Summary
The treatment options for patients with vascular and structural heart disease have been growing over recent years with a strong trend towards less invasive treatment modalities.
In this chapter we will describe the evolution of cardiac catheter laboratories and take a look into the future with a strong focus on imaging techniques as they are used today as well as in the near future.
Cardiac catheter laboratories have adapted to the general progress seen in medicine during the 20th century. They are diagnostic and treatment spaces that are primarily devoted to cardiac diseases in particular coronary disease. One of their key functions is therefore coronary imaging, including invasive techniques to assess and determine the structure of the coronary vessel wall allowing for a more complete diagnosis. Advances in technology reflect the demands of the interventional operators themselves who desire as optimal an image as possible while performing the most minimal invasive procedure.
The chapter follows the evolution of the catheter laboratory from its beginnings through to the contemporary state-of-the-art functionalities and finally a glimpse into the future.
An effort is made to look through the eyes of different users involved in treating cardiovascular patients. Patient safety and effectiveness are the starting points of every treatment, so we will describe developments targeted to fulfil that desire.
Introduction
The adult cardiac catheterisation laboratory has evolved from a facility to understand cardiac and coronary cardiovascular physiology, using right and left heart catheterisation techniques, to one of routine elective and non-elective diagnosis and treatment across a broad spectrum of coronary, peripheral and cardiac structural disease. The catheter laboratory environment has reflected the demands of interventional practitioners and increasingly those of patients.
The past
HISTORICAL PERSPECTIVE
The catheterisation laboratory (‘cath lab’) emerged in the 1950’s as an experimental facility to study congenital and valvular heart disease. Following the development of selective coronary angiography and surgical coronary revascularisation techniques this evolved into a formal diagnostic discipline in need of a designated area. These early cath labs were located within existing radiology department imaging rooms ( Figure 1 ) and hence procedures were frequently performed after ‘office hours’.in order not to impact on the radiology worklist. It was not, however, until the seminal work of Andreas Gruntzig with balloon angioplasty in the 1970’s and 1980’s. and the simultaneous use of antithrombotic and fibrinolytic therapies for acute myocardial infarction that a rapid expansion of dedicated cardiac catheter laboratories took place.
This expansion ushered in the next era of the cardiac catheterisation laboratory, namely as a diagnostic and therapeutic environment. In particular the laboratory became involved with non-elective patients with acute coronary syndromes thus requiring them to be 24/7 facilities. Although initially restricted to academic university hospital centres, with growing technical expertise, equipment improvements and patient selection protocols there was an expansion of facilities to non-academic centres. This second era, which was primarily concerned with coronary work has now entered a third age with the advent of percutaneous therapies relevant to structural and peripheral cardiovascular disease.
The present
CONVENTIONAL CATHETER LABORATORIES
Contemporary catheter laboratories exist in four external environments that are dependent on the surgical and critical care support available:
1. The catheter laboratory with on-site cardiothoracic surgical support
2. The catheter laboratory without cardiothoracic support
3. The mobile or free-standing catheter laboratory
4. The hybrid laboratory
No matter the external environment a cath lab consists of a certain number of essential elements [11. Bashore TM. (chair) Task Force, American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on Cardiac Catheterization Laboratory Standards. J Amer Coll Cardiol. 2001;37(8). ].
Diagnostic functions of a cardiac catheter laboratory
- Right heart catheterisation and angiography
- Right and left heart catheterisation and angiography
- Left heart catheterisation and angiography
- Coronary angiography
- Myocardial biopsy
- Pericardiocentesis
Procedure room
The AHA recommends a minimum of 500-600 square feet for the main procedure room and an additional 100-200 square feet for the control room. Further space requirements relate to the imaging equipment [22. Klein LW, Miller DL, Goldstein J, Haines D, Balter S, Fairobent L, Norbash A; On behalf of the members of the Multispecialty Occupational Health Group. The catheterization laboratory and interventional vascular suite of the future: Anticipating innovations in design and function. Catheter Cardiovasc Interv. Jan 1 ]. A lead protected viewing area is also mandatory.
Within or adjacent to the lab there must be storage space for drugs and equipment ( Figure 2 ).
Access to the lab must be wide in order to allow critical care transfers with anaesthetic equipment and preferably automatic doors at two entrances to the lab.
Ancillary rooms/waiting areas and a patient recovery zone although not mandatory are advisable to enhance patient flow. Lead protection apparel must be housed upright in an orderly fashion to prevent damage that may reduce its protective function ( Figure 3 ).
A scrub room or area for the operating staff is ideally situated in a separate room adjacent to the main cath lab, although in many less recent designs it is incorporated within the lab itself.
A sluice for disposal of waste must be adjacent to the lab.
Hardware
Essential requirements include X-ray equipment, haemodynamic and radiographic monitor displays, radiation shielding, a movable operating table, reinforced floors, a control room (which must be adjacent to the lab or within the lab itself) to allow full view of the percutaneous procedure.
Contemporary X-ray imaging equipment includes digital flat panel technology [33. [Epub ahead of print] No abstract available.
3. High Performance Digital Flat-Panel Detectors Revolutionize X-Ray Imaging in Cardiology. X-Ray Technology Update, GE Medical Systems, February 2000. Digital Imaging and Communications in Medicine (DICOM), National Electrical Manufacturers Association, 2001.]. This has many advantages over the original image intensifier technology used in early cath lab designs ( Figure 4 ). These include:
1. uniformity of brightness across the entire image
2. absence of glare
3. absence of geometric distortion
4. improved dynamic range
Biplane x-ray equipment is also used in contemporary designs. This was the original form of x-ray contruction but was supplanted by monoplane technology in the 1990’s. The advantages of biplane technology include:
1. Improved procedural execution of structural cases
2. Reduced radiation and contrast load
3. Improved acquisition of anomalous coronary arteries [44. Wang A, Pulsipher MW, Jaggers J, Peterson GE, O’Laughlin MP, Bashore TM, Harrison JK. Simultaneous biplane coronary and pulmonary arteriography: A novel technique for defining the course of an anomalous left main coronary artery originating from the right sinus of Valsalva. Cathet Cardiovasc Diagn. 1997 Sep;42(1):73-78. ]
4. Reduction in panning artefact
5. Improved ventriculograhy
Lighting must include overhead, soft perimeter lighting and surgical spotlight capability. Some contemporary designs use coloured lighting (ambilight). This is described later in the chapter.
Emergency equipment should include an anaesthetic machine and resuscitation cart with external defibrillator ( Figure 5 ). IABP and transthoracic echo equipment should be adjacent to the lab. ( Figure 6 ).
Adjunctive invasive diagnostic equipment is increasingly being integrated into the primary display monitors of state-of-the art cath labs, nevertheless standalone IVUS, FFR, and OCT in many cases still exist. These should remain in the lab and be easily attached to the primary monitoring systems.
Information technology
This consists of primary software for haemodynamics, electrocardiographic monitoring as well as software for image archiving and review and clinical report generation. Integration of data into primary line-of-sight displays for the operator is fast coming standard design in new cath lab constructions. ( Figure 7 [panels A, and B]). Digital picture archiving with easy retrieval is the goal of any cath lab informatics system. Traditionally the dynamic cardiovascular and interventional images were difficult to integrate into the main hospital archiving system owing to limits on size and bandwidth. Nowadays enhanced storage capacity means that in most units this integration is possible so that images can be easily viewed and retrieved form any location in the hospital ( Figure 8 ).
Occupational health considerations
Occupational hazards that impact on the health of catheter laboratory staff include:
1. Ionising radiation
2. Orthopaedic disease
3. Biological (non-radiation) hazards
4. Chemical hazards
5. Psychological hazards
These hazards are important as they should shape and inform the design of the catheter laboratory environment. Unfortunately due to under-reporting a lack of data these have had hitherto minimal input into catheter laboratory design [55. Goldstein JA, Balter S, Cowley M, Hodgson J, Klein LW. Occupational hazards of interventional cardiologists: prevalence of orthopedic health problems in contemporary practice. Cathet Cardiovasc Interv. 2004;63:407-411. , 66. Dehmer GJ. Occupational hazards for interventional cardiologists. Cathet Cardiovasc Interv. 2006;68:974-976. ].
Long term work in the catheter laboratory environment exposes practitioners to the risks of ionising radiation and orthopaedic injury. The former is dealt with in detail in  View chapter. It is apposite to mention, however, that there are increasing concerns surrounding the biological effects of long-term exposure to low levels of ionising radiation [77. Serruys PW. How to remain focussed in a globaised world. Eurointervention. 2012; 9:1009-1010. , 88. Roguin Ariel, Goldstein Jacob, Bar Olivier. Brain tumours among interventional cardiologists: a cause for alarm? Report of four new cases from two cities and a review of the literature. EuroIntervention. 2012;7:1081-1086. ].
View chapter. It is apposite to mention, however, that there are increasing concerns surrounding the biological effects of long-term exposure to low levels of ionising radiation [77. Serruys PW. How to remain focussed in a globaised world. Eurointervention. 2012; 9:1009-1010. , 88. Roguin Ariel, Goldstein Jacob, Bar Olivier. Brain tumours among interventional cardiologists: a cause for alarm? Report of four new cases from two cities and a review of the literature. EuroIntervention. 2012;7:1081-1086. ].
A sentinel reporting system for adverse effects in particular cataract and neoplasia is being proposed in order to better understand the scale of the hazard.
With regard to orthopaedic injury, although once again there is limited scientific data, surveys reveal a high reported incidence of (weight-bearing) spinal, hip and knee complaints [55. Goldstein JA, Balter S, Cowley M, Hodgson J, Klein LW. Occupational hazards of interventional cardiologists: prevalence of orthopedic health problems in contemporary practice. Cathet Cardiovasc Interv. 2004;63:407-411. ]. This is intuitively a result of the heavy lead-based radiation protection apparel, however, poor lighting and awkward line-of-sight views of the monitor displays also contribute significantly to poor ergonomic design. Among long-serving interventionists orthopaedic injuries are frequently responsible for absence of work and in some cases can curtail careers.
As in other clinical areas biological (predominantly infectious) hazards are ever present and so a universal precautionary approach is required with all bodily fluids considered to be potentially hazardous. Sharps management includes adequate provision of secure disposal bins in addition to strict clinical process protocols.
Chemical exposure to anaesthetic gases should not occur with modern scavenging systems installed within contemporary cath labs. Hand-scrub liquids and repeated gloving-up for multiple procedures can induce allergic or contact irritant dermatitis. A range of standard and hypoallergenic gloves should be available.
Owing to the acute coronary syndrome workload and risk of serious complications during catheter laboratory practice. Cath lab staff are exposed to psychological distress, and shift pattern work. These effects may translate into sub-optimal performance.
Inventory control
The cardiac catheterisation laboratory has been the location for the interventional treatment of coronary disease since the 1970’s. The changing face of cardiovascular disease management, however, has placed demands that have led to the development of treatments for structural and peripheral disease
Percutaneous cardiovascular technologies have thus proliferated in an almost exponential fashion. A catheter laboratory needs to be stocked with sufficient materials in order to deliver such a clinical service. Stock/inventory management is therefore an integral part of catheter laboratory workflow. An average inventory may include between 300-350 items.
There are several models of inventory control. cath lab units tend to use one or a combination of models.
These include:
a. a consignment model: where stock is placed by the manufacturer but that a charge is only made on items that have been used. The manufacturer may move equipment in order to maximise their product visibility.
b. a Just-in-time model, where items are only ordered for specific procedures..This has the advantage of only allowing the unit to buy products as and when they are needed. Its disadvantage is that external factors such as delayed delivery can impact significantly on the ability to provide a service.
c. a Bulk model, where estimates on future use based on current and past inventories is used to obtain stock en masse. This has the advantage of secure procurement, however, as many items are used infrequently it can be prohibitively expensive.
In addition to the method of procurement , monitoring the usage of materials is vital for efficient inventory management. Here traditionally manual counting of stock has been the foremost method employed but is time-consuming and due to its repetitive nature is prone to error ( Figure 2 and Figure 9). More modern methods rely on barcode control of stock that can allow for efficient automation of this important process.
HYBRID LABORATORIES
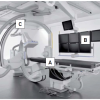
The advent of percutaneous therapies for aortic stenosis combined with the promotion of the multidisciplinary Heart team (see Chapter Head) following the Syntax study has heralded in a sea change in interventional practice. Transaortic valvular implantation can be performed via one of several access routes and this necessitates the presence of a team with surgical expertise. The location of this quasi-surgical procedure requires both the attributes of an operating room and that of an interventional catheterisation laboratory ( Figure 10 ).
The operating room specifications of importance are:
- Positive airflow to enhance sterility
- Optimised lighting
- Equipment for heart-lung bypass
The catheterisation laboratory specifications of importance are:
- Advanced imaging technology
- Movable operating table
- Advanced information technology systems
By combining these attributes the concept of the hybrid laboratory has emerged. The hybrid laboratory thus ideally consists of several components:
The requirements are for a large room with all the anaesthetic requirements of an operating room as well as close to the definitive operating theatre complex, and critical care facility
Able to produce multiple field of views, ceiling mounted, with rotational as well as digital subtraction angiographic capability.
- Adjunctive multi-modality imaging
Live acquisition
In order to view the immediate results of on-table adjunctive imaging, these should be integrated into the main monitor display. Intraccardiac echo, transoesophageal echo all need to be included in the feeds into the slave monitors.
Previously acquired imaging
Increasingly pre-procedural imaging with CT and MR is being used to help execute an intervention. Ideally the hybrid lab should be able to co-register the previously acquired images with a fluoroscopic overlay ( Figure 11 ). This process involves segmentation where specific anatomical features are emphasised and extraneous parts of the dataset are disregarded. This form of technology is particularly useful for complex structural interventions when manoeuvres using 2D imaging alone can be challenging and can add unnecessarily to the overall dose of ionising radiation.
MOBILE CATHETER LABORATORIES
These angiographic facilities are used where fixed cath labs are not available because of contamination e.g., MRSA or where fixed facilities are too distant or underused by the local population. This may be seen where there are communities suffering socio-economic deprivation [99. Sketch MH Jr, Pieper KS, Warner J, Daniel JM, Wilkerson TM, Harrison JK, Peterson ED, Bashore TM. Mobile cardiac catheterization laboratories increase use of cardiac care in women and African Americans.Am Heart J. 2007 Sep;154(3):532-8. ].
THE HEALING ENVIRONMENT
The evolution of technology and medical care is now more focussed on not just the technical outcome of the procedure but also the patient experience and journey. This is most evident in paediatric care but is also true of adult patients. Manufacturers in cath lab design have begun to develop the concept of the healing environment where lighting and space are used to try and promote a more pleasant patient experience of a procedure.
Ambilight ( Figure 12 )
The ambilight is an example of one such approach and includes changeable background lighting as well as audiovisual tools such as ceiling mounted video displays.
The future
To look into the future of vascular imaging and intervention and the way it will be performed can be done in different ways: either by formulating the optimal situation as one would wish to see or dream it, or by building on today’s developments in technology.
In both scenarios the starting point is the best diagnosis and treatment options for the patient, with there being no harm or risk from radiation or contrast. However, the recent past has taught us that predicting the future is almost impossible. Developments in vascular diagnosis and treatment have changed faster then anyone could have predicted 25 years ago, with a strong trend towards minimalisation of the invasiveness of the procedure.
It therefore seems wise to limit one’s look into the future to the next 3 to 5 years.
Before speculating on the technical developments that have to come from the clinicians’ desires and must be developed together with the industries’ engineers and that will be influenced by external factors such as resources and medical progress in general, it seems wise to try to formulate the ideal situation. Therefore, start with the dream of an optimal situation in the future and then see what is already available or under development.
The ultimate dream today is optimal imaging and functional information enabling precise diagnosis and treatment of the cardiovascular patient without any risk or harm. For example, the dream could be 3D imaging with functional information up to cellular level without the use of potentially harmful radiation or contrast media.
To outline further this laboratory for the future an input from many stakeholders is necessary. Not only different users such as interventional cardiologists, electrophysiologists, vascular surgeons and radiologists, but in particular engineers and computer experts (IT) should be involved in future designs.
Requirements for a hybrid (valvular) catheter laboratoryRoom
- Large size, ventilation/gases/suction, proximity to OR/ICU
- Ability to adjust range for soft tissue imaging
- Ceiling mountedequipment
- Rotational angiography capability
- Digital subtraction angiographic capability
X-ray system
Adjuctive imaging to aid:
- Pre-procedure planning
- Procedure execution
- CT guided procedures
- Registration with CT
Up to 6 display monitors
- Imaging workstation and in-room monitors
- Navigations systems and robotics
- Supplies
- Toolbox for complications
- Haemodynamic monitoring
- Heart-lung bypass / anaesthetic equipment
TRENDS
When we look at today’s trends in treatment modalities and take that as a starting point to describe the future laboratories, we notice that in vascular medicine there is the need for better understanding of the pathophysiology of the vessel and the vascular reaction on intervention. Therefore, what we want is to be able to predict which patient needs which procedure and how he/she will react to, and profit from this procedure. Some of the answers will come from other sources but much information will be gathered during a procedure with different imaging and measuring methods. These data will inform us during a procedure in real-time about the underlying pathophysiology of a disease, how to treat it and in the case of intervention the final outcome. For instance, in the patient with an acute coronary syndrome, one can be informed about the plaque by using plaque analysing systems such as Volcano intravascular ultrasound (IVUS) (Volcano Corporation, San Diego, CA, USA), and we can use fractional flow reserve (FFR) to check the appropriateness of the procedure whereas IVUS and optical coherence tomography (OCT) can be used for sizing and control of the procedure. To help us to a better understanding and planning of procedures, 3D imaging is the approach nearest to the anatomy we want to investigate and treat. In fact, today the first steps are being made towards 3D reconstruction of the vascular tree with 3D motion compensation algorithms which also enable us to interpret stent geometry after implantation ( Figure 13 ). All this should be incorporated in the laboratory in a construction such that everything is built into one console and can be seen simultaneously on one screen.
We also foresee a strong increase in the minimal invasive treatment of valvular disease and other non-vascular cardiac disorders necessitating perfect 3D imaging including 3D echocardiography and overlay imaging technology to guide procedures.
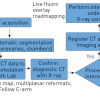
Similar developments are seen in electrophysiology where procedures are getting more and more complex and need perfect guiding with complex road mapping systems. Intricate electromagnetic mapping systems are used to guide more complex ablation procedures, such as for atrial fibrillation or ventricular tachycardias. The 3D reconstructions of the heart that are integrated in these mapping systems are usually required by CT-scanning prior to the procedure ( Figure 14 ).
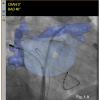
Recently, intraprocedural atriography by rotating the C-arch has proven to be a more cost-effective and accurate source for these 3D reconstructions. [1010. Knecht S, Wright M, Akrivakis S, et al: Prospective randomized comparison between the conventional electroanatomical system and three-dimensional rotational angiography during catheter ablation for atrial fibrillation. Heart Rhythm. 2010; 7:459-465. ] The desire for simple and effective procedures has led to using only these 3D volumes in combination with electrophysiological catheters for the fast yet efficient treatment of patients with paroxysmal AF. ( Figure 15 ). shows a routine set-up used in several EP laboratories in which a preprocedural CT-scan is overlaid on real-time fluoroscopy to permit fast and cost-effective treatment for paroxysmal atrial fibrillation without the use of intricate electro-anatomic mapping systems. In the EP lab 3D reconstructions of the left atrium superimposed on the real-time fluoroscopy (such as EP navigator) have been used for several years for the treatment of patients with paroxysmal atrial fibrillation [1111. Stevenhagen YJ, van der Voort PH, Dekker LRC, et al.: 3D CT Overlay in comparison to CARTO Merge for Pulmonary Vein Antrum Isolation. J Cardiovasc Electrofysiol. 2010; 21:634-639. ] It is our expectation that 3D reconstructions will be introduced for device implantations will also be introduced in the coming years and that using 3D reconstructions of the cardiac venous system in combination with electromagnetic navigation will guide epicardial LV-led implantations with minimal or even no fluoroscopy. Integration of all these sources of information will constitute a major challenge for engineers and computer experts. Likewise, optimal integration of various imaging modalities such as 3D reconstructions of infarcted ventricles or coronary arteries into mapping systems for the analysis of electrical conduction will greatly support the efficacy and safety of endocardial or epicardial ablations of ventricular tachyarrhythmias.
New professionals have entered the traditional cathlab arena in recent years. Hybrid rooms combining full operation room and cathlab facilities enable us to perform more and more complex procedures. Vascular and cardiac surgeons work together with interventionalists for percutaneous or transapical aortic valve implantations and mitral valve repair. There is no doubt that 3D imaging will facilitate such complex procedures. Likewise, the epicardial approach for pulmonary vein isolations by the cardiac surgeon in cooperation with the electrophysiologist, which places additional endocardial lesions after assessing the degree of block, requires a new kind of cathlab [1111. Stevenhagen YJ, van der Voort PH, Dekker LRC, et al.: 3D CT Overlay in comparison to CARTO Merge for Pulmonary Vein Antrum Isolation. J Cardiovasc Electrofysiol. 2010; 21:634-639. ]. One of the modalities that allows 3D imaging is CT scanning. A wider application can be foreseen such as pre-procedural planning particularly for structural intervention,, but in many situations it seems logical to have that kind of information directly available in the laboratory. The same principle more or less applies to MRI.
Vascular and cardiac surgeons have moved from a situation where they had the anatomy directly visualised and literally in their hands to an environment where they have to rely on technical imaging techniques. These techniques need specific interpretation and may even provide better information than previously. Surgeons may now perform procedures in a remote and minimally invasive way. They will have specific demands and might need specific imaging modalities on-line, such as CT or MRI.
Future perspectives
- Minimal invasiveness is the future
- Patient safety and efficiency will be the leading factors
- A more general specialist treating the cardiovascular patient will emerge who has to have a profound knowledge of future imaging
WHAT CAN WE EXPECT?
Today, digital imaging is the basis in our work, but the strong need to decrease radiation and contrast use might change this leading us to use more frequently, if possible echo and MRI during procedures.
In today’s modern combined catheterisation laboratories, the so-called hybrid rooms where cardiologists, vascular surgeons, cardiac surgeons and radiologists come together, the use of flat-panel detectors is routine and a further development of 3D angiography, road mapping systems and integrated imaging modalities will further enhance the therapeutic options. Tissue determination during the procedure will tailor the therapy. An important future development that will help us in increasing success rates of ablations in the electrophysiology lab is the possibility to see in a real-time fashion lesion development and size. Real-time appreciation of transmurality and degree of overlap of individual ablation points will be of great value in the EP cathlab.
INTEGRATION
As we view today’s trends, there will be an increase in combining and integrating different modalities, where up until today information has been mostly gathered before a procedure starts and then a procedure is performed typically using fluoroscopy and angiography, we already observe an increase in combining modalities during the procedure.
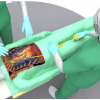
In percutaneous valve implants, information gained before a procedure, for instance CT scanning of the aortic route for sizing and optimal projection directions, can be used during the procedure as an overlay to guide the procedure in combination with 3D echocardiography before and during the same procedure. By using the combination of these modalities, the use of contrast and x-ray is already decreased significantly. This is only one example of the combining of modalities. In electrophysiology we also see a strong trend towards the use of a combination of imaging modalities and robotics [1212. Robotic approach to catheter ablation. Ernst S. Current Opinion in Cardiology. 2008, 23:28–31. ].
SAFETY ERGONOMICS
As described above, future laboratories will host different specialists and more complex patients undergoing extensive procedures. This will demand a new design of the laboratories. Hybrid rooms that are already seen in a number of hospitals require a different air treatment and a different way of working in relation to sterility. Multiple air turnovers more than 5 or 10 times are not only mandatory in the case of anaesthesia but also for durable implants. In addition, more space is needed in case of on the spot change to surgery. Therefore, machinery in the room producing heat and needing space is another complicating factor.
For the professionals working in the laboratories, longer procedures further stress the need for an alternative to the conventional lead protection. The use of ultrasound and MRI will increase, but x-ray is still the most frequently used modality. Spine issues, related to the wearing of shielding, are known to every professional in today’s laboratories. Therefore, alternatives such as lead shielding carried by frames or mounted on the ceiling (so-called zero gravity) or remote control (robot-like) of the tools are needed to solve this problem. Awareness systems for x-ray exposure will further reduce the use of fluoroscopy or angiography which are not absolutely necessary.
The use of contrast media in an ageing population with a higher frequency of renal function impairment drives the need for less usage of contrast. ( Figure 16A and Figure 16B ).
INFORMATION TECHNOLOGY
Today, but even more so in the future, there is the absolute necessity to document our procedures. This is mandatory not only to register the outcome but also to be able to calculate the costs of the materials used and to order new materials. Society demands maximal transparency in costs, indications, outcomes and safety. These data should be readily available, reproducible and comparable, and trends must be watched. This requires solid software and hardware and capable data managers.
Remote data interpretation and monitoring of procedures requires optimal connectivity to allow supervision or counselling during the procedures.
Future technological innovations
- Tissue characterisation will be performed in the near future allowing focused treatment
- We are on the threshold of 3D imaging without the use of x-ray and contrast
- Remote or robot surgery seems useful
Dreams
Systems to operate catheters remotely for interventions or ablations, such as Stereotaxis, represented our dreams 10 years ago..If resources had been unlimited these dreams would have reached a higher degree of reality. These innovations, however, remain and their use in the catheter lab may be realisable in the future.
Personal perspective - Jacques J. Koolen
With financial constraints, not every dream of the engineer and the doctor will come true, but, as we can see already today, patient safety and, related to that, the need for optimal guidance of procedures are major issues.
What I expect in the near future is a further development in the direction of 3D imaging, with a parallel development in tissue characterisation. At first, 3D imaging will be performed by a combination of CT and echo, but over time non x-ray non-contrast systems will predominantly be used. Whether remote control systems will find a broad application is in part dependent on the use of non-x-ray systems and in part on their preciseness and their ease of use.
As already stated, looking into the future is not easy but, with a lot of technical developments on the horizon, patient diagnosis and treatment will be perfected further.