Summary
PVS is a progressive illness and unless good surgical relief can be obtained early in the course of the disease the course becomes recalcitrant to further therapeutic intervention with long-term results being generally disappointing. Published series do, however, clearly document short-term improvements from catheter approaches, not only in terms of vessel diameter, pullback gradients and right ventricular pressure or pulmonary artery resistance, but also in patient symptoms. There is clearly much room for improvement in the management of this condition though the rarity of the lesion precludes significant advances from being made. Animal models hold some promise [8282. Mutsuga M, Narita Y, Yamawaki A, Satake M, Kaneko H, Usui A, Ueda Y. Development of novel drug-eluting biodegradable nano-fiber for prevention of postoperative pulmonary venous obstruction. Interact Cardiovasc Thorac Surg. 2009;8:402-6; discussion 6-7. , 8383. Furukawa T, Kishiro M, Fukunaga H, Ohtsuki M, Takahashi K, Akimoto K, Shimizu T, Kawasaki S, Kumasaka T. Drug-eluting stents ameliorate pulmonary vein stenotic changes in pigs in vivo. Pediatr Cardiol. 2010;31:773-9. ]. A reasoned interventional approach following exploration of surgical options and a joint institution decision would begin with a careful diagnostic catheter study followed by targeted angioplasty. In the presence of a fixed lesion, despite high inflation pressures of a non-compliant angioplasty balloon, a cutting balloon might be considered. Where there is significant recoil of a lesion and the clinical circumstances demand a good result, a stent may be placed. Interventional procedures must regrettably be regarded as palliative, with the disease being associated with an all too frequently grave overall prognosis.
Introduction
Stenosis of the pulmonary veins is a rare but serious condition and can involve single or multiple veins. The outlook is guarded and treatment options limited. Following therapy, realised clinical improvement can be disappointingly short-lived. It is against this backdrop that many catheter and surgical therapies have emerged. Results not infrequently leave the reader wondering whether the natural history has been modified at all; in most cases the progression of disease is relentless. Here we review the disease pathogenesis and the catheter-based treatment options available. Interventional techniques including angioplasty, cutting balloon angioplasty and stent placement are discussed in detail. What is known regarding risk factors for an adverse outcome is considered, along with the appropriate timing for intervention.
Definitions
Pulmonary vein stenosis (PVS) can be defined as primary or secondary depending on whether it occurs in the absence or presence of prior atrial surgery or intervention. In a paediatric population primary PVS occurs most commonly following prematurity and secondary PVS most commonly following repair of total anomalous pulmonary venous drainage (TAPVD). In an adult population, secondary PVS can follow radio-frequency ablation procedures for atrial fibrillation or atrial futter. Primary PVS can occur in isolation but is often associated with a range of other cardiac diagnoses [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence., 44. Devaney EJ, Chang AC, Ohye RG, Bove EL. Management of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 2006;81:992-5; discussion 995-6.
This reference begins to discuss the treatment options available in the context of a series of 36 cases.]. Age of presentation varies but for primary PVS it is usually in infancy, with failure to thrive, respiratory infections, dyspnoea and respiratory failure being the most frequent initial complaints [22. Drossner DM, Kim DW, Maher KO, Mahle WT. Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics. 2008;122:e656-61.
The association of pulmonary vein stenosis and prematurity is a relatively recent observation and is introduced in this reference., 44. Devaney EJ, Chang AC, Ohye RG, Bove EL. Management of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 2006;81:992-5; discussion 995-6.
This reference begins to discuss the treatment options available in the context of a series of 36 cases., 55. Seale AN, Daubeney PE, Magee AG, Rigby ML. Pulmonary vein stenosis: initial experience with cutting balloon angioplasty. Heart. 2006;92:815-20. ]. In premature infants it can be compounded by the coexistence of chronic lung disease. There is a weak association between the number of veins involved and the degree of their obstruction with the severity of symptoms [88. Breinholt JP, Hawkins JA, Minich LA, Tani LY, Orsmond GS, Ritter S, Shaddy RE. Pulmonary vein stenosis with normal connection: associated cardiac abnormalities and variable outcome. Ann Thorac Surg. 1999;68:164-8. ]. Stenosis of a single vein can, however, drive pulmonary hypertension. Pulmonary hypertension becomes increasingly severe with time and right ventricular failure evolves. If there is an associated atrial septal defect in this setting profound cyanosis can result. Periodic haemoptysis is not infrequent from the affected lobe or the collateralisation that can resut.
Pulmonary vein stenosis
- PVS is a rare condition and not infrequently associated with other cardiac malformations and prematurity [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence., 22. Drossner DM, Kim DW, Maher KO, Mahle WT. Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics. 2008;122:e656-61.
The association of pulmonary vein stenosis and prematurity is a relatively recent observation and is introduced in this reference.]
- PVS is a progressive illness and unless good surgical relief can be obtained early in the course of the disease the course becomes recalcitrant to further therapeutic intervention with long-term results being generally disappointing [33. Holt DB, Moller JH, Larson S, Johnson MC. Primary pulmonary vein stenosis. Am J Cardiol. 2007;99:568-72.
This reference searches the Pediatric Cardiac Care Consortium Database to identify 31 cases from which to attempt to clarify prognostic predictive factors for adverse outcomes.]
- In this context interventional procedures must be regarded as palliative, with a primary objective of symptomatic improvement [44. Devaney EJ, Chang AC, Ohye RG, Bove EL. Management of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 2006;81:992-5; discussion 995-6.
This reference begins to discuss the treatment options available in the context of a series of 36 cases.]
Prevalence
PVS was first described in 1951 [99. Reye RD. Congenital stenosis of the pulmonary veins in their extrapulmonary course. Med J Aust. 1951;1:801-2. ] emphasising the rarity of the lesion and the difficulties with making a diagnosis. By comparison with other uncommon left heart inflow obstructive lesions (cor triatriatum, supramitral membrane and mitral stenosis), PVS is much rarer [1010. Lucas RV Jr, Anderson RC, Amplatz K, Adams P Jr, Edwards JE. Congenital Causes of Pulmonary Venous Obstruction. Pediatr Clin North Am. 1963;10:781-836. , 1111. Nakib A, Moller JH, Kanjuh VI, Edwards JE. Anomalies of the pulmonary veins. Am J Cardiol. 1967;20:77-90. , 1212. Shone JD, Amplatz K, Anderson RC, Adams P Jr, Edwards JE. Congenital stenosis of individual pulmonary veins. Circulation 1962;26:574-81. , 1313. Park SC, Neches WH, Lenox CC, Zuberbuhler JR, Siewers RD, Bahnson HT. Diagnosis and surgical treatment of bilateral pulmonary vein stenosis. J Thorac Cardiovasc Surg. 1974;67:755-61. , 1414. Mortensson W, Lundstrom NR. Congenital obstruction of the pulmonary veins at their atrial junctions. Review of the literature and a case report. Am Heart J. 1974;87:359-62. , 1515. Bini RM, Cleveland DC, Ceballos R, Bargeron LM Jr, Pacifico AD, Kirklin JW. Congenital pulmonary vein stenosis. Am J Cardiol. 1984;54:369-75. , 1616. van Son JA, Danielson GK, Puga FJ, Edwards WD, Driscoll DJ. Repair of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 1995;60:144-50. ]. Searching the Pediatric Cardiac Care Consortium database over a twenty-year period, Holt reports an incidence of primary PVS of 0.03% [33. Holt DB, Moller JH, Larson S, Johnson MC. Primary pulmonary vein stenosis. Am J Cardiol. 2007;99:568-72.
This reference searches the Pediatric Cardiac Care Consortium Database to identify 31 cases from which to attempt to clarify prognostic predictive factors for adverse outcomes.]. No gender discrepancy has been described. Familial cases have rarely been reported [1717. Edwards JE. Congenital stenosis of pulmonary veins. Pathologic and developmental considerations. Lab Invest. 1960;9:46-66. , 1818. van de Laar I, Wessels M, Frohn-Mulder I, Dalinghaus M, de Graaf B, van Tienhoven M, van der Moer P, Husen-Ebbinge M, Lequin M, Dooijes D, de Krijger R, Oostra BA, Bertoli-Avella AM. First locus for primary pulmonary vein stenosis maps to chromosome 2q. Eur Heart J. 2009;30:2485-92. ].
There is no clear pattern of associated malformations occurring with PVS evident from the literature. Of 58 cases of PVS retrospectively reviewed across three European countries, isolated PVS occurred in only 10% with the remainder being associated with various cardiac anomalies (ventricular septal defect, atrioventricular septal defect, cor triatriatum, supravalvar mitral membrane, scimitar syndrome, coarctation and Ebstein’s malformation amongst others) [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence.]. Similar findings have been reported in other series [88. Breinholt JP, Hawkins JA, Minich LA, Tani LY, Orsmond GS, Ritter S, Shaddy RE. Pulmonary vein stenosis with normal connection: associated cardiac abnormalities and variable outcome. Ann Thorac Surg. 1999;68:164-8. , 1919. Fong LV, Anderson RH, Park SC, Zuberbuhler JR. Morphologic features of stenosis of the pulmonary veins. Am J Cardiol. 1988;62:1136-8. , 2020. Driscoll DJ, Hesslein PS, Mullins CE. Congenital stenosis of individual pulmonary veins: clinical spectrum and unsuccessful treatment by transvenous balloon dilation. Am J Cardiol. 1982;49:1767-72. , 2121. Ito M, Kikuchi S, Hachiro Y, Abe T. Congenital pulmonary vein stenosis associated with cor triatriatum. Ann Thorac Surg. 2001;71:722-3. , 2222. Pappas G. Left pulmonary vein stenosis associated with transposition of the great arteries. Ann Thorac Surg. 1986;41:208-9. ]. More recently we have become increasingly aware of PVS as a long-term sequela in extremely preterm babies. Of the 26 cases reviewed by Drossner, 61% occurred in infants who were preterm [22. Drossner DM, Kim DW, Maher KO, Mahle WT. Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics. 2008;122:e656-61.
The association of pulmonary vein stenosis and prematurity is a relatively recent observation and is introduced in this reference.]. Secondary or acquired PVS frequently follows repair of TAPVD (7-11%) [1616. van Son JA, Danielson GK, Puga FJ, Edwards WD, Driscoll DJ. Repair of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 1995;60:144-50. , 2323. Hartyanszky IL, Huttl T, Kadar K, Koncz E, Lozsadi K. Stenosis of pulmonary veins with total left anomalous pulmonary venous return. Eur J Cardiothorac Surg. 1990;4:284-6. , 2424. Caldarone CA, Najm HK, Kadletz M, Smallhorn JF, Freedom RM, Williams WG, Coles JG. Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg. 1998; 66:1514-20. , 2525. Hyde JA, Stumper O, Barth MJ, Wright JG, Silove ED, de Giovanni JV, Brawn WJ, Sethia B. Total anomalous pulmonary venous connection: outcome of surgical correction and management of recurrent venous obstruction. Eur J Cardiothorac Surg. 1999;15:735-40; discussion 40-1. , 2626. Michielon G, Di Donato RM, Pasquini L, Giannico S, Brancaccio G, Mazzera E, Squitieri C, Catena G. Total anomalous pulmonary venous connection: long-term appraisal with evolving technical solutions. Eur J Cardiothorac Surg. 2002;22:184-91. , 2727. Haworth SG, Reid L. Structural study of pulmonary circulation and of heart in total anomalous pulmonary venous return in early infancy. Br Heart J. 1977;39: 80-92. , 2828. Yamaki S, Tsunemoto M, Shimada M, Ishizawa R, Endo M, Nakayama S, Hata M, Mohri H. Quantitative analysis of pulmonary vascular disease in total anomalous pulmonary venous connection in sixty infants. J Thorac Cardiovasc Surg. 1992;104:728-35. ]. It is unlikely that inadequate opening of the pulmonary venous confluence into the left atrium by the surgeon wholly explains the high incidence of PVS following TAPVD repair. A pre-existing developmental abnormality of the pulmonary veins is in many cases a more likely explanation. Secondary PVS is also seen following radio-frequency ablation in the left atrium for atrial fibrillation/flutter in adults [2929. Packer DL, Keelan P, Munger TM, Breen JF, Asirvatham S, Peterson LA, Monahan KH, Hauser MF, Chandrasekaran K, Sinak LJ, Holmes DR Jr. Clinical presentation, investigation, and management of pulmonary vein stenosis complicating ablation for atrial fibrillation. Circulation. 2005;111:546-54. , 3030. Purerfellner H, Aichinger J, Martinek M, Nesser HJ, Cihal R, Gschwendtner M, Dierneder J. Incidence, management, and outcome in significant pulmonary vein stenosis complicating ablation for atrial fibrillation. Am J Cardiol. 2004;93:1428-31, A10. ]. The pathology and outcome here is different and is considered separately.
The pathogenesis of PVS is poorly defined beyond the recognition that fibrous intimal thickening and medial hypertrophy occur rapidly [2020. Driscoll DJ, Hesslein PS, Mullins CE. Congenital stenosis of individual pulmonary veins: clinical spectrum and unsuccessful treatment by transvenous balloon dilation. Am J Cardiol. 1982;49:1767-72. , 3131. Thapar MK, Riff E, Halees Z. Intrapulmonary agenesis of venous system and bronchopulmonary arterial anastomosis. Br Heart J. 1991;66:182-4. , 3232. Mehta AV, Chidambaram B. Absent left pulmonary vein without anomalous connection: diagnosis and management in the newborn. Am Heart J. 1992;124:804-6. , 3333. Kingston HM, Patel RG, Watson GH. Unilateral absence or extreme hypoplasia of pulmonary veins. Br Heart J. 1983;49:148-53. ]. It may be of greater value to define the nature of the obstruction, as this may direct therapeutic approaches and be more strongly predictive of outcome following therapy. For primary PVS there is strong evidence to support rapid disease progression with stenosis eventually resulting in atresia developing through infancy or into early childhood. There are documented examples of normal pulmonary venous drainage on early imaging in individuals who have ultimately developed PVS within months [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence., 22. Drossner DM, Kim DW, Maher KO, Mahle WT. Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics. 2008;122:e656-61.
The association of pulmonary vein stenosis and prematurity is a relatively recent observation and is introduced in this reference., 3434. Chakrabarti S, Tsao S, Vettukattil JJ, Gnanapragasam JP. Pulmonary vein stenosis mimicking chronic lung disease. Acta Paediatr. 2003;92:857-8. , 3535. Ussia G, Marasini M, Zannini L, Pongiglione G. Acquired pulmonary vein obstruction after open-heart surgery. Eur J Cardiothorac Surg. 2002;22:465-7. ].
Obstruction for secondary PVS following TAPVD repair may be limited to the anastomosis or the pulmonary venous confluence. In some cases, however, the obstruction will be more extensive with a fibrous reaction extending along the course of the vein into the lung parenchyma or associated with a developmental hypoplasia or absence of the pulmonary veins. Obviously this last sub-type, with its origins most likely in utero, will be the most difficult to treat if treatable at all. It has yet to be established whether these difficult to manage patients can be identified with careful imaging, though many centres routinely perform high resolution cardiac computed tomography or magnetic resonance imaging frequently combined with diagnostic angiography with this intention. Some cases of secondary PVS are associated with mediastinal fibrosis [3636. Dye TE, Saab SB, Almond CH, Watson L. Sclerosing mediastinitis with occlusion of pulmonary veins. Manifestations and management. J Thorac Cardiovasc Surg. 1977;74:137-41. , 3737. Chazova I, Robbins I, Loyd J, Newman J, Tapson V, Zhdaov V, Meyrick B. Venous and arterial changes in pulmonary veno-occlusive disease, mitral stenosis and fibrosing mediastinitis. Eur Respir J. 2000;15:116-22. ]. Mediastinal fibrosis is usually idiopathic and progressive but consideration should be given to infective mediastinal fibrosing disease (excluding tuberculosis and aspergillus disease especially in the setting of immunocompromised individuals, Figure 1 ).
ACQUIRED PULMONARY VEIN STENOSIS FOLLOWING RADIO-FREQUENCY ABLATION FOR ATRIAL FIBRILLATION
Acquired pulmonary vein stenosis in adults is a rare disease and until recently was most frequently caused by extrinsic disease infiltrating and surrounding the pulmonary veins (including fibrosing mediastinitis, sarcoidosis and neoplasia). Following the advent of radio-frequency ablation for atrial fibrillation a collection of adults with secondary pulmonary vein stenosis emerged. Given the rarity of this entity and the difficulties with non-invasive imaging assessment of atrial structures in the adult it is not surprising that diagnosis is frequently delayed. Presentation is usually non-specific (such as dyspnoea and lethargy), and a heightened awareness of the possibility of this diagnosis following radio-frequency procedures is essential. As ablation strategies have evolved, pulmonary vein stenosis is now an extremely uncommon complication of this treatment.
Imaging
2-D colour-flow transthoracic echocardiography remains the imaging tool of choice in affording serial assessment of right ventricular pressure as well as identifying the number of veins involved [3838. Smallhorn JF, Pauperio H, Benson L, Freedom RM, Rowe RD. Pulsed Doppler assessment of pulmonary vein obstruction. Am Heart J. 1985;110:483-6. , 3939. Smallhorn JF, Freedom RM, Olley PM. Pulsed Doppler echocardiographic assessment of extraparenchymal pulmonary vein flow. J Am Coll Cardiol. 1987;9:573-9. , 4040. Minich LL, Tani LY, Breinholt JP, Tuohy AM, Shaddy RE. Complete follow-up echocardiograms are needed to detect stenosis of normally connecting pulmonary veins. Echocardiography. 2001;18:589-92. , 4141. Smallhorn JF, Burrows P, Wilson G, Coles J, Gilday DL, Freedom RM. Two-dimensional and pulsed Doppler echocardiography in the postoperative evaluation of total anomalous pulmonary venous connection. Circulation. 1987;76:298-305. ] ( Figure 2 ). Pulmonary veins are potentially obstructed on echocardiography if the pulsed-wave Doppler of the pulmonary vein shows non-phasic flow or a velocity exceeding 1.6 m/s [4242. Webber SA, de Souza E, Patterson MW. Pulsed wave and color Doppler findings in congenital pulmonary vein stenosis. Pediatr Cardiol. 1992;13:112-5. ]. All new cases of congenital heart disease and all postoperative patients should have all pulmonary veins carefully interrogated. Chest radiographs can be difficult to interpret with single-sided pulmonary venous obstruction as some patients demonstrate ipsilateral signs of pulmonary plethora and pulmonary venous hypertension whilst others demonstrate signs in the contralateral lung because of the maldistribution of blood flow that eventually results [4343. Swischuk LE, L’Heureux P. Unilateral pulmonary vein atresia. AJR Am J Roentgenol. 1980;135:667-72. , 4444. Johnson JF, Juris AL, Barnes EV. Bronchial arteries to right pulmonary artery anastomoses in right pulmonary vein atresia. Cardiovasc Intervent Radiol. 1982;5:238-40. ]. Pulmonary perfusion scans rarely help with decision making. Acoustic windows especially in older patients can limit the sensitivity of echocardiography and in the setting of clinical suspicion of pulmonary venous obstruction cardiac high resolution spiral computed tomography or magnetic resonance imaging is increasingly being employed to define the sites of obstruction with or without angiography. Computed tomography has advantages in infants, achieving greater resolution than magnetic resonance imaging and frequently obviating the need for general anaesthesia in view of the speed of image acquisition ( Figure 1 ) [4545. Ou P, Marini D, Celermajer DS, Agnoletti G, Vouhé P, Sidi D, Bonnet D, Brunelle F. Non-invasive assessment of congenital pulmonary vein stenosis in children using cardiac-non-gated CT with 64-slice technology. Eur J Radiol. 2009;70:595-9. ]. Magnetic resonance (MR) imaging with angiography will avoid radiation exposure and is preferred in many units performing MR scans in infants under general anaesthesia ( Figure 3 ). MR has the advantage of enabling assessment of right ventricular pressures and flow assessments for accurate quantification of pulmonary vascular resistance in combination with a transpulmonary gradient obtained with a hybrid catheter study [4646. Muthurangu V, Taylor A, Andriantsimiavona R, Hegde S, Miquel ME, Tulloh R, Baker E, Hill DL, Razavi RS. Novel method of quantifying pulmonary vascular resistance by use of simultaneous invasive pressure monitoring and phase-contrast magnetic resonance flow. Circulation. 2004;110:826-34. , 4747. Kuehne T, Yilmaz S, Schulze-Neick I, Wellnhofer E, Ewert P, Nagel E, Lange P. Magnetic resonance imaging guided catheterisation for assessment of pulmonary vascular resistance: in vivo validation and clinical application in patients with pulmonary hypertension. Heart. 2005;91:1064-9. ]. Surgical decisions may be made at this point depending on institutional preference or following diagnostic catheterisation studies. Our practice is to perform angiography as well as non-invasive imaging assessments with MR or CT. The reasons for this include an accurate assessment of pulmonary vascular resistance but more importantly an attempt at defining the exact nature of the underlying obstructive disease. Angiographic definitions of pulmonary venous obstruction can be difficult though a reduction in overall diameter to <50% of the vessel diameter, slowed return of contrast from the obstructed lung segment and a mean gradient through the stenosis >5 mmHg would be strongly supportive.
Surgical treatment options
The surgical options available to manage both primary and secondary PVS are beyond the scope of this chapter, which can only offer a brief discussion of the options against which to position the role of catheter-based intervention. Many surgical approaches have been tried including anastomotic revision for secondary PVS, intraoperative stent placement, patch venoplasty, dilation and scar excision and sutureless pericardial marsupialisation [2525. Hyde JA, Stumper O, Barth MJ, Wright JG, Silove ED, de Giovanni JV, Brawn WJ, Sethia B. Total anomalous pulmonary venous connection: outcome of surgical correction and management of recurrent venous obstruction. Eur J Cardiothorac Surg. 1999;15:735-40; discussion 40-1. , 4848. Najm HK, Caldarone CA, Smallhorn J, Coles JG. A sutureless technique for the relief of pulmonary vein stenosis with the use of in situ pericardium. J Thorac Cardiovasc Surg. 1998;115:468-70. , 4949. Lacour-Gayet F, Rey C, Planche C. Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ. Arch Mal Coeur Vaiss. 1996;89:633-6. , 5050. Ricci M, Elliott M, Cohen GA, Catalan G, Stark J, de Leval MR, Tsang VT. Management of pulmonary venous obstruction after correction of TAPVC: risk factors for adverse outcome. Eur J Cardiothorac Surg. 2003;24:28-36; discussion ]. Sutureless repair techniques involve reconstituting atrial tissue to pericardium with the intent of avoiding left atrial suture lines. There are some encouraging reports of success following these methods [2525. Hyde JA, Stumper O, Barth MJ, Wright JG, Silove ED, de Giovanni JV, Brawn WJ, Sethia B. Total anomalous pulmonary venous connection: outcome of surgical correction and management of recurrent venous obstruction. Eur J Cardiothorac Surg. 1999;15:735-40; discussion 40-1. , 4848. Najm HK, Caldarone CA, Smallhorn J, Coles JG. A sutureless technique for the relief of pulmonary vein stenosis with the use of in situ pericardium. J Thorac Cardiovasc Surg. 1998;115:468-70. , 4949. Lacour-Gayet F, Rey C, Planche C. Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ. Arch Mal Coeur Vaiss. 1996;89:633-6. ]. Each report is retrospective and none compares directly the efficacy of surgery versus catheter treatment and usually both treatments are used collaboratively. It is also likely that different patient populations are described since catheter treatments are often performed only when all other options have been exhausted. Nevertheless, Devaney and others report some of the most optimistic results for the management of this disease [44. Devaney EJ, Chang AC, Ohye RG, Bove EL. Management of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 2006;81:992-5; discussion 995-6.
This reference begins to discuss the treatment options available in the context of a series of 36 cases., 2424. Caldarone CA, Najm HK, Kadletz M, Smallhorn JF, Freedom RM, Williams WG, Coles JG. Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg. 1998; 66:1514-20. , 2525. Hyde JA, Stumper O, Barth MJ, Wright JG, Silove ED, de Giovanni JV, Brawn WJ, Sethia B. Total anomalous pulmonary venous connection: outcome of surgical correction and management of recurrent venous obstruction. Eur J Cardiothorac Surg. 1999;15:735-40; discussion 40-1. , 4949. Lacour-Gayet F, Rey C, Planche C. Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ. Arch Mal Coeur Vaiss. 1996;89:633-6. , 5050. Ricci M, Elliott M, Cohen GA, Catalan G, Stark J, de Leval MR, Tsang VT. Management of pulmonary venous obstruction after correction of TAPVC: risk factors for adverse outcome. Eur J Cardiothorac Surg. 2003;24:28-36; discussion ]. Among 11 patients with acquired PVS who underwent surtureless pericardial marsupialisation there was only one late death secondary to restenosis [44. Devaney EJ, Chang AC, Ohye RG, Bove EL. Management of congenital and acquired pulmonary vein stenosis. Ann Thorac Surg. 2006;81:992-5; discussion 995-6.
This reference begins to discuss the treatment options available in the context of a series of 36 cases., 2424. Caldarone CA, Najm HK, Kadletz M, Smallhorn JF, Freedom RM, Williams WG, Coles JG. Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg. 1998; 66:1514-20. , 4949. Lacour-Gayet F, Rey C, Planche C. Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ. Arch Mal Coeur Vaiss. 1996;89:633-6. ].
Catheter indications
Most institutions consider intervening on pulmonary veins after exhausting surgical approaches in the symptomatic child with systemic level or greater right ventricular pressures. In the asymptomatic child with single vein involvement and right ventricular pressures which are not particularly elevated, observation would seem prudent given the potential risks of intervention and the lack of evidence to support improved long-term outcome. Occasionally intervention has been performed on pulmonary veins as short-term palliation before surgery or to improve the possibility of a better surgical result, for example on obstructed descending and vertical veins in TAPVD [5151. Kitano M, Yazaki S, Kagisaki K, Kurosaki K. Primary palliative stenting against obstructive mixed-type total anomalous pulmonary venous connection associated with right atrial isomerism. J Interv Cardiol. 2009;22:404-9.
Although a rare procedure this report is highly innovative in bridging an infant to surgery by stenting an obstructed descending vein in the context of obstructed total anomalous pulmonary venous drainage. Lateral thinking such as this may prove beneficial in such rare and complex cases., 5252. Jhang WK, Chang YJ, Park CS, Oh YM, Kim YH, Yun TJ. Hybrid palliation for right atrial isomerism associated with obstructive total anomalous pulmonary venous drainage. Interact Cardiovasc Thorac Surg. 2008;7:282-4. , 5353. Wong DT, Yoo SJ, Lee KJ. Implantation of drug-eluting stents for relief of obstructed infra-cardiac totally anomalous pulmonary venous connection in isomerism of the right atrial appendages. Cardiol Young. 2008; 18:628-30. ]. Following growth, this may allow surgery on a more stable infant and is a potentially life-saving therapy.
Angioplasty might be usefully performed in a suture line anastomotic obstruction where the pulmonary venous confluence opens into the left atrium. However, it is the authors’ and others’ experience that obstruction secondary to surgical technique is rarely the cause of secondary PVS, with a more insidious developmental abnormality of the pulmonary veins being more likely and, as discussed above, less responsive to therapy. Many institutions favour further surgery using a sutureless technique as the initial approach to these patients. Stents will continue to be placed in primary and secondary PVS but generally most interventionists will place a stent only after failed angioplasty or in a high-risk situation where a good short-term result needs to be achieved, such as in a child on a ventilator with severe pulmonary hypertension. The child will, however, be committed to future procedures for in-stent stenosis.
Catheterization procedure
PREPARATION AND ACCESS
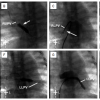
The goals of the procedure are set jointly by the cardiology and surgical teams. Quantifying risks can also be problematic but they are probably similar to the risk of performing a diagnostic catheter study in a pulmonary hypertensive child. These risks have been considered in the literature and can be used as a guide [5454. Taylor CJ, Derrick G, McEwan A, Haworth SG, Sury MR. Risk of cardiac catheterization under anaesthesia in children with pulmonary hypertension. Br J Anaesth. 2007;98:657-61. ]. General anaesthesia is indicated and appropriate planning with the anaesthetist and post-procedure intensive care team should be arranged. One unit of blood needs to be readily available. Femoral venous access improves the chances of crossing the atrial septum through a patent foramen ovale if present. Access from the inferior caval vein also improves the catheter approach to the right-sided veins which can be difficult, though not impossible, to access if approaching from the internal jugular vein. For interrupted inferior caval vein with azygous continuation or bilateral femoral vein occlusion a transhepatic approach is favoured over the internal jugular vein approach for the same reason. We routinely place a 4 French (Fr) arterial sheath for arterial pressure monitoring, confirming a normal left ventricular end-diastolic pressure and to check arterial blood gases periodically. As procedures can be prolonged and are performed on the left side of the circulation, full heparinisation is appropriate after crossing the atrial septum in case transseptal puncture is necessary (heparin sulphate 100 IU/kg iv and then to maintain an ACT >200s). Systemic emboli is a common complication either from the long sheaths and long duration of the procedure or from thrombus in partially obstructed or near atretic veins that are then openend during the procedure. Transseptal puncture in infants is potentially hazardous as the left atrium is usually small and the atrial septum hypertrophied. We prefer to use a radio-frequency wire with a coaxial catheter such as the system available from Baylis (Montreal, QC, Canada) as this affords greater control ( Figure 4 ) but standard Brockenbrough needle approaches can be used in older children. Prophylactic antibiotics are given by some to cover the procedure. A blood gas should be checked before recording haemodynamic data and the endotracheal tube position confirmed. The lung fields should be viewed on brief fluoroscopy for lobar collapse.
HAEMODYNAMICS
Right heart haemodynamic data can be obtained with a 4-5 Fr multipurpose, a 4-5 Fr Judkins right coronary or a 5-6 Fr balloon wedge catheter depending on preference. Attention should be given to the inspired oxygen content. In practice it can be difficult to keep this to less than 30% in unstable patients; blood gases will therefore need to be taken alongside haemodynamic data to calculate dissolved oxygen. The minimal set of pressures, saturations and blood gases required are inferior and superior caval veins, right atrium, pulmonary artery, left atrium and aorta. If the atrial septum cannot be crossed a pulmonary venous wedge pressure will suffice as approximating left atrial pressure.
ANGIOGRAPHY
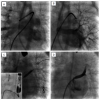
Selective or non-selective pulmonary artery wedge angiograms can be a productive place to start following collection of haemodynamic data and are often highly informative as to the site, number and severity of stenoses. An angiogram can be performed with a balloon wedge catheter, a pigtail catheter or a multipurpose catheter either in each pulmonary artery separately or in each individual lobar branch. Layered neat non-ionic contrast media (10 mls) with either saline or aspirated blood (10 mls) can be injected rapidly by hand (20 mls leurlocked syringe) to define the course of the pulmonary venous return. These images are usually best acquired straight anteroposterior and straight lateral until the site of obstruction is defined ( Figure 1 ).
PULMONARY VEIN CANNULATION
Following wedge angiograms the atrial septum is crossed either directly or via a transseptal puncture with a Brockenbrough needle or a radio-frequency wire as already discussed. A guiding sheath can then be placed and heparin given if it has not been given already. The left-sided upper and lower veins are usually easily entered from an inferior caval vein approach. Right-sided veins can be more difficult and several catheters may need to be tried, sometimes employing the roof of the left atrium to increase the curve on the catheter. A guidewire may be useful such as a Terumo 0.035’ wire (Terumo Europe, Leuven, Belgium). Engagement should be attempted with a 5 Fr multipurpose catheter with consideration given to changing to a cobra glide catheter (Boston Scientific, Natick, MA, USA) if the former were unsuccessful. The Judkins right coronary catheter can also be gainfully employed. The pressure gradient across the target lesion should be recorded. If catheter position has been difficult to obtain then a second venous sheath will allow simultaneous left atrial and proximal vein pressure measurements to be obtained without losing position of the catheter and ultimately wire position. Selective hand angiograms should be obtained with neat contrast. The right-sided veins are often best profiled in a straight anteroposterior or right anterior oblique and lateral projection with the left-sided veins requiring some left anterior oblique and cranial angulation. Optimal profiling will require further alteration of angulation after obtaining initial angiographic images depending on the location of the stenosis [5555. Tang M, Gerds-Li JH, Nedios S, Roser M, Fleck E, Kriatselis C. Optimal fluoroscopic projections for angiographic imaging of the pulmonary vein ostia: lessons learned from the intraprocedural reconstruction of the left atrium and pulmonary veins. Europace. 2010;12:37-44. ].
Catheter intervention
ANGIOPLASTY
Angioplasty for PVS has been performed for more than two decades [5656. Qureshi AM, Prieto LR, Latson LA, Lane GK, Mesia CI, Radvansky P, White RD, Marrouche NF, Saad EB, Bash DL, Natale A, Rhodes JF. Transcatheter angioplasty for acquired pulmonary vein stenosis after radiofrequency ablation. Circulation. 2003;108:1336-42.
A review of 19 cases of radiofrequency-induced acquired pulmonary vein stenosis., 5757. Lock JE, Bass JL, Castaneda-Zuniga W, Fuhrman BP, Rashkind WJ, Lucas RV Jr. Dilation angioplasty of congenital or operative narrowings of venous channels. Circulation. 1984;70:457-64.
This early paper in the transcatheter experience of balloon angioplasty of venous obstructive lesions is a useful read in highlighting the complications and difficulties likely to be encountered., 5858. Wax DF, Rocchini AP. Transcatheter management of venous stenosis. Pediatr Cardiol. 1998;19:59-65; discussion 6. ]. Short-term improvement is clearly documented including improvement in symptoms [66. Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB. Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Cardiovasc Catheter Interv. 2010;75:1084-90.
Cutting balloon angioplasty has proved useful in severely stenotic pulmonary arterial lesions and although it continues to have its advocates for pulmonary vein stenosis the results are not particularly promising.]. However, the improvement is short-lived and in most restenosis is evident by 3-6 months following the initial dilatation. It is for this reason that other methods have been tried, but due to the rarity of the lesion there are no studies directly comparing one procedure against another. In view of the fact that no procedure has proved itself superior, many operators perform angioplasty initially only proceeding to cutting balloons or stent placement if the lesion is fixed or there is marked elastic recoil respectively. If a good result is realised with angioplasty the procedure may be discontinued at this point and clinical progress observed. Drug eluting balloons can be tried but there is as yet no evidence that these yield a superior result.
Interventional management
- Multiple procedures may be necessary and angioplasty is the initial technique of choice [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence.]
- In the presence of a fixed lesion, despite high inflation pressures of a non-compliant angioplasty balloon, a cutting balloon might be considered [55. Seale AN, Daubeney PE, Magee AG, Rigby ML. Pulmonary vein stenosis: initial experience with cutting balloon angioplasty. Heart. 2006;92:815-20. , 66. Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB. Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Cardiovasc Catheter Interv. 2010;75:1084-90.
Cutting balloon angioplasty has proved useful in severely stenotic pulmonary arterial lesions and although it continues to have its advocates for pulmonary vein stenosis the results are not particularly promising.]
- Where there is significant recoil of a lesion and the clinical circumstances demand a good result, a stent may be placed [77. Mendelsohn AM, Bove EL, Lupinetti FM, Crowley DC, Lloyd TR, Fedderly RT, Beekman RH 3rd. Intraoperative and percutaneous stenting of congenital pulmonary artery and vein stenosis. Circulation. 1993;88:II210-7.
Following the above experience with balloon angioplasty it was only a matter of time before stents would be placed into pulmonary veins. The results are universally disappointing.]
ANGIOPLASTY TECHNIQUE
The stenosed pulmonary vein should be cannulated as distally as possible to improve wire position. Several wires can be used and the choice will depend to some extent on the age of the child and the catheter position achieved. The floppy part of the wire needs to be beyond the stenosis to provide a secure scaffold for delivering and retrieving various-sized angioplasty balloons. 0.014’ coronary wires such as heavy weight or middle weight wires are particularly useful in infants (Abbott Vascular, Abbott Park, IL, USA). Two coronary wires (‘buddy wire’) can increase the amount of support and aid tracking of the angioplasty balloon ( Figure 4 ). Several coronary wires may need to be tried if it is difficult crossing a tight lesion.
Angioplasty should increase the diameter of the narrowed lesion by a factor of 3, aiming to achieve a size similar to the distal vessel diameter if possible ( Figure 5 ). This might involve using a smaller balloon followed by a larger one. The first inflation is useful in assessing the recoil of the vessel and the likelihood of achieving a good result with angioplasty alone. Again, coronary balloons are particularly useful in small infants though other non-compliant larger balloons will be required in larger patients (for example Balt Cristal [Synapse, Dublin, Ireland] and Opta® pro non-compliant balloons [Cordis, Johnson & Johnson, Warren, NJ, USA] amongst others).
CUTTING BALLOONS
Poor results from conventional balloon angioplasty led to exploration of cutting balloon angioplasty [2020. Driscoll DJ, Hesslein PS, Mullins CE. Congenital stenosis of individual pulmonary veins: clinical spectrum and unsuccessful treatment by transvenous balloon dilation. Am J Cardiol. 1982;49:1767-72. , 5757. Lock JE, Bass JL, Castaneda-Zuniga W, Fuhrman BP, Rashkind WJ, Lucas RV Jr. Dilation angioplasty of congenital or operative narrowings of venous channels. Circulation. 1984;70:457-64.
This early paper in the transcatheter experience of balloon angioplasty of venous obstructive lesions is a useful read in highlighting the complications and difficulties likely to be encountered., 5959. Sugiyama H, Veldtman GR, Norgard G, Lee KJ, Chaturvedi R, Benson LN. Bladed balloon angioplasty for peripheral pulmonary artery stenosis. Catheter Cardiovasc Interv. 2004;62:71-7. ] alone or more likely in combination with angioplasty and drug euting balloons. These can be used safely in infants albeit with long procedure times [55. Seale AN, Daubeney PE, Magee AG, Rigby ML. Pulmonary vein stenosis: initial experience with cutting balloon angioplasty. Heart. 2006;92:815-20. ]. As with standard balloon angioplasty, results are not sustained and repeat procedure is likely to be required within 6 months [66. Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB. Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Cardiovasc Catheter Interv. 2010;75:1084-90.
Cutting balloon angioplasty has proved useful in severely stenotic pulmonary arterial lesions and although it continues to have its advocates for pulmonary vein stenosis the results are not particularly promising.]. Short-term improvements in vessel calibre, right ventricular pressure and pulmonary artery resistance and improvement in patient symptoms can be expected [55. Seale AN, Daubeney PE, Magee AG, Rigby ML. Pulmonary vein stenosis: initial experience with cutting balloon angioplasty. Heart. 2006;92:815-20. ]. Superiority of cutting balloon angioplasty over conventional angioplasty techniques is suggested by a number of authors but no randomised comparison has been performed [66. Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB. Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Cardiovasc Catheter Interv. 2010;75:1084-90.
Cutting balloon angioplasty has proved useful in severely stenotic pulmonary arterial lesions and although it continues to have its advocates for pulmonary vein stenosis the results are not particularly promising.]. Cutting balloon angioplasty has also been performed in adults with PVS following radio-frequency ablation procedures [5656. Qureshi AM, Prieto LR, Latson LA, Lane GK, Mesia CI, Radvansky P, White RD, Marrouche NF, Saad EB, Bash DL, Natale A, Rhodes JF. Transcatheter angioplasty for acquired pulmonary vein stenosis after radiofrequency ablation. Circulation. 2003;108:1336-42.
A review of 19 cases of radiofrequency-induced acquired pulmonary vein stenosis., 6060. Saad EB, Marrouche NF, Saad CP, Ha E, Bash D, White RD, Rhodes J, Prieto L, Martin DO, Saliba WI, Schweikert RA, Natale A. Pulmonary vein stenosis after catheter ablation of atrial fibrillation: emergence of a new clinical syndrome. Ann Intern Med. 2003;138:634-8. , 6161. Saad EB, Rossillo A, Saad CP, Martin DO, Bhargava M, Erciyes D, Bash D, Williams-Andrews M, Beheiry S, Marrouche NF, Adams J, Pisanò E, Fanelli R, Potenza D, Raviele A, Bonso A, Themistoclakis S, Brachmann J, Saliba WI, Schweikert RA, Natale A. Pulmonary vein stenosis after radiofrequency ablation of atrial fibrillation: functional characterization, evolution, and influence of the ablation strategy. Circulation. 2003;108:3102-7. ].
CUTTING BALLOON TECHNIQUE
A wire is placed in the stenosed pulmonary vein for stability as described above and a 6 Fr guiding sheath placed over the wire to protect the cardiac structures from the cutting balloon. Cutting balloons range from 2.25 mm to 8 mm in diameter (Boston Scientific, Natick, MA, USA). A manometer should be used to ensure the recommended pressures are not exceeded (8-10 atm). Care should be taken to bring the balloon back into the guiding sheath and the blades should be checked on removal from the body.
STENT PLACEMENT
Results from stent placement in PVS are difficult to evaluate by comparison with angioplasty or cutting balloon angioplasty as they are likely to be used when the initial angioplasty result is regarded by the operator as sub-optimal ( Figure 6) [77. Mendelsohn AM, Bove EL, Lupinetti FM, Crowley DC, Lloyd TR, Fedderly RT, Beekman RH 3rd. Intraoperative and percutaneous stenting of congenital pulmonary artery and vein stenosis. Circulation. 1993;88:II210-7.
Following the above experience with balloon angioplasty it was only a matter of time before stents would be placed into pulmonary veins. The results are universally disappointing., 6262. Ungerleider RM, Johnston TA, O’Laughlin MP, Jaggers JJ, Gaskin PR. Intraoperative stents to rehabilitate severely stenotic pulmonary vessels. Ann Thorac Surg. 2001;71:476-81. , 6363. Tomita H, Watanabe K, Yazaki S, Kimura K, Ono Y, Yagihara T, Echigo S. Stent implantation and subsequent dilatation for pulmonary vein stenosis in pediatric patients: maximizing effectiveness. Circ J. 2003;67:187-90.
There may be a place for serial stent dilatation to achieve a sufficient intraluminal diameter in order to reduce the risk of neointimal proliferation and stent restenosis. Such an aggressive approach remains unproven., 6464. Tomita H, Watanabe K, Yazaki S, Kimura K, Ono Y, Yagihara T, Echigo S. Stent implantation and subsequent dilatation for pulmonary vein stenosis in pediatric patients: maximizing effectiveness. Circ J. 2003;67:187-90. , 6565. Vance MS, Bernstein R, Ross BA. Successful stent treatment of pulmonary vein stenosis following atrial fibrillation radiofrequency ablation. J Invasive Cardiol. 2002;14:414-6. , 6666. Doyle TP, Loyd JE, Robbins IM. Percutaneous pulmonary artery and vein stenting: a novel treatment for mediastinal fibrosis. Am J Respir Crit Care Med. 2001;164:657-60. , 6767. Dieter RS, Nelson B, Wolff MR, Thornton F, Grist TM, Cohen DM. Transseptal stent treatment of anastomotic stricture after repair of partial anomalous pulmonary venous return. J Endovasc Ther. 2003;10:838-42. , 6868. Michel-Behnke I, Luedemann M, Hagel KJ, Schranz D. Serial stent implantation to relieve in-stent stenosis in obstructed total anomalous pulmonary venous return. Pediatr Cardiol. 2002;23:221-3. , 6969. Coulson JD, Bullaboy CA. Concentric placement of stents to relieve an obstructed anomalous pulmonary venous connection. Cathet Cardiovasc Diagn. 1997;42: 201-4. ]. Although short-term results are good, significant in-stent stenosis occurs quickly and is a major problem. Further stents, intrastent sonotherapy [7070. O’Laughlin MP, Perry SB, Lock JE, Mullins CE. Use of endovascular stents in congenital heart disease. Circulation. 1991;83:1923-39. ], drug-eluting stents or PTFE-covered stents [7171. McMahon CJ, Mullins CE, El Said HG. Intrastent sonotherapy in pulmonary vein restenosis: a new treatment for a recalcitrant problem. Heart. 2003;89:E6. ] have all been used to try to combat this but with no evidence of a superior result. Animal stent models do exist and may be useful in the future for trialling drug delivery stents to combat rapidly occurring in-stent stenosis [7272. Gordon BM, Moore JW. Treatment of pulmonary vein stenosis with expanded polytetrafluoroethylene covered stents. Catheter Cardiovasc Interv;75:263-7. ]. A variety of stents are available. In infants coronary stents are commonly used as larger stents are frequently too difficult to place. Experience with coronary stents suggests that even a 4 mm stent can be dilated to 7-8 mm serially [7373. Hosking M, Redmond M, Allen L, Broecker L, Keaney M, Lebeau J, Walley V. Responses of systemic and pulmonary veins to the presence of an intravascular stent in a swine model. Cathet Cardiovasc Diagn. 1995;36: 90-6; discussion 7. ]. However, whilst short-term results with coronary stents are acceptable, early restenosis does occur and ultimately they are limited by the child’s growth. Whether the rate of in-stent stenosis can be slowed or delayed with drug-eluting stents or even systemic chemotherapy remains to be established [7474. Bentham J, Shettihalli N, Orchard E, Westaby S, Wilson N. Endovascular stent placement is an acceptable alternative to reoperation in selected infants with residual or recurrent aortic arch obstruction. Catheter Cardiovasc Interv. ]. Genesis stents (Cordis, Johnson & Johnson, Warren, NJ, USA) have also been used effectively; these can be delivered through a 5 or 6 Fr guiding sheath and are capable of reaching larger sizes in older children. Covered stents have also been used more recently (smallest 7 mm x 16 mm stent) [7171. McMahon CJ, Mullins CE, El Said HG. Intrastent sonotherapy in pulmonary vein restenosis: a new treatment for a recalcitrant problem. Heart. 2003;89:E6. ]. Stents should generally not be used if a fixed lesion is present, though a cutting balloon might be used followed by a stent. They are of use in difficult circumstances where a good result needs to be achieved and angioplasty has been unsuccessful, for example where there is significant recoil of a lesion or a dissection flap has been raised following angioplasty.
Stents can also be placed in obstructed descending or vertical veins in TAPVD before surgical correction. Angioplasty has been effectively performed for this indication though stent placement may be more appropriate since the cause is usually fixed compression [7575. Dragulescu A, Ghez O, Quilici J, Fraisse A. Paclitaxel drug-eluting stent placement for pulmonary vein stenosis as a bridge to heart-lung transplantation. Pediatr Cardiol. 2009;30:1169-71. , 7676. Bu’Lock FA, Jordan SC, Martin RP. Successful balloon dilatation of ascending vein stenosis in obstructed supracardiac total anomalous pulmonary venous connection. Pediatr Cardiol. 1994;15:78-80. ]. This may be particularly useful to ameliorate the preoperative condition of the collapsed neonate presenting with pulmonary venous obstruction [7777. Ramakrishnan S, Kothari SS. Preoperative balloon dilatation of obstructed total anomalous pulmonary venous connection in a neonate. Catheter Cardiovasc Interv. 2004;61:128-30. , 7878. Lo-A-Njoe SM, Blom NA, Bokenkamp R, Ottenkamp J. Stenting of the vertical vein in obstructed total anomalous pulmonary venous return as rescue procedure in a neonate. Catheter Cardiovasc Interv. 2006;67:668-70. ]. In the setting of a univentricular circulation this may be sufficient to enable growth and delay surgery through to bicaval bidirectional anastomosis [5151. Kitano M, Yazaki S, Kagisaki K, Kurosaki K. Primary palliative stenting against obstructive mixed-type total anomalous pulmonary venous connection associated with right atrial isomerism. J Interv Cardiol. 2009;22:404-9.
Although a rare procedure this report is highly innovative in bridging an infant to surgery by stenting an obstructed descending vein in the context of obstructed total anomalous pulmonary venous drainage. Lateral thinking such as this may prove beneficial in such rare and complex cases., 5252. Jhang WK, Chang YJ, Park CS, Oh YM, Kim YH, Yun TJ. Hybrid palliation for right atrial isomerism associated with obstructive total anomalous pulmonary venous drainage. Interact Cardiovasc Thorac Surg. 2008;7:282-4. , 5353. Wong DT, Yoo SJ, Lee KJ. Implantation of drug-eluting stents for relief of obstructed infra-cardiac totally anomalous pulmonary venous connection in isomerism of the right atrial appendages. Cardiol Young. 2008; 18:628-30. , 6767. Dieter RS, Nelson B, Wolff MR, Thornton F, Grist TM, Cohen DM. Transseptal stent treatment of anastomotic stricture after repair of partial anomalous pulmonary venous return. J Endovasc Ther. 2003;10:838-42. , 6868. Michel-Behnke I, Luedemann M, Hagel KJ, Schranz D. Serial stent implantation to relieve in-stent stenosis in obstructed total anomalous pulmonary venous return. Pediatr Cardiol. 2002;23:221-3. ].
Intraoperative stent placement
Stents can be placed intraoperatively [77. Mendelsohn AM, Bove EL, Lupinetti FM, Crowley DC, Lloyd TR, Fedderly RT, Beekman RH 3rd. Intraoperative and percutaneous stenting of congenital pulmonary artery and vein stenosis. Circulation. 1993;88:II210-7.
Following the above experience with balloon angioplasty it was only a matter of time before stents would be placed into pulmonary veins. The results are universally disappointing., 6262. Ungerleider RM, Johnston TA, O’Laughlin MP, Jaggers JJ, Gaskin PR. Intraoperative stents to rehabilitate severely stenotic pulmonary vessels. Ann Thorac Surg. 2001;71:476-81. ] although this is a very rare procedure since access can generally be obtained with perseverance using transcatheter techniques
Post-intervention assessment
Intensive care or high dependency support following these procedures is prudent as the patient is at a significant risk of a pulmonary hypertensive crisis. The usual monitoring procedures of access sites should be followed as per local institution preference. Close surveillance is necessary for follow-up and children are usually reviewed within 4 weeks following the procedure. Echocardiography is often sufficient to monitor progress.
Outcome analysis
Regardless of aetiology the prognosis for paediatric patients with PVS remains poor. There is a suggestion from published series that early surgical intervention in suitable cases with sutureless techniques may be associated with better outcomes, but this is far from proven and remains hotly debated. The difficulty lies in identifying those cases likely to benefit. Diagnosis in infancy, markedly elevated mean pulmonary artery pressure, multiple vein involvement and congenital rather than acquired disease may be associated with a worse outcome [33. Holt DB, Moller JH, Larson S, Johnson MC. Primary pulmonary vein stenosis. Am J Cardiol. 2007;99:568-72.
This reference searches the Pediatric Cardiac Care Consortium Database to identify 31 cases from which to attempt to clarify prognostic predictive factors for adverse outcomes.]. In those cases not deemed suitable for surgical intervention two-year survivals of 40-50% are consistently reported across case series [11. Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY, McCarthy KP, Jones S, Shaughnessy L, Sunnegardh J, Hanseus K, Rigby ML, Keeton BR, Daubeney PE; British Congenital Heart Association. Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart. 2009;95:1944-9.
This and the second reference in this bibliography are the largest reported collection of cases to document the high mortality and morbidity associated with this condition and also to give an estimate of its incidence., 22. Drossner DM, Kim DW, Maher KO, Mahle WT. Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics. 2008;122:e656-61.
The association of pulmonary vein stenosis and prematurity is a relatively recent observation and is introduced in this reference., 66. Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB. Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Cardiovasc Catheter Interv. 2010;75:1084-90.
Cutting balloon angioplasty has proved useful in severely stenotic pulmonary arterial lesions and although it continues to have its advocates for pulmonary vein stenosis the results are not particularly promising., 7979. Vincent RN, Diehl HJ. Unusual stents in infants with severe congenital heart disease. J Interv Cardiol 2003; 16:189-91. , 8080. Jenkins KJ, Sanders SP, Orav EJ, Coleman EA, Mayer JE Jr, Colan SD. Individual pulmonary vein size and survival in infants with totally anomalous pulmonary venous connection. J Am Coll Cardiol. 1993;22:201-6. ]. It is particularly problematic comparing outcomes between different techniques as published series are small, retrospective and not randomised. Given that it is likely that more severe cases would undergo a catheter rather than a surgical procedure it is not possible to compare the two approaches. Rapid restenosis is well documented with all catheter interventions [33. Holt DB, Moller JH, Larson S, Johnson MC. Primary pulmonary vein stenosis. Am J Cardiol. 2007;99:568-72.
This reference searches the Pediatric Cardiac Care Consortium Database to identify 31 cases from which to attempt to clarify prognostic predictive factors for adverse outcomes., 77. Mendelsohn AM, Bove EL, Lupinetti FM, Crowley DC, Lloyd TR, Fedderly RT, Beekman RH 3rd. Intraoperative and percutaneous stenting of congenital pulmonary artery and vein stenosis. Circulation. 1993;88:II210-7.
Following the above experience with balloon angioplasty it was only a matter of time before stents would be placed into pulmonary veins. The results are universally disappointing., 6262. Ungerleider RM, Johnston TA, O’Laughlin MP, Jaggers JJ, Gaskin PR. Intraoperative stents to rehabilitate severely stenotic pulmonary vessels. Ann Thorac Surg. 2001;71:476-81. ]. The concerning lack of evidence that an intervention alters the natural progression of the disease means that therapy needs to be directed towards achieving symptomatic improvement.
Predictors of poor outcome or rapid progression of disease that might guide the timing of intervention and the type of intervention performed are lacking. Earlier age of onset particularly in infancy, multiple involved veins, associated cardiac malformation and higher initial pulmonary artery pressure are identified variables but are not especially helpful in the day-to-day management of an individual case [33. Holt DB, Moller JH, Larson S, Johnson MC. Primary pulmonary vein stenosis. Am J Cardiol. 2007;99:568-72.
This reference searches the Pediatric Cardiac Care Consortium Database to identify 31 cases from which to attempt to clarify prognostic predictive factors for adverse outcomes.]. Primary PVS may also be a worse prognostic variable than secondary or acquired PVS following repair of TAPVD [2727. Haworth SG, Reid L. Structural study of pulmonary circulation and of heart in total anomalous pulmonary venous return in early infancy. Br Heart J. 1977;39: 80-92. , 2828. Yamaki S, Tsunemoto M, Shimada M, Ishizawa R, Endo M, Nakayama S, Hata M, Mohri H. Quantitative analysis of pulmonary vascular disease in total anomalous pulmonary venous connection in sixty infants. J Thorac Cardiovasc Surg. 1992;104:728-35. , 5050. Ricci M, Elliott M, Cohen GA, Catalan G, Stark J, de Leval MR, Tsang VT. Management of pulmonary venous obstruction after correction of TAPVC: risk factors for adverse outcome. Eur J Cardiothorac Surg. 2003;24:28-36; discussion , 8181. Yun TJ, Coles JG, Konstantinov IE, Al-Radi OO, Wald RM, Guerra V, de Oliveira NC, Van Arsdell GS, Williams WG, Smallhorn J, Caldarone CA. Conventional and sutureless techniques for management of the pulmonary veins: Evolution of indications from postrepair pulmonary vein stenosis to primary pulmonary vein anomalies. J Thorac Cardiovasc Surg. 2005;129:167-74. ].
Personal perspective - Neil Wilson
Pulmonary vein stenosis is an extremely rare condition such that most interventionists will only manage a small number of cases during their careers. The rarity of the lesion precludes objective direct comparison of differing techniques because case series are small. As we mention in the text, the emergence of cutting balloons, stent angioplasty and drug-eluting stent use are symptoms of the progressive disease which one is dealing with in most cases. Despite the progression of this disease surgery is favoured initially by most institutions. Ultimately, therefore, catheter-based procedures are performed late on very sick infants. Over the last two decades we have moved from a more aggressive approach to a more balanced position as the hoped-for improvements have not been realised. Thorough multimodal diagnostic assessment is essential if we are to understand the nature of the condition. Timely angioplasty, usually on a repeated basis followed by close follow-up, is our procedure of choice. More aggressive approaches with stent placement are adopted when there is significant recoil of a lesion and the clinical situation affords no other option. These infants are often ventilator dependent and have severe pulmonary hypertension. This is a condition for which a national register of data may prove useful and dialogue with international colleagues of emerging techniques is likely to be of more use than review of the literature. Objectives need to be realistic with an overall aim of improving quality of life. Education and counselling of the parents should honestly reflect this.