolo R, Onuma Y, Stankovic G, Louvard Y, Vranckx P, Valgimigli M, Windecker S, Serruys PW. Application of the MADS classification system in a "mega mammoth" stent trial: Feasibility and preliminary clinical implications. Catheter Cardiovasc Interv. 2019;93:57-63. ]
Kissing balloon post dilatation (KBPD)
- Single-stent technique
Kissing balloon post dilatation (KBPD) is generally recommended following the single-stent (provisional T-stenting) approach. The randomised Nordic-Baltic Bifurcation Study III [154154. Niemela M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Kumsars I, Jegere S, Dombrovskis A, Gunnes P, Stavnes S, Steigen TK, Trovik T, Eskola M, Vikman S, Romppanen H, Makikallio T, Hansen KN, Thayssen P, Aberge L, Jensen LO, Hervold A, Airaksinen J, Pietila M, Frobert O, Kellerth T, Ravkilde J, Aaroe J, Jensen JS, Helqvist S, Sjogren I, James S, Miettinen H, Lassen JF, Thuesen L. Randomised comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123:79-86. ] (n=477) did, however, question this recommendation as similar clinical outcomes were observed in patients who did (n=238) or did not (n=239) undergo final KBPD after MainB stenting in the single-stent bifurcation approach; final KBPD was however shown to reduce angiographic SideB (re)stenosis, particularly in patients with true bifurcation lesions. Notably, this study did not specifically assess the left main, with approximately 7-8% of patients undergoing ULM PCI. In addition, the longer-term risks of stent thrombosis from not performing final KBPD have not yet been reported. In the author’s opinion, it would therefore still perhaps not be unreasonable to perform final KBPD in the context of a single-stent approach when undertaking ULM PCI. Furthermore, as previously discussed, the option of further adjunctive imaging/adjunctive tools can be considered to assess the haemodynamic status of the SideB if required.
Within the context of the left main, long term outcomes of 105 consecutive patients treated with simple crossover stenting from the left main to the left anterior descending coronary artery (in the absence of angiographically significant ostial left circumflex disease) and without opening of the struts in the left circumflex ostium, demonstrated acceptable longer-term (3-year) clinical outcomes. Specifically, MACE 9.7%, cardiac death 2.2%, myocardial infarction 2.2% and target lesion revascularization 8.6%. Notably, ‘pure’ ostial LCX-related repeat revascularization was required in only two patients. [269269. Lee HM, Nam CW, Cho YK, Yoon HJ, Park HS, Kim H, Chung IS, Heo YS, Hur SH, Kim YN, Kim KB. Long-term outcomes of simple crossover stenting from the left main to the left anterior descending coronary artery. Korean J Intern Med. 2014;29:597-602 ]. These findings are supported by Kang et al, demonstrating that in LMCA bifurcation lesions with mild LCX ostial disease, the use of single-stent technique rarely resulted in the functional LCX compromise. [270270. Kang SJ, Ahn JM, Kim WJ, Lee JY, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Functional and morphological assessment of side branch after left main coronary artery bifurcation stenting with cross-over technique. Catheter Cardiovasc Interv. 2014;83:545-52 ]. An explanation for these findings may relate to the fact that the left main to left circumflex angulation is more perpendicular and therefore less susceptible to carina shift [138138. Farooq V, Okamura T, Onuma Y, Gogas BD, Serruys PW. Unravelling the complexities of the coronary bifurcation: is this raising a few eyebrows? EuroIntervention: 2012;7:1133-41. , 140140. Farooq V, Serruys PW, Heo JH, Gogas BD, Okamura T, Gomez-Lara J, Brugaletta S, Garcìa-Garcìa HM, van Geuns RJ. New Insights Into the Coronary Artery Bifurcation. Hypothesis-Generating Concepts Utilizing 3-Dimensional Optical Frequency Domain Imaging. JACC Cardiovasc Interv. 2011;4:921-931. ].
- Double-stent technique
As with non-LMS bifurcation disease, when two stents are used in unprotected distal LMS PCI, KBPD with non-compliant balloons should be performed in practically all circumstances [205205. Ge L, Airoldi F, Iakovou I, Cosgrave J, Michev I, Sangiorgi GM, Montorfano M, Chieffo A, Carlino M, Corvaja N, Colombo A. Clinical and angiographic outcome after implantation of drug-eluting stents in bifurcation lesions with the crush stent technique: importance of final kissing balloon post-dilation. Am J Cardiol. 2005;46:613-20. , 206206. Costa RA, Mintz GS, Carlier SG, Lansky AJ, Moussa I, Fujii K, Takebayashi H, Yasuda T, Costa JR, Jr., Tsuchiya Y, Jensen LO, Cristea E, Mehran R, Dangas GD, Iyer S, Collins M, Kreps EM, Colombo A, Stone GW, Leon MB, Moses JW. Bifurcation coronary lesions treated with the crush technique: an intravascular ultrasound analysis. Am J Cardiol. 2005;46:599-605. , 207207. Ormiston JA, Currie E, Webster MW, Kay P, Ruygrok PN, Stewart JT, Padgett RC, Panther MJ. Drug-eluting stents for coronary bifurcations: insights into the crush technique. Catheter Cardiovasc Interv. 2004;63:332-6. , 208208. Murasato Y. Impact of three-dimensional characteristics of the left main coronary artery bifurcation on outcome of crush stenting. Catheter Cardiovasc Interv. 2007;69:248-56. , 209209. Dzavik V, Kharbanda R, Ivanov J, Ing DJ, Bui S, Mackie K, Ramsamujh R, Barolet A, Schwartz L, Seidelin PH. Predictors of long-term outcome after crush stenting of coronary bifurcation lesions: importance of the bifurcation angle. Am Heart J. 2006;152:762-9. ]. Furthermore, a 2–step KBPD approach – high pressure (>20 atm) post dilatation of the SideB ostium with a non-compliant balloon, 0.25 mm smaller in diameter than nominal SB diameter, followed by final KBPD (8-10 atm) to correct any stent distortion – has been shown to minimise ostial SideB stenosis after crush stenting in bench testing, [210210. Ormiston JA, Webster MW, Webber B, Stewart JT, Ruygrok PN, Hatrick RI. The crush technique for coronary artery bifurcation stenting: insights from micro-computed tomographic imaging of bench deployments. JACC Cardiovasc Interv. 2008;1:351-7. ] and should ideally be the preferred technique.
Guide catheter sizing
Whenever performing LMS bifurcation intervention, important consideration must be given to the sizing of the hardware to ensure that the operator is not faced with situations where they cannot advance 2 stents. Internal diameters of guide catheters vary, based not only on the French size but also on the manufacturer, and the operator must ensure that the guide catheter is capable of delivering the hardware needed to undertake the procedure safely. As a generalised, simplified rule, a 6 Fr guide catheter can simultaneously accommodate a single angioplasty balloon and stent, and a 7 Fr catheter 2 stents.
Single-stent technique
Provisional T-stent technique
The provisional T-stenting ( Figure 54 and Figure 55A ) approach is a single-stent strategy that allows for the placement of a second stent – utilising other techniques such as T-stenting, TAP technique, culotte or reverse crush – if SideB stenting is required [211211. Iakovou I, Ge L, Colombo A. Contemporary stent treatment of coronary bifurcations. J Am Coll Cardiol. 2005;46:1446-55. ]. A coronary wire is passed into the MainB (usually the LAD) and SideB. Cross-over stenting (LMS-LAD) is undertaken and post-dilation performed as required.
The appearance of the ostial LCx is reassessed and may be left untouched or treated by KBPD previously discussed. Furthermore, given the poor correlation between angiographic appearances of the SideB ostium and haemodynamic compromise, [133133. Koh JS, Koo BK, Kim JH, Yang HM, Park KW, Kang HJ, Kim HS, Oh BH, Park YB. Relationship Between Fractional Flow Reserve and Angiographic and Intravascular Ultrasound Parameters in Ostial Lesions: Major Epicardial Vessel vs. Side Branch Ostial Lesions. JACC Cardiovasc Interv. In Press 2012. , 134134. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB, Choi YS, Tahk SJ. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633-7. , 135135. Nam CW, Hur SH, Koo BK, Doh JH, Cho YK, Park HS, Yoon HJ, Kim H, Chung IS, Kim YN, Fearon WF, Tahk SJ, Kim KB. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ J. 2011;41:304-7. , 136136. Farooq V, Heo JH, Raber L, Brugaletta S, Radu M, Gogas BD, Diletti R, Onuma Y, Garcia-Garcia HM, Serruys PW. Tools & techniques: risk stratification and diagnostic tools in left main stem intervention. EuroIntervention. 2011;7:747-53. , 137137. Kang SJ, Mintz GS, Kim WJ, Lee JY, Oh JH, Park DW, Lee SW, Kim YH, Lee CW, Park SW, Park SJ. Changes in left main bifurcation geometry after a single-stent crossover technique: an intravascular ultrasound study using direct imaging of both the left anterior descending and the left circumflex coronary arteries before and after intervention. Circ Cardiovasc Interv. 2011;4:355-61. ] alternative assessment of the SideB may be required with adjunctive intravascular imaging or FFR as previously discussed. If necessary, a second stent may need to be deployed. KBPD is mandatory to complete the procedure if a two-stent technique is adopted.
Techniques to reduce the risk of carina shift and SideB closure during the provisional T-stenting approach include the proximal optimisation technique (POT), [156156. Hildick-Smith D, Lassen JF, Albiero R, Lefevre T, Darremont O, Pan M, Ferenc M, Stankovic G, Louvard Y. Consensus from the 5th European Bifurcation Club meeting. EuroIntervention. 2010;6:34-8. , 212212. Lefevre T, Darremont O, Albiero R. Provisional side branch stenting for the treatment of bifurcation lesions. EuroIntervention. 2010;6 Suppl J:J65-71. ] to avoid SideB compromise by sizing the stent diameter to the distal MainB diameter and post-dilating more proximally, and to facilitate coronary rewiring of the SideB and allow for appropriate stent apposition at the SideB ostium as illustrated ( Figure 55B ).
Skirt technique
The Skirt technique is a technique to treat distal LMCA disease when the disease does not affect the LAD or LCx ostia (i.e., Medina 1, 0, 0 disease), in the presence of a more acute bifurcation angle ( Figure 56 ). After implantation of the stent, KBPD is performed with close attention paid to ensure that the angioplasty balloons remain within the confines of the stent.
Double-stent techniques
Culotte stent technique
This is a strategy suitable for lesions where the ostium of the SideB (usually the LCx) is diseased, the angulation between the vessels is <60° (to minimise the risk of carina and plaque shift) and, importantly, the 2 vessels are of similar diameter ( Figure 57 and Figure 58 ).
The more angulated branch (usually the SideB: LMS-LCx) is first stented with the consequent jailing of a second previously placed coronary wire in the straighter branch (usually the MainB: LMS-LAD) ( Figure 57 ). At this stage, rewiring of the LMS to LAD is required; it is, however, crucial to ensure that the coronary wire is passed through the true lumen of the LMS portion of the LMS-LCx stent into the LAD (and not behind the stent if underdeployed). The operator may wish to go blind and predilate the LMS-LAD with a large balloon if he/she is confident with regard to the wire positioning or use intravascular imaging. Intravascular imaging can facilitate this process by imaging the LMS-LCx stent to ensure full stent apposition of the LMS portion of the LMS-LCx stent: importantly, this should be performed using the LMS-LCx coronary wire. Thereafter, the procedure is completed with predilatation of the LMS-LAD, removal of the jailed LMS-LAD wire, deployment of the LMS-LAD stent overlapping more proximally with the LMS-LCx stent, and KBPD to complete as illustrated. An actual case employing this technique is illustrated ( Figure 58 ).
This technique provides an optimal reconstruction of the distal left main bifurcation but with a significant area of stent overlap. The use of a new generation of stents with open cells facilitates this technique.
T-stent technique
The T-stent strategy ( Figure 59 and Figure 60 ) is used when a 2-stent strategy is required and the angulation between both LMS branches (MainB and SideB) approaches 90°.
This technique provides a good reconstruction of a T-shaped distal LMS bifurcation. The main risks are those of incomplete ostial coverage (if the SideB stent is deployed too distally) and the subsequent risk of restenosis, or of deploying the SideB stent too proximally and therefore leading to excessive protrusion into the LMS stent (and thus requiring a subsequent crush to correct). The metallic markers of the deploying balloon of the stent should be used to ensure that the SideB stent is just protruding into the LMS, in order to ensure appropriate stent positioning. A modified version of the T-stent technique can also be considered ( Figure 61 ).
Mini-crush stent technique
The mini-crush technique [213213. Galassi AR, Tomasello SD, Capodanno D, Barrano G, Ussia GP, Tamburino C. Mini-Crush Versus T-Provisional Techniques in Bifurcation Lesions: Clinical and Angiographic Long-Term Outcome After Implantation of Drug-Eluting Stents. JACC Cardiovasc Interv. 2009;2:185-194. ] ( Figure 62 and Figure 63) has largely replaced the standard crush technique [211211. Iakovou I, Ge L, Colombo A. Contemporary stent treatment of coronary bifurcations. J Am Coll Cardiol. 2005;46:1446-55. ] since it has the advantage of leading to a reduced area of overlapping stent struts.
To perform mini-crush stenting ( Figure 62 ) the SideB is first stented (usually LCx-LMS) by positioning the SideB stent to allow for minimal protrusion into the LMS through the use of the deploying balloon markers, whilst simultaneously positioning the MainB stent (usually LMS – LAD) to cover the protrusion into the MainB. Next, the MainB is stented. Deployment of the MainB stent crushes the proximal SideB stent against the LMS wall. Subsequently, the LCx is rewired through the stent struts of the LAD and crushed LCx stent in order to perform post-dilatation of the SideB ostium (and clearance of struts) followed by a final KBPD [213213. Galassi AR, Tomasello SD, Capodanno D, Barrano G, Ussia GP, Tamburino C. Mini-Crush Versus T-Provisional Techniques in Bifurcation Lesions: Clinical and Angiographic Long-Term Outcome After Implantation of Drug-Eluting Stents. JACC Cardiovasc Interv. 2009;2:185-194. , 214214. Kornowski R. The mini-crush technique for managing bifurcation lesions. Catheter Cardiovasc Interv. 2009;74:85-7. , 215215. Galassi AR, Tomasello SD, Sacchetta G, Seminara D, Canonico L, Tamburino C. The mini-crush technique for the treatment of coronary trifurcation lesions. EuroIntervention. 2008;4:358-64. ].
One note of caution is that although KBPD of a single (MainB) stent approach produces the best scaffolding of the SideB ostium if the wire crosses into the SideB through the distal struts at the SideB ostium, when re-crossing the SideB after MainB stenting during the mini-crush the reverse holds true, [210210. Ormiston JA, Webster MW, Webber B, Stewart JT, Ruygrok PN, Hatrick RI. The crush technique for coronary artery bifurcation stenting: insights from micro-computed tomographic imaging of bench deployments. JACC Cardiovasc Interv. 2008;1:351-7. ] namely that distal crossing is more likely to result in gaps in the stent coverage at the SideB ostium. A potential tip to avoid this complication is to rewire the SideB during mini-crush with a proximal passage of the coronary wire: this will increase the chances of the coronary wire entering the SideB through a more based proximal cell [212212. Lefevre T, Darremont O, Albiero R. Provisional side branch stenting for the treatment of bifurcation lesions. EuroIntervention. 2010;6 Suppl J:J65-71. , 216216. Burzotta F, De Vita M, Sgueglia G, Todaro D, Trani C. How to solve difficult side branch access? EuroIntervention. 2010;6 Suppl J:J72-80. ].
T-stenting and Protrusion (TAP) technique
This technique can be used in the majority of the bifurcation lesions ( Figures 64 and Figure 65 ). It can provide a good reconstruction of distal LMS bifurcation with minimal stent overlap. The main drawback of this technique is that it leads to the formation of a metallic neocarina; conversely, it is technically less difficult to perform ( Figure 70 ). The MainB (usually LMS-LAD) is stented. Next, predilatation of the LMS-LCx through the stent struts is performed to clear any struts at the SideB (LCx) ostium, followed by the passage of a stent to the ostium of the SideB with a balloon left in the MainB stent. The proximal edge of the SideB stent is positioned inside the MainB by ensuring the metallic markers of the deploying stent balloon are located in the LMS at about the level of the SideB orifice. The SideB stent is subsequently delivered at high pressure, whilst a deflated balloon is left in the MainB stent. To finish, a final KBPD is performed in order to reshape the carina ( Figure 64 and Figure 65 ) [217217. Burzotta F, Gwon HC, Hahn JY, Romagnoli E, Choi JH, Trani C, Colombo A. Modified T-stenting with intentional protrusion of the side-branch stent within the main vessel stent to ensure ostial coverage and facilitate final kissing balloon: the T-stenting and small protrusion technique (TAP-stenting). Report of bench testing and first clinical Italian-Korean two-centre experience. Catheter Cardiovasc Interv. 2007;70:75-82. ].
V-stent technique
The V-stent technique (or “kissing stent” technique) ( Figure 66 and Figure 67 ) is suitable in similar situations to the crush technique. Its main use is in Medina 0, 1, 1 lesions. Importantly, the LMS should be able to accommodate 2 stents (ostially placed in the LAD and LCx) abutting each other at the carina ( Figure 66B ).
Simultaneous kissing stent (SKS) technique
A variant of the V stenting technique is the simultaneous kissing stent (SKS) technique, also known as “shotgun” stenting ( Figure 66 and Figure 67 ) [218218. Morton AC, Siotia A, Arnold ND, Korgul P, Bowles J, Heppenstall J, Gunn J. Simultaneous kissing stent technique to treat left main stem bifurcation disease. Catheter Cardiovasc Interv. 2007;69:209-15. , 219219. Brett S, Gunn J. Shotgun stenting of the left main coronary artery bifurcation. Heart 2006;92:310-. , 220220. Brett S, Gunn J. Images in cardiology. Shotgun stenting of the left main coronary artery bifurcation. Heart 2006;92:310. , 221221. Kim YH, Park DW, Suh IW, Jang JS, Hwang ES, Jeong YH, Lee SW, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. Long-term outcome of simultaneous kissing stenting technique with sirolimus-eluting stent for large bifurcation coronary lesions. Catheter Cardiovasc Interv. 2007;70:840-6. ]. This technique consists of creating a long metallic neocarina with a double lumen (double barrel) in the LMS ( Figure 66B ). It is mainly recommended for use in disease affecting the entire bifurcation with a very large LMS and a major difference in diameters compared to the two SideBs. The main limitation of this technique is that the double layer at the centre of the vessel may make future intervention difficult.
Summary of technical difficulty, location and number of metallic layers and formation of metallic neocarina with differing bifurcation procedures
( Figure 68 and Figure 70 ) illustrate these concepts.
Double Kissing Crush (DK-crush) technique
As previously discussed, the kissing crush (DK-crush) technique has been shown to be associated with improved clinical outcomes when compared to Culotte stenting and provisional stenting in the randomised DKCRUSH-III trial ( Figure e11a Figure e11b and Figure e11c ) and DKCRUSH V trial, respectively. [268268. Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, Kwan TW, Paiboon C, Zhou YJ, Lv SZ, Dangas GD, Xu YW, Wen SY, Hong L, Zhang RY, Wang HC, Jiang TM, Wang Y, Chen F, Yuan ZY, Li WM, Leon MB. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61:1482-8 , 297297. Chen SL, Zhang JJ, Han Y, Kan J, Chen L, Qiu C, Jiang T, Tao L, Zeng H, Li L, Xia Y, Gao C, Santoso T, Paiboon C, Wang Y, Kwan TW, Ye F, Tian N, Liu Z, Lin S, Lu C, Wen S, Hong L, Zhang Q, Sheiban I, Xu Y, Wang L, Rab TS, Li Z, Cheng G, Cui L, Leon MB, Stone GW. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol. 2017;70::2605-2617. ] A schematic description of the DK-crush and Culotte stenting techniques used in the DK-CRUSH-III study is illustrated (Fig. e12). In brief, DK-crush is performed as follows: [268268. Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, Kwan TW, Paiboon C, Zhou YJ, Lv SZ, Dangas GD, Xu YW, Wen SY, Hong L, Zhang RY, Wang HC, Jiang TM, Wang Y, Chen F, Yuan ZY, Li WM, Leon MB. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61:1482-8 , 271271. Chen SL, Santoso T, Zhang JJ, Ye F, Xu YW, Fu Q, Kan J, Paiboon C, Zhou Y, Ding SQ, Kwan TW. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol. 57 (2011), pp. 914–920 , 272272. Chen SL, Ye F, Zhang JJ, Zhu ZS, Lin S, Shan SJ, Liu ZZ, Liu Y, Duan BX, Ge JB. DK crush technique: modified treatment of bifurcation lesions in coronary artery. Chin Med J (Engl). 2005;118:1746 –50. ]
- SideB stenting
- Balloon crush
- Alternative SideB inflation with a noncompliant balloon at high pressure (≥16 atm) followed by first kissing balloon inflation
- MainB stenting
- Alternative SideB inflation with a noncompliant balloon at high pressure (≥16 atm) followed by final kissing balloon inflation
Dedicated bifurcation devices
The use of dedicated bifurcation devices to undertake left main intervention include the TRYTON side-branch stent ( Figure e13 ), in conjunction with a conventional stent (usually a DES) in a “reverse culotte” technique [222222. Magro M, van Geuns RJ. TheTryton side branch stent. EuroIntervention. 2010;6 Suppl J:J147-50. ]. Early retrospective registry experience has been encouraging [223223. Magro M, Bartorelli A, Lesiak M, Simsek C, Almeida M, Foley D, Serruys P.W, van Geuns RJ. Acute Procedural Outcome in Patients Treated with a Dedicated Bifurcation Stent for Left Main Stem Disease – The TRYTON LM Multicentre Registry. Presented at TCT, San Francisco, United States, 2011. ]. A prospective multicentre registry of 52 consecutive patients with left main disease treated in nine European centres has recently been reported. [273273. Magro M, Girasis C, Bartorelli AL, Tarantini G, Russo F, Trabattoni D, D’Amico G, Galli M, Gómez Juame A, de Sousa Almeida M, Simsek C, Foley D, Sonck J, Lesiak M, Kayaert P, Serruys PW, van Geuns RJ. Acute procedural and six-month clinical outcome in patients treated with a dedicated bifurcation stent for left main stem disease: the TRYTON LM multicentre registry. EuroIntervention. 2013;8:1259-69 ] Fifty-one of 52 patients were successfully treated with the Tryton stent, with final kissing balloon dilatation performed in 48/51 (94%) cases. The procedural success rate was reported at 94%, with acute gain of 1.52±0.86 mm in the left main and 0.92±0.47 mm in the side branch. Peri-procedural MI occurred in three patients. Six-month hierarchical MACE, TLR, MI and cardiac death were reported as 22%, 12%, 10% and 2% respectively. No cases of definite stent thrombosis were reported. Other dedicated bifurcation devices have been reported in the left main [224224. Hasegawa T, Ako J, Koo BK, Miyazawa A, Sakurai R, Chang H, Dens J, Verheye S, Grube E, Honda Y, Fitzgerald PJ. Analysis of left main coronary artery bifurcation lesions treated with biolimus-eluting DEVAX AXXESS plus nitinol self-expanding stent: intravascular ultrasound results of the AXXENT trial. Catheter Cardiovasc Interv. 2009;73:34-41. , 225225. Dubois CL, Wijns W. The AXXESS self-expanding biolimus A9 eluting stent system for coronary bifurcation lesions. EuroIntervention. 2010;6 Suppl J:J130-4. , 226226. Gil RJ, Vassiliev D, Michalek A, Kern A, Formuszewicz R, Dobrzycki S, Lesiak M, Wojcik J, Kardaszewicz P, Lekston A. First-in-man study of paclitaxel-eluting stent BiOSS (Bifurcation Optimisation Stent System) dedicated for coronary bifurcation stenoses: three months results. Kardiologia polska. 2012;70:45-52. ]. Regarding the BioSS LIM C sirolimus-eluting bifurcation dedicated stent, the POLBOS LM study is ongoing, which is a single-arm prospective multi-centre study enrolling 260 patients (SYNTAX score ≤32) with pre-specified performance goal based on the results of the EXCEL trial with contemporary percutaneous coronary intervention (PCI) for LMCA disease (NCT03508219).
Trifurcation disease
Within the SYNTAX trial, over one fifth (20.1%) of distal LMS lesions in the LMS PCI subset had trifurcation lesions [193193. Mohr Friedrich SP, Hamm Christian & Robert Jones. The SYNergy between Percutaneous Coronary Intervention and Cardiac Surgery (SYNTAX) Study. ESC Congress 2008. Munich, Germany. European Society of Cardiology. ]. The practical approach to treating this lesion subset is to avoid 3-vessel trifurcation stenting due to the potential risk of multiple stent layering and compression/crushing of vessels, as simultaneous triple kissing balloon inflation is technically more challenging to perform, and requires larger guide catheters (e.g., 8 Fr) or even the use of 2 guide catheters [227227. Ramcharitar S, Vaina S, Serruys PW, Sianos G. Treatment of a distal left main trifurcation supported by the TandemHeart left ventricular assist device. Hellenic journal of cardiology. 2007;48:110-4. , 228228. Dubois CL, Sinnaeve PR, Desmet WJ. Simultaneous triple kissing stenting in an unprotected left main coronary artery. Eur Heart J. 2006;27:1897. , 229229. Tamburino C, Tomasello SD, Capodanno D, Di Salvo ME, Marza F, Ruggero Galassi A. Long-term follow-up after drug eluting stent implantation in left main trifurcations. EuroIntervention. 2009;5:432-7. , 230230. Testa L, Bedogni F. How should I treat a coronary traffic jam? A triple kissing balloon in distal left main trifurcation. EuroIntervention. 2011;6:1011-6. ]. Instead, reliance on the “simple is better” approach is recommended, with an up-front 1 or 2 stent technique, depending on the pattern of disease, usually treating the LAD and the larger branch (LCx or intermediate branch). KBPD is generally recommended with post-dilatation of the third branch if needed to ensure that it is not haemodynamically compromised.
Notably data from SYNTAX ( Figure e13 ) demonstrated that although the presence of ULMCA disease to show a trend towards being protective against late/very late (beyond 30 days) definite/probable stent thrombosis on univariable analyses (hazard ratio: 0.61; 95% confidence interval: 0.33 to 1.12; p = 0.10), any baseline angiographically visible thrombus (hazard ratio: 4.86; 95% confidence interval: 4.86; 1.73 to 13.65; p = 0.003) and trifurcation lesion (hazard ratio: 2.27; 95% confidence interval: 1.01 to 5.12; p = 0.048) were the strongest independent predictors. Sixty-six of 903 subjects (7.3%) in the PCI cohort were reported to have trifurcation lesions, of which 12 of these 66 subjects had ARC ST (ARC definite ST: n = 5; ARC probable ST: n = 5; ARC possible ST: n = 2). Three of the 12 cases of ARC ST occurred in <30 days (2 in subjects with ULMCA disease), and 7 occurred in >30 days (6 in subjects with ULMCA disease). [285285. Farooq V, Serruys PW, Zhang Y, Mack M, Ståhle E, Holmes DR, Feldman T, Morice MC, Colombo A, Bourantas CV, de Vries T, Morel MA, Dawkins KD, Kappetein AP, Mohr FW. Short-term and long-term clinical impact of stent thrombosis and graft occlusion in the SYNTAX trial at 5 years: Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery trial. J Am Coll Cardiol. 2013;62:2360-9 ].
Distal LMS (Bifurcation Disease)
- When undertaking ULM PCI, although carina shift is the predominant mechanism of SideB closure, given the larger volume of plaque in a diseased LMS, plaque shift and incomplete stent expansion are important technical issues that should be considered
- Aorto-ostial and mid-vessel lesions comprise 30% of ULM PCI and should be treated with a single-stent strategy
- Distal bifurcation lesions comprise two thirds of ULM disease and are associated with more adverse clinical outcomes compared to ostial or shaft LMS disease
- Whenever possible, a one-stent strategy to ULM bifurcation PCI should be adopted, as it is associated with fewer adverse clinical outcomes compared to a 2-stent approach
- KBPD after a one-stent approach may not be unreasonable. Long term data using this is awaited
- KBPD after a 2-stent approach is mandatory to correct any stent distortion and minimise immediate ostial SideB stenosis
- The choice of a 2-stent approach to the left main bifurcation is dependent on the anatomy and whether an upfront provisional approach (majority of cases) or a 2-stent approach is required. Treatment algorithms as described can guide the operator (as previously illustrated ( Figure 52 and Figure 53 ). The double kissing crush technique has been reported to be associated with improved clinical outcomes when compared to Culotte stenting and provisional stenting in a randomised clinical trials.
- Trifurcation disease occurs in 20% of distal LMS PCI lesions. A “simple is better” approach should be adopted with the aim of ensuring patency of all branches and minimising the risk of late/very late stent thrombosis.
Personal perspective – Patrick W. Serruys
With the release of the primary results of the 3-year follow-up of the EXCEL trial, the non-inferiority of PCI in comparison with CABG was established for site-reported low (<22) and intermediate (22 – 33) SYNTAX scores (although core laboratory analysis identified 27% of patients in the highest SYNTAX tertile – above 33). The concern for the near future will be the results of long-term follow-up. The EXCEL 5-year results are expected in the end of 2019. Another awaited results to complement EXCEL 5-years and to go further in the follow-up period is the Extended SYNTAX (SYNTAXES), where patients are followed for 10 years after the procedure they were randomised (either PCI or CABG).
The topics that will most likely progress are:
Decision making tools: The SYNTAX score is consolidated as a decision making tool, and its variations for prognostic impact (SYNTAX score II) and functional non-invasive assessment of stenosis (SYNTAX score III). In a mid-term period we should also expect artificial intelligence as an adjunctive tool to SYNTAX scores calculation.
Devices: Bifurcation dedicated devices for left main are coming back. Results of the ongoing POLBOS – left main study are awaited. This study is testing the Bioss LIM C. This device has the philosophy of the established provisional stenting and a “POT-like” technique. The study will assess a pre-specified performance goal based on the results of EXCEL.
Pharmacotherapy: Inhibitors of PCSK9 may be a great hope for patients with non-obstructive coronary artery disease, and therefore extrapolated and applied as secondary prevention especially when patients have three-vessel or left main stem disease.