Summary
This chapter gives an account of the history of coronary interventional cardiology. After the performance of coronary angiography and the first effective surgical myocardial revascularisation, the first coronary angioplasty performed by Andreas Gruentzig in September 1977 was the beginning of an extraordinary saga of techniques developed to repair stenosed vessels and to prevent acute complications and restenosis.
The chapter includes a complete description of the pioneering work of Andreas Gruentzig and addresses the history of subsequent innovative techniques such as the long guidewire or Monorail techniques, directional atherectomy, rotablator, ROTACS, cutting balloon, brachytherapy and therapeutic ultrasound. The development of coronary stents from the bare metal era to that of drug-eluting stents is also detailed. Additional diagnostic tools in the realm of coronary angioplasty are mentioned where pertinent.
Therapeutic applications of cardiac and vascular catheterisation were introduced in the late 1970s. Percutaneous coronary interventions have been the centrepiece of interventional cardiology. The story started in 1977 with the pioneering work of Andreas Gruentzig and was followed by an explosion of exciting and innovative techniques, some of which were successfully applied to other fields of cardiovascular medicine (valvular disease, arrhythmias, congenital heart disease, carotid and other peripheral vascular disease) as well as non-cardiovascular fields (gynaecology, gastroenterology, pneumology and urology).
In this chapter, we will consider only coronary interventional cardiology.
History of coronary balloon angioplasty
Dr Andreas Roland Gruentzig ( Figure 1 ) was born in Dresden, Germany, on June 25, 1939. His father got drafted during the Second World War as a geographer for the meteorological services of the Luftwaffe. He disappeared shortly before the end of the war. His mother, a musician and piano teacher, was left with two small sons to whom she dedicated the rest of her life. First, she emigrated with her children to Argentina where they had relatives (1950-2). After a short stay there, the family returned to Leipzig, East Germany. In 1957 they left East Germany for Heidelberg in West Germany ahead of the Wall going up. Rumour has it that the two gifted adolescent sons had been earmarked for manual work careers in the German Democratic Republic. Understandably, neither the mother nor the sons themselves agreed with this governmental verdict, one of the reasons for their emigration. Medical tutors on Gruentzig’s way to Zurich were Schettler and Schaefer in Heidelberg, West Germany, and Rose and Holland in London, United Kingdom. Robert Hegglin, the chief of the medical outpatient clinic (Medizinische Poliklinik) at the University Hospital of Zurich, Switzerland, attracted Gruentzig’s attention with his textbook “Differential Diagnosis in Internal Medicine”, one of the leading publications on the subject in German. Gruentzig had an interview for a job with Hegglin and was accepted. He started his training in Hegglin’s department on November 1, 1969, but Hegglin died just three weeks later on November 22 from a ruptured aortic aneurysm at the age of 62. Although they spent virtually no time together, this is an excellent example of one great man passing the torch on to another great man. Had it not been for Hegglin’s reputation, Gruentzig would not have joined the staff in Zurich. Instead of building up his interest in vascular disease in the newly founded angiology unit of Alfred Bollinger, one of the division heads in Hegglin’s department, he might have moved on to a different field, and no Gruentzig balloon would ever have been invented. Gruentzig’s interest in catheter-based therapy of vascular disease had been further fuelled during the time he spent at the Max-Ratschow-Klinik in Darmstadt, West Germany, in 1969.
Stimulated but also mentored by Bollinger, a pioneer in the discipline of angiology, Gruentzig became a fine clinician and a practically oriented clinical researcher. Angiology was the ideal foundation Gruentzig needed to develop first peripheral and then coronary angioplasty. The discipline angiology deals with peripheral vascular disease from prevention to diagnosis, pharmacological and, more recently, interventional therapy, just as cardiology does for heart disease. Angiology units were created in some European countries but angiology never reached widespread acceptance as a separate discipline as cardiology.
During his brief training period in radiology in 1971 and 1972, Gruentzig was allowed to travel to the famous Aggertalklinik in Engelskirchen, West Germany, to watch Eberhard Zeitler applying the Dotter method for percutaneous treatment of peripheral arteries. This method was flourishing in Germany much more than in its native country, the United States [11. Dotter C, Judkins M. Transluminal treatment of arteriosclerotic obstruction: description of a new technic and a preliminry report of its application. Circulation. 1964;3:654-670. ]. Again, the existence of angiology provided the optimal background. Although Gruentzig sensed that the idea of dilating stenoses by pushing telescope-like plastic tubes of increasing diameter through the narrowing could not be the ultimate solution, he was excited about offering a mechanical therapy to his patients. In December 1971, Zeitler gave a lecture in Lucerne, Switzerland, and Gruentzig urged him to drop by on the way home at the University Hospital of Zurich to help with a first local patient [22. Beck A, Gruentzig A. Eine Idee verändert die Medizin. Clio Verlag Konstanz, Germany 2000. ]. The procedure was carried out by Zeitler with Gruentzig assisting under the scrutiny of virtually all the senior radiologists. The local site of the stenosis in the superficial femoral artery was improved conspicuously. However, the patient started to have pain in his leg while he was still on the table and a complete occlusion of the popliteal artery by embolic debris was diagnosed.
Gruentzig was not the kind of person to give up after this. He continued to use the Dotter method on his own in a small series of patients which he followed up together with Maria Schlumpf, his personal assistant, in the meticulous way typical of both of them. Notwithstanding, he continued to look for a better technique. His initial experiments performed in 1971 with a stiff wire with a C-shaped tip which was rotated using a regular household drill worked in the animal model as an initial percutaneous atherectomy device but it was not pursued further. Gruentzig had been intrigued by the idea of Werner Porstmann in Berlin, East Germany, of using a caged latex balloon for dilatation of arteries. Again, Gruentzig intuitively knew that the direction was right but that there had to be a better way. Together with his wife Michaela, Maria Schlumpf and her husband Walter, he experimented with different materials. The breakthrough came with the involvement of Heinrich Hopff, a retired plastics expert from the Swiss Technical University Zurich just a stone’s-throw away from the University Hospital. He suggested polyvinyl chloride (PVC) to achieve a form-constant cylindrical balloon. Early in 1973 the group found further help in the person of a rubber expert by the name of Kienast from the local Maag rubber factory. He provided PVC for free. Following the suggestions of Hopff, they overdistended a segment of PVC tube thereby forming a fairly pressure-resistant cylindrical balloon. To produce a balloon catheter, Gruentzig pulled this tube over a plastic catheter and circumferentially glued both ends of the tube to the catheter. Before that, he had cut some side holes into the plastic catheter exactly where the overdistended segment of the PVC tube (the actual balloon) came to. For inflation and deflation of the balloon, Gruentzig inserted a wire with a distal cone into the plastic catheter. The cone occluded the distal end of the plastic catheter. Injecting fluid into the proximal end inflated the balloon and aspirating it led to deflation ( Figure 2 ). Most of this took place on the kitchen table of the apartment of the Gruentzig couple ( Figure 3 ). Initially, Andreas had assumed that a silk stocking would be required to prevent even a PVC balloon from turning into a spherical shape with increasing pressure. He had found a manufacturing plant in Niederlenz, Switzerland, producing such fabrics, and he had come across a person there by the name of Schaerer who provided advice as well as samples. However, it turned out that such a stocking was not required after all. This simplified the production of the preparedballoons significantly. Gruentzig recounts this development in his own typical way:
“I spent the next two years contacting manufacturing plants in an attempt to solve this problem. Especially fruitful was the cooperation of a factory that produced shoelaces and which provided me with silk meshes which I planned to wrap around the balloon, thus limiting its outer diameter. I then needed a very thin balloon to insert within the mesh. It was at that time that I met a retired chemist, Dr. Hopff, a professor emeritus of chemistry of the Technical University of Zurich. He introduced me to polyvinyl chloride compounds. I started to experiment with this material and studied his book on organic chemistry. I acquired some small thin polyvinyl chloride material used as insulation for electrical wires. Following the description in his book, I heated a localized segment of the tubing and applied compressed air pressure resulting in a localized aneurysm of the tubing. I used a second outer tubing measuring 4 mm in diameter to confine the diameter of the segment. After hundreds of experiments, most of which were performed in my own kitchen, I was able to form a sausage-shaped distensible segment which I tried to reinforce with the silk mesh. When I mounted the material on normal catheter tubing and applied pressure to distend the aneurysmal segment, I suddenly realised that the strength of this material was so great that the silk mesh was not necessary. This was a great break-through and enabled me to reduce the size of the catheter”.
This crude single-lumen balloon was used for clinical cases for over a year starting at the end of 1973. The first patient had a short occlusion of his femoral artery at the Hunter canal. There was no Internal Review Board at the time and Gruentzig presented the case to the chief of internal medicine, Walter Siegenthaler, who gave the go-ahead. The case was subsequently presented to an interdisciplinary board. The chief of general surgery expressed concern even in the face of a beautiful angiographic and clinical result. However, the chief of cardiac surgery, Ake Senning, a pioneer in his own right, came to Gruentzig’s support. Gruentzig recounts (courtesy of Maria Schlumpf):
“In spite of the fact that the patient’s artery was now patent, concern was expressed by the peripheral vascular surgeon over the existence of complications. The chief of surgery also expressed his concern. The chief of cardiac thoracic surgery, Dr. Senning, managed to modify the statement of his colleagues. After this rather difficult session, the chief of medicine, Dr. Siegenthaler, finally concluded that we should proceed with additional patients.”
Parallel to his clinical work with the single-lumen catheter, Gruentzig roamed the pertinent workshops and pestered experts for a technology to produce a double-lumen catheter. He got help from an employee of the Schneider Medintag Company by the name of Schmid. This company was later going to produce the Gruentzig coronary balloon catheters but, initially, Mr. Schmid was frowned upon by his superiors because of his collaboration with Gruentzig. He contributed the idea of carving a longitudinal channel into the outside surface of the plastic tube over which a second thin plastic tube was shrunk to create a second channel. To make separate use of both lumens, a y-connector had to be constructed for the outer end. This, again, was quite a struggle. None of the medical equipment manufacturers who were presented with this double-lumen catheter was interested in producing it industrially. Gruentzig was forced to construct the catheters laboriously himself with the help of Walter Schlumpf. Even the first prototype balloons used for coronary angioplasty in dogs were self-made. It was only in the middle of 1976 that the Cook Company and Schneider Medintag started to produce Gruentzig balloons. The peripheral balloons which Gruentzig and Schlumpf produced were not only used by Gruentzig himself but also shipped to colleagues who had started using the Gruentzig procedure. Such balloons went to Zeitler and other physicians in, e.g., Frankfurt, Munich, Heidelberg, Vienna, Amsterdam and New York.
In terms of his hospital career, Gruentzig had accepted the offer to work as a fellow in cardiology in October 1973, shortly before his first peripheral angioplasty with his balloon technique. On March 1, 1974, he was promoted to chief fellow, and on August 1, 1974, to senior cardiologist. Thus, his cardiology training took about 10 months, probably the shortest fellowship in cardiology ever. The chief of cardiology, Wilhelm Rutishauser, was quite enamoured with the drive and academic potential of the young doctor he had appointed. On the other hand, his deputy chief, Hans Peter Krayenbuehl, was utterly sceptical towards the mechanical approach Gruentzig applied to vascular disease. Unfortunately for Gruentzig, Rutishauser left Zurich for Geneva in April 1976 and Krayenbuehl took over.
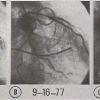
The first canine coronary angioplasty was performed on October 22, 1975, about two weeks after the cardiac surgeon Marko Turina had produced a coronary stenosis with a silk ligature. The heart was sent to the pathologists J. Schneider and J. Leu who advised strongly against continuing the experiments based on what they saw. Gruentzig knew better from his clinical experience with peripheral angioplasty already amounting to several hundred patients. By 1976, dog experiments with coronary angioplasty were already far advanced and the method was ready for clinical use. A coronary double-lumen catheter had been produced by Schneider Medintag and was waiting for the first client ( Figure 4 ).
It has not been widely publicised that the first attempt at coronary angioplasty in a catheterisation laboratory preceded intraoperative coronary angioplasty by more than a year and the first case of percutaneous coronary angioplasty which was actually performed by a year and six months. On March 22, 1976, a 63-year-old man was referred to Gruentzig after having been cared for in the coronary intensive care unit for over two weeks without achieving relief of unstable angina complicated by recurrent infarctions. A cardiac catheterisation had revealed severe triple vessel disease, including a stenosis of the left main stem, and the patient had been turned down by the cardiac surgeons due to his poor surgical bypass targets and poor general health.
Gruentzig had hesitated because the case in no way represented what he had envisaged for his first coronary patient. The patient consented to having the new procedure tried out on him, cognizant of his desperate situation. Due to abdominal aortic disease it was not possible to insert the guiding catheter from the groin. Access was gained from the left brachial artery but the coronary ostium could not be found with the bulky guiding catheter (about 10 Fr). The procedure was abandoned without a balloon catheter ever being inserted into the coronary artery. The patient died two days later from acute myocardial infarction, the third he had suffered in three weeks (personal communication: Peter C. Baumann). Gruentzig’s recollection of the case has been published [33. King III S. Angioplasty from bench to bedside to bench Circulation. 1996;93(1621-1629). ]:
“The first patient on whom we attempted dilatation was a case in which coronary vascular surgery was denied. The patient with unstable angina, multivessel disease, main stem stenosis, referred to the coronary care unit, was presented to me and everyone assured me that attempted dilatation with success would be the proof for the efficacy of this method. I agreed, eager to enter the era of competition with the surgeons. Unfortunately, the patient was so diseased that every attempt to puncture the groin artery failed because of total closures: only the left brachial artery had positive flow to allow the passage of the catheter to the aorta. With this entrance, the catheters were unable to guide the coronary dilatation catheter to the orifice of the left main so that we had to abandon the procedure. The patient died several days after the procedure of a final myocardial infarction. The case taught me that if you start a method, you should start with an ideal case and not with end-stage disease, and this had been the truth for so many other colleagues in a similar position later in time.”
About a year later, on May 9, 1977, clinical coronary balloon angioplasty became a reality with a total of four cases of intraoperative procedures being carried out during open heart surgery by the team of Elias Hanna, cardiac surgeon, Richard K. Myler, cardiologist and Andreas Gruentzig in San Francisco, USA. These cases were successful, or at least uneventful, as the dilated lesions were simultaneously bypassed. The invitation to perform intraoperative angioplasty had emanated from Gruentzig’s presentation of the dog experiments during the annual convention of the American Heart Association in Miami [44. Gruentzig A, Turina M, Schneider J. Experimental percutaneous dilatation of coronary artery stenosis (abstract). Circulation. 1976;53:II-81. ], USA, in November 1976. There he had caught the attention of Myler, a person henceforth instrumental in the further development of clinical coronary angioplasty. Gruentzig returned to Zurich invigorated and continued to look out for a first ideal percutaneous case.
Today it sounds odd that no suitable patient could be found for months. Several factors were involved. First, the attitude towards balloon angioplasty turned from fairly lenient where peripheral arteries were concerned to blatantly hostile when coronary arteries became the target. The cardiac surgeons, exclusively privileged to work in these delicate structures at the time, were not the primary foes. It was the internists who looked upon someone embarking on bloody interventions in the sacred centre of the human body as a frivolous heretic about to lose his mind. Secondly, coronary artery disease in that era was not worked up invasively until its late stage. A coronary angiogram showing a single lesion was an exquisite rarity at the time and almost considered a mistake in the indication for the coronary angiogram.
Gruentzig spent the first two weeks of September 1977 back in San Francisco, USA, to find a suitable patient there. Interestingly, even in this more aggressive environment, and in the busy practice of Myler, no candidate was found. Frustrated, Gruentzig returned home. This is when Bernhard Meier presented to him a 38-year-old patient who had been transferred from a peripheral hospital because of several weeks of unstable angina. He had undergone coronary angiography on September 14, 1977, and a single discrete lesion in the proximal left anterior descending coronary artery had been documented. Gruentzig offered the patient the chance to become the first human being to undergo coronary balloon angioplasty. The patient shared the room with people recovering from coronary bypass surgery, and had already been informed by the doctor performing his coronary angiogram that surgery was going to be necessary for him as well. Therefore, the the option of an alternative to bypass surgery was quite appealing to him.
The plan to intervene was first approved by Senning, the senior cardiac surgeon, and subsequently by Siegenthaler, Gruentzig’s ultimate medical chief. As the physician responsible for the patient, Meier accompanied him to the catheterisation laboratory. The case was performed in a quiet atmosphere. Gruentzig was more tense than usual only to the eyes of people who knew him well. The patient, who was awake, apparently had full faith in his doctor. People were walking in and out, the faces of the surgeons somewhere between stern and bemused, their minds behind the facade no doubt a bit worried.
The patient reminisces on the intervention as follows:
“I had been transferred to the University Hospital of Zurich from the Kantonsspital Baden because of severe chest pain that had caught me while fishing in the Limmat river early one morning. Although the pain had subsided and no infarction had been found, the pain recurred several times at rest and a stress test on a bicycle apparently showed dramatic changes in my electrocardiogram. On the evening of September 15, 1977 Andreas Gruentzig, a young doctor about my age, explained to me his new method to treat narrowed heart vessels such as the one they had documented in my heart. I immediately fell for the balloon method and for the charisma of Dr. Gruentzig whom I trusted immensely. I did not hesitate to consent to become a guinea pig, even more so because Dr. Gruentzig guaranteed that a surgical team would be on stand-by in case complications occurred. My roommates recovering from bypass surgery warned me about being overly optimistic and predicted that I would come back with a scar on my chest just as they had. The next day in the catheterisation laboratory, the atmosphere was quite calm. My groin was numbed and I could personally watch the catheter finding its way to my heart. Dr. Gruentzig showed me the narrowing before he inserted the balloon catheter and removed it. I felt no pain. In the faces of Dr. Gruentzig and other doctors in the laboratory I could see the success of my intervention reflected. My roommates appeared quite jealous when I returned without the scar and was able to move around normally the next day without any pain.”
The patient found himself back on the bicycle ergometer two days after the procedure. Interestingly, this test was still positive electrocardiographically with some ST elevation, albeit markedly improved compared to the pre-intervention test. The thallium perfusion test also showed some residual reversible ischaemia. At that time, this was thought to be part of the recuperation process. Little did Andreas Gruentzig know that this was rather exceptional and in a way worrisome after angioplasty of a single discrete lesion.
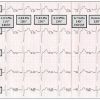
During this first case, the roller pump which had kept the dogs alive during prolonged balloon inflations in the animal experiments stood by, ready to be brought into action if required. It was not going to be used in this case or in any subsequent case as the short occlusion of the coronary artery was well tolerated. Only years later was the pump used for a short period of time as a temporary perfusion device in abrupt vessel closure during coronary angioplasty when arterial blood harvested from a femoral artery was reinjected into the distal coronary artery beyond the occlusion. Today the roller pump is one among many specimens in the museum of coronary angioplasty. In this exceptional case, poor fluoroscopy, overzealous advice from peers and the ease of the intervention, which surprised even the inventor, led to an additional dilatation of the take-off of a diagonal branch, not in need of any treatment. The patient had a short period of right bundle branch block (later to be recognised as an extremely rare complication of balloon angioplasty), but otherwise his course was uneventful. The case was thoroughly documented in terms of pressure curves ( Figure 5 ). However, the angioplasty film has disappeared and so has the written report. The only written report preserved is the discharge summary written by Meier. Gruentzig appears on this letter only as a recipient of a copy
Gruentzig’s recollection of the first case performed was published by J. Willis Hurst in 1986 [55. Hurst J. The first coronary angiopsty as described by Andreas Gruentzig. Am J Cardiol. 1986;57:185-186. ]. He had planned to withhold this case from the media until more cases with some follow-up had been accumulated. However, the patient informed a journalist. Gruentzig convinced the media to wait for a few months before making this procedure public. The news finally hit the front page of a daily newspaper in Zurich in February 1978.
A follow-up angiogram was performed one month after the procedure and showed a perfect result [66. Gruentzig A. Results from coronary angioplasty and its implications for the future. Am Heart. J 1982;103:779-783. ] ( Figure 6 ). It was presented together with the results of the first four patients at the annual convention of the American Heart Association in November 1977. The picture of the fourth uppatient in particular triggered an interruption by spontaneous ovation during Gruentzig’s presentation. It showed a tight left main stem stenosis completely removed by balloon angioplasty. The case had been performed in Frankfurt, West Germany, with the assistance of Martin Kaltenbach. Unfortunately, this particular patient (a 43-year-old man) had recurrent symptoms only one month after his successful intervention. A follow-up angiogram showed a restenosis of 40% and no re-intervention was carried out. In spite of the diagnosis of vasospastic angina, the treating physician continued with beta-blockers. A few weeks later the patient had an anterior myocardial infarction and had to be resuscitated at home. He died in February 1978 from the consequences of this event. At autopsy, all his coronary arteries including the left main stem were patent and there was no detectable damage to the arterial wall of the left main stem (personal communication: Martin Kaltenbach). This patient was the reason for striking left main stem disease off the indication list of coronary angioplasty for quite a while.
Gruentzig’s second case contributed to this early change of policy. It had been performed in Frankfurt, West Germany, again with Martin Kaltenbach, and also involved a left main stem stenosis. In this case the lesion was barely improved. Although a lesion of the right coronary artery was simultaneously dilated (make no mistake, the second coronary angioplasty in the world consisted of left main and simultaneous right coronary artery dilatation!) and the patient was clinically improved, he was not symptom-free and underwent bypass surgery during the summer of 1978. He had an uneventful course. At the 20-year anniversary of percutaneous transluminal coronary angioplasty (PTCA) he had a follow-up angiogram in Rothenburg, West Germany. The third patient had been a patient in Zurich and in this case again double vessel disease was treated simultaneously with success. It was not until the seventh patient that a significant complication occurred and emergency coronary artery bypass surgery had to be carried out. It was performed by Turina, and the outcome was good. The cases of the first five patients were published in the Lancet [77. Gruntzig A. Transluminal dilatation of coronary-artery stenosis. Lancet. 1978; 1:263. ] and the initial series of 50 patients in the New England Journal of Medicine [88. Gruntzig AR, Senning A, Siegenthaler WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. N Engl J Med. 1979;301:61-68. ].
The first patient became a personal friend to Andreas Gruentzig, Maria Schlumpf and Bernhard Meier. Subsequently, he participated as a popular delegate in a number of the live teaching courses on PTCA. The four such courses held in Zurich before Gruentzig left for Emory University in Atlanta, USA, gave rise to an avalanche of similar live courses which continue to the present day. The programme of the first live course extended over 4 days and featured 5 coronary angioplasties (one of a bypass graft), 2 femoral angioplasties, and 1 renal angioplasty. The last live course in Zurich brought together the “who’s who” of interventional cardiovascular specialists amounting to 212 people at the time. It provided the rare opportunity to have four giants of invasive cardiovascular medicine (Dotter, Gruentzig, Judkins and Sones) under one roof. Unfortunately, all of them died about 5 years later in what was, for this specialty, the gloomy year of 1985.
During the first years of coronary angioplasty the live courses served the additional purpose of licensing. Only doctors who had attended such a course were entitled to buy angioplasty balloons. With a prized certificate of Gruentzig, they had to find the Schneider Company located in the basement of an old house in Zurich and pay cash in Swiss francs for the material.
Coronary angioplasty appeared to be a small step for Gruentzig but it turned out to be a huge step for mankind. It had transformed the first patient from a seriously ill man to a healthy one within minutes, this for 35 years and counting. Even more importantly and in contrast to the first landing on the moon 8 years earlier, it has had a lasting impact on the wellbeing of mankind. It transformed cardiology from an investigational, drug-oriented discipline to a hybrid between internal medicine and surgery. Interventional cardiology emerged to become the leading medical specialty performing the highest number of important interventions and making cardiology a mature and comprehensive specialty efficiently dealing with western society’s most important curse, coronary artery disease. Moreover, Gruentzig’s coronary angioplasty paved the way for other nonsurgical interventions such as electrophysiology, carotid angioplasty, gastrointestinal catheter procedures, and so forth.
Unfortunately, he did not live to take the credit for it. Gruentzig died in a plane crash piloting his twin-engine Zeneca back from a weekend at Hilton Head Island to Atlanta through bad weather. It was October 27, 1985, and he was in a rush to be at the hospital in time to continue his important clinical work on Monday morning. His wealth had grown commensurately with his reputation and so had the size of his planes, from the small Piper and, later, Cessna he had started with in Zurich. His PTCA technique, however, had taken off for good, and an untimely end, although predicted by many, was never a real threat.
While Gruentzig was in favour of extending the procedure to uncharted territories such as the renal arteries, he himself shied away from attempting carotid angioplasty. Meier presented him with what appeared to be an ideal case in 1978 but he turned down the patient. He argued that surgical carotid endarterectomy was not comparable to cardiac surgery as the problem lay right underneath the skin. The chest did not have to be cracked open and the heart did not have to be stopped and replaced temporarily by a machine. He also argued that a complication in the brain would mark a patient for life and would remind the patient every minute of the failed intervention. By contrast, a cardiac complication rarely led to intractable symptoms if the patient lived beyond it. Although carotid angioplasty has since found a large community of supporters, it will never reach the uncontested and coveted role coronary angioplasty eventually came to enjoy.
The world’s first coronary angioplasty patient had a marvellous further course. He quit smoking and, shortly after his one-month angiogram [66. Gruentzig A. Results from coronary angioplasty and its implications for the future. Am Heart. J 1982;103:779-783. ] showing a pristine result, he also quit all medications. On the occasion of the ten-year anniversary he underwent a follow-up coronary angiogram by Spencer B. King III at a live course in Atlanta, USA. It showed essentially normal coronary arteries. On the 20-year anniversary he underwent a live exercise test on Swiss prime-time television ( Figure 7 ) and an angiogram by magnetic resonance. Again, no sign of restenosis or new disease was found. Nevertheless, he was convinced to start taking acetylsalicylic acid and simvastatin for secondary prevention. In 2000, 23 years after the intervention, he experienced a couple of episodes of chest pain early in the morning while at rest. The exercise test was normal ( Figure 8 ). An angiogram was performed on April 10, 2000, showing an excellent long-term result at the dilated site but a nonsignificant narrowing in the left anterior descending coronary artery proximal to it. The fractional flow reserve in that vessel was preserved (0.83) ( Figure 9 ).
Initially he agreed to conservative treatment. Yet, a few months later, he returned for angioplasty, because the pain had reoccurred in the small hours of the morning a couple of times. He had a hard time understanding why he should have to live with that, remembering his excellent experience with coronary angioplasty 23 years earlier. After a balloon dilatation, he was not pleased with the appearance of the lesion and convinced Meier that a stent needed to be placed ( Figure 9 ). Drug-eluting stents had yet to be introduced into clinical medicine at that time.
About six weeks later, the patient started to have severe exertional angina. Notably, he had never ever had exertional angina before. The follow-up angiogram on December 7, 2000, showed a severe in-stent restenosis which was re-dilated with a balloon ( Figure 10 ). The exertional angina immediately disappeared and currently is no longer present, some 12 years later.
This fantastic story requires a few comments: Gruentzig’s official first coronary angioplasty case (discounting the aborted attempt in 1976) was in many ways atypical. Then again it represents a fantastic example of what the method is capable of. The patient clearly had superimposed spasm, as his symptoms only occurred at rest. During the pre-intervention exercise test he had ST elevation and ventricular tachycardia but no chest pain. This is a rare finding in coronary artery disease. The fact that the stenosis showed up identically on two coronary angiograms two days apart (the diagnostic study on September 14, 1977, and the angioplasty on September 16, 1977) proves that the lesion was not simply a spasm. In spite of the fact that the radiologist who reported on both the diagnostic study and the angioplasty procedure had described diffuse disease and many stenoses, the coronary tree of the patient looked clean except for the one discrete stenosis. It continued to do so for decades. It is of note that Andreas Gruentzig was not allowed to write his reports himself at the time, and that the reports of the two historic catheterisations written by radiologists not present at the interventions have been lost. They can be reconstructed from the hospital discharge letter, the only pertinent written document of the case preserved. Both the diagnostic 35 mm cine film and the film of the procedure itself have disappeared. Only photographs of the left coronary angiograms have been preserved in the literature and on slides.
The patient did not observe any of the paradigms of secondary prevention so dear to us today except that he quit smoking. Nevertheless, he had an excellent clinical course until 23 years later, when he experienced the same type of symptoms at rest which had prompted his initial exploration. This time only a nonsignificant lesion in the vicinity of the initial site was discovered and the symptoms were considered either spastic or non-coronary [99. Meier B. The first patient to undergo coronary angioplasty: 23-year follow-up. N Engl J Med. 2001;344:144-145. ]. While the patient was at first content with knowing that there was no significant disease in his coronary arteries, he insisted on an intervention when early morning rest pain reoccurred several times over the subsequent months. He then also requested a stent when the initial angioplasty result was suboptimal. This happened about ten months before the first drug-eluting stent was available, and he suffered an in-stent restenosis of the worst kind only a few weeks after the intervention. Fortunately, a simple balloon re-dilatation solved the problem. Understandably, his second coronary problem appeared to him to be dealt with in a more complicated and less efficient way than his first some 20 years before. Hence, when he had his second contact with the method as a patient, the tremendous evolution of the procedure which he had pioneered together with his doctor, Andreas Gruentzig, was hardly apparent to him.
It is safe to say that the procedure has not only helped millions of people but probably also saved numerous lives (the ones when patients with acute myocardial infarction were rescued, and the ones which would have been lost to a possible infarction avoided thanks to timely treatment of a lesion). It fostered many a career, created a gargantuan industry, and constituted an iterative topic of a significant percentage of the medical literature. The media repeatedly deal with it and even lay literature about this topic abounds. Had Andreas Gruentzig only been able to witness the ever-growing impact of his procedure on mankind, giving not only help but also jobs, prestige, satisfaction and a reason to live to countless people, how pleased he would have been. He might even have been consoled by the fact that, in spite of being suggested for the Nobel prize in 1978 together with Melvin Judkins and Mason Sones by Dr. Foley, he was never nominated. His plane crash in 1985 killed that dream with him. On the other hand, it imprinted him indelibly in our memories as an ever young, good-looking, charismatic and sociable giant in medicine. Maybe it spared him two disappointments in his life other, that is, than being ignored by the Nobel committee, namely the fact that outdoing his prodigious invention of coronary angioplasty was virtually impossible and that the traditional German universities just did not seem to be ready to appoint him to a prestigious chairmanship. While he was undoubtedly one of the most important European physicians of all time, the old continent hesitated on a top-level job offer until it was too late, much in contrast to the new continent.
With some exceptions, European peers and particularly superiors had not been kind towards Andreas Gruentzig. In a strictly hierarchical organisation reigning in the typical traditional European university hospital, a person casting a large and long shadow is not welcome. Andreas Gruentzig was clearly discriminated against when it came to promotions in Zurich. He had the smallest office among colleagues his age, had to pay for secretarial help for all correspondence pertaining to coronary angioplasty from private sources, and was rarely praised for successes but regularly reprimanded for “unsuccesses”. His patient allotment was rationed to less than one slot a day. No wonder that the welcoming attitude of the United States to success, and the generous offers from many an American university, such as Stanford or Harvard, or institutions such as Cleveland Clinic, were attractive to Gruentzig. He resisted the temptation for a long time and continued to apply for positions at West German universities. However, when he was turned down time and time again, and when Emory University in Atlanta, USA, offered a high position in an active cardiovascular unit with a full professorship and a new, completely staffed catheterisation laboratory accompanied by sufficient bed capacity (Coca Cola Company being the sponsor behind this), he accepted. He pushed aside reservations about the English language and American culture, engraved into his mind during his education in East Germany. He invested considerable time in motivating his wife to accompany him and he offered one last chance to the University Hospital of Zurich to improve his situation. How the story continued is well-known and, perhaps, the way it had to be.
Development of balloon angioplasty after the first procedure
From 1977 to 1981, coronary angioplasty was recommended for very select cases: the patients should be symptomatic, with stable angina and good left ventricular function. They also had to be candidates for coronary artery bypass surgery. Andreas Gruentzig himself stated in a meeting that the technique should be limited to a small number of patients presenting with the above-mentioned characteristics. Among the major reasons for these limitations were the balloon catheter characteristics. There was a very small fixed guidewire at the tip of the balloon precluding torquing it after the balloon had been introduced into the coronary artery ( Figure 4). The deflated size (1.5 to 2.0 mm) and the stiffness of the balloon did not allow tight lesions or acute curvatures to be passed, and it was only possible to push it through straight coronary segments, mainly in the proximal left anterior descending coronary artery and the first segment of the right coronary artery. In addition, the guiding catheters (9 Fr) had a very thick wall and a relatively small lumen: because of the space-occupying bulky balloon shaft it was difficult to inject contrast medium and to ascertain the position of the balloon inside the vessel. This required the connection to a pressure gauge for distal pressure measurement to assess the result haemodynamically. Fluoroscopy was poor and not usable for this. While cine runs could be replayed from video recorders the size of a truck, crisp still frames were not available. The processing of the 35 mm cine film to use its good resolution in the middle of the procedure was too time-consuming.
A major step forward was achieved when John Simpson proposed the removable guidewire which subsequently allowed torque control, giving it the name steerable guidewire ( Figure 11 ).
John Simpson had applied the Seldinger technique used for years in catheterisation and notably also Gruentzig’s angioplasty of peripheral vessels to the coronary artery tree. The guidewire had a solid core which was tapered toward the distal end to increase flexibility. The tapered distal end of the core wire was surrounded by a coil spring which was made from radiopaque material. An attachable handle (torque) for manoeuvring the guidewire was also proposed.
The balloon catheter included a lumen accepting a 0.018 inch (0.46 mm) Teflon-coated flexible-tipped guidewire. The independently movable guidewire greatly facilitated the negotiation of the vessel but measurement of distal pressures became more complicated.
After testing in animal and cadaver hearts, Simpson reported in 1982 the first human experiences with the new catheter system [1010. Simpson JB, Baim DS, Robert EW, Harrison DC. A new catheter system for coronary angioplasty. Am J Cardiol. 1982;49:1216-1222. ]: he performed angioplasty in 53 patients with single vessel disease and the success rate was 64 per cent. Using a smaller balloon in the last 41 cases, he was able to increase the success rate to 73 per cent.
The major advantage was the easier navigation of the vessel to be treated, since it was possible to withdraw and to reshape the guidewire and also to avoid the risk of dissection by pushing the balloon in a guided fashion (on a track) through an atherosclerotic plaque.
The invention of the steerable guidewire and the over-the-wire coaxial technique led to the founding of Advanced Cardiovascular Systems (ACS) in 1978. Technological refinements improved these guidewires rapidly. They became available in different diameters (from 0.010 to 0.018 inch, 0.25 to 0.46 mm). Radio-opacity was improved by inclusion of titanium or platinum. The friction was reduced by Teflon coating. The tips were shapeable with good residual memory. Gruentzig’s group presented their steerable system in parallel [1111. Gruentzig AR, Meier B. Current Status of dilatation catheters and guiding systems. Am J Cardiol. 1984; 53.92c-93c. ].
A short-lived revival of the fixed wire balloon was witnessed with the Medtronic Omniflex system ( Figure 12 ) proposed by Maurice Buchbinder. It featured a system able to deflect the tip by an external handle: in this way the tip of the wire and the balloon could be pointed toward the target lumen and adapted to the anatomy. The stiffness of the device was also considered an advantage to cross chronic total occlusions [1212. Hamm CW, Kupper W, Kuck KH, Hofmann D, Bleifeld W. Recanalization of chronic, totally occluded coronary arteries by new angioplasty systems. Am J Cardiol. 1990; 66:1459-1463. ].
Even with steerable guidewires, a problem remained. Passage of a very tight stenosis implied a small balloon (2.0 mm), but to optimise the results a bigger balloon (3.0 or 3.5 mm) was required. In the early stages, it was necessary to remove not only the balloon catheter but also the guidewire. The next tedious step was to pass again through the stenosis disrupted by the first balloon inflation. In some cases, this new passage was impossible or led to a dissection because during the second approach the guidewire passed underneath the plaque. The standard length of guidewires was 175 cm; to exchange the balloon catheter whilst the wire was still in place required a longer guidewire (approximately 300 cm). To overcome that issue, the first solution was to extend the guidewire. Special devices to connect a standard coronary guidewire to an extension were developed.
The connection between the two parts of the guidewire were, however, not very solid and in a number of cases the removal of the initial balloon was followed by the inadvertent removal of the distal part of the guidewire proximal to the lesion or by the disconnection of the two parts of the small wire. In these cases, all the benefit of an initially intricate procedure was lost with, in some cases, occlusive dissection of the vessel requiring emergency bypass surgery.
An alternative to the extension was the long guidewire technique described by Kaltenbach [1313. Kaltenbach M. The long wire technique--a new technique for steerable balloon catheter dilatation of coronary artery stenoses. Eur Heart J 1984; 5:1004-1009. ]. After the insertion of a guiding catheter into the ostium of the obstructed coronary artery the stenosis was crossed with a special guidewire (Schneider Medintag, Zurich, Switzerland) of 3 m length. The guidewire was equipped with a ball-shaped tip to make the tip less traumatic to the vessel wall during the unavoidable pulling and pushing motions during a balloon exchange.
This wire could be introduced without a balloon catheter so that, during the process of passing the stenosis, unhindered contrast medium injections were possible. This facilitated display of the exact localisation of the wire tip and of anatomical details within the coronary artery. Advancing and rotating of the wire occurred reliably and without friction. Likewise, possible impediments of the wire tip were better felt proximally. Abrupt vessel closure during probing became a rare event. If it happened after balloon expansion it could be handled by recrossing the lesion over the wire remaining in place. This contributed to a significant fall in need for emergency operations from about 5% to 1% in the hands of the inventor.
The next major advance was the Monorail system proposed by Bonzel [1414. Bonzel T, Wollschläger H, Just H. A new catheter system for the mechanical dilatation of coronary stenoses with exchangeable intracoronary catheters, fast flow of the contrast agent and improved control. Biomed Tech (Berl). 1986;31:195-200. ]. A guidewire with a length of about 3 m to exchange a balloon was necessary because the end of a normal wire (about 170 cm long) disappeared into the shaft of the balloon catheter before the latter was fully retracted out of the body. The solution was not to extend or replace the wire but to modify the catheter shaft in such a way that the wire could still be held in the hand while the catheter was being fully retracted. For this purpose, the shaft would no longer envelope the wire coaxially but would release the wire through a side hole proximal to the balloon and run in parallel to the balloon shaft ( Figure 13 ).
Bonzel termed his balloon wire system a sliding rail system [1414. Bonzel T, Wollschläger H, Just H. A new catheter system for the mechanical dilatation of coronary stenoses with exchangeable intracoronary catheters, fast flow of the contrast agent and improved control. Biomed Tech (Berl). 1986;31:195-200. ]. Later, the term "Monorail" was coined by Meier, inspired by monorail trains with carriages running astride of, or suspended from, one rail ( Figure 14 ).
The alteration in the construction of the catheter brought major changes to the procedure. The guidewire and the balloon catheter were now introduced separately. There were appreciable advantages in first advancing the standard-length guidewire and navigating across the stenosis. It could be moved swiftly with little friction within the large-diameter guiding catheter. It also left ample space for injections of contrast medium and, when it got through after passing the stenosis, it could easily be retracted, given a new curve, or exchanged. When the tip of the wire had passed the stenosis, the Monorail catheter was loaded on to the proximal end of the wire from where it slid through the body of the patient into the coronary artery and into the stenosis.
In a similar way, the balloon catheter could be retrieved again and exchanged for a new one. The guidewire could be manually controlled all the time during the advancement, retraction and exchange of the balloon catheters. The tip of the guiding catheter could also be kept in place securely at the ostium of the coronary artery. The only function of the shaft of the balloon catheter was to advance and to retract as well as to fill and empty the balloon via a small hollow space inside. The cross-section of the shaft was reduced. More space was left in the guide catheter so that injection of contrast medium was facilitated and the imaging of the stenosis was improved even with the balloon in the coronary artery. Miniaturisation of the systems brought about huge progress. Standard guide catheters have been reduced in size from 9 Fr to 6 Fr or even 5 Fr in the meantime, which corresponds to a reduction of the cross-section by about 70%.
The conventional coaxial over-the-wire principle was abandoned in most European centres quite quickly.
The new devices
By the mid 1980s, new technological advances such as steerable guidewires or Monorail catheters had made angioplasty easier and more successful. While the number of procedures rapidly increased, restenosis was becoming a crucial issue. Some interventional cardiologists even used to repeat coronary angiography systematically at 6 months to screen for restenosis. That event appeared to occur in about 30% to 40% of cases. While it was fairly simple and safe to do repeat angioplasty, the high restenosis rate was a downside and stimulated research to prevent or limit the neointimal proliferation, considered to be the main mechanism of restenosis. Numerous clinical trials were launched to identify the “magic bullet” against restenosis: more than 70 clinical trials were conducted using various drugs (conventional or new) in more than 50,000 patients. Meanwhile, several interventional cardiologists, engineers and companies thought that the solution might emerge from new tools other than the balloon (which stretched the vessel, disrupted the plaque, and favoured the neointimal proliferation) rather than from drugs.
Engineers and interventional cardiologists proposed and tested a long list of devices and various different sources of energy were proposed to treat atherosclerotic plaque with a view to decreasing the risk of restenosis significantly. The era of “new devices” was ushered in.
DIRECTIONAL ATHERECTOMY
Directional atherectomy (DCA) was one of the first of the “new devices”. The concept was introduced by Simpson in 1985. The first atherectomy was performed in 1985 in a superficial femoral artery [1515. Simpson J, Johnson D, HV T. Transluminal atherectom: A new approach to the treatment of atherosclerotic vascular disease. Circulation. 1985;72:111. ]. This initial experience led the FDA to approve the device for peripheral vessel disease in 1987. Three years later, DCA was approved by the FDA as the first non-balloon percutaneous coronary interventional device. DCA is an over-the-wire cutting and retrieval system ( Figure 15 ). The Flexicut device was developed by the DVI Company created by J. Simpson. Johnson [1616. Johnson DE. Directional peripheral atherectomy: histopathologic aspects of a new interventional technique. J Vasc Interv Radiol. 1990;1:29-33. , 1717. Johnson DE, Braden L, Simpson JB. Mechanism of directed transluminal atherectomy. Am J Cardiol. 1990;65:389-391. ] showed that the device was able to remove important pieces of atherosclerotic material and to achieve a marked enlargement of the lumen. Nevertheless, numerous reports suggested that the main effect was due to a “Dotter effect”, i.e., a mechanical dilatation of the vessel with possible recoil and decrease of the initial beneficial effects.
Initially, Simpson’s atherectomy device was bulky ( Figure 15 ) requiring large guiding catheters (11 Fr). Later, the miniaturisation of the device and thinner wall guiding catheters allowed the use of 9.5 Fr guiding catheters.
In spite of a number of complications (abrupt closure [33. King III S. Angioplasty from bench to bedside to bench Circulation. 1996;93(1621-1629). , 44. Gruentzig A, Turina M, Schneider J. Experimental percutaneous dilatation of coronary artery stenosis (abstract). Circulation. 1976;53:II-81. , 55. Hurst J. The first coronary angiopsty as described by Andreas Gruentzig. Am J Cardiol. 1986;57:185-186. ], distal embolisation, myocardial infarction (6%-17%), perforations (~1%), the device became quite popular, particularly in North America. Several clinical trials (CAVEAT-I [1818. Topol EJ, Leya F, Pinkerton CA, Whitlow PL, Hofling B, Simonton CA, Masden RR, Serruys PW, Leon MB, Williams DO, King SB, Mark DB,Isner JM, Holmes DR, Ellis SG, Lee KL, Keeler GP, Berdan LG, Hinohara T, Califf RM. A comparison of directional atherectomy with coronary angioplasty in patients with coronary artery disease. The CAVEAT Study Group. N Engl J Med. 1993;329:221-227. ], CCAT [1919. Adelman AG, Cohen EA, Kimball BP, Bonan R, Ricci DR, Webb JG, Laramee L, Barbeau G, Traboulsi M, Corbett BN, Schwartz L, Logan AG. A comparison of directional atherectomy with balloon angioplasty for lesions of the left anterior descending coronary artery. N Engl J Med. 1993;329:228-233. ], CAVEAT-II [2020. Holmes DR, Jr., Topol EJ, Califf RM, Berdan LG, Leya F, Berger PB, Whitlow PL, Safian RD, Adelman AG, Kellett MA, Jr., Talley JD, Shani J, Gottlieb RS, Pinkerton CA, Lee KL, Keeler GP, Ellis SG. A multicenter, randomized trial of coronary angioplasty versus directional atherectomy for patients with saphenous vein bypass graft lesions. CAVEAT-II Investigators. Circulation. 1995;91:1966-1974. ]), however, failed to show a clear advantage in terms of restenosis rate reduction when cathetercompared with balloon angioplasty. Optimal atherectomy trials (OARS [2121. Simonton CA, Leon MB, Baim DS, Hinohara T, Kent KM, Bersin RM, Wilson BH, Mintz GS, Fitzgerald PJ, Yock PG, Popma JJ, Ho KK, Cutlip DE, Senerchia C, Kuntz RE. 'Optimal' directional coronary atherectomy: final results of the Optimal Atherectomy Restenosis Study (OARS). Circulation. 1998;97:332-339. ], BOAT [2222. Baim DS, Cutlip DE, Sharma SK, Ho KK, Fortuna R, Schreiber TL, Feldman RL, Shani J, Senerchia C, Zhang Y, Lansky AJ, Popma JJ, Kuntz RE. Final results of the Balloon vs Optimal Atherectomy Trial (BOAT). Circulation. 1998;97:322-331. ], START [2323. Tsuchikane E, Sumitsuji S, Awata N, Nakamura T, Kobayashi T, Izumi M, Otsuji S, Tateyama H, Sakurai M. Final results of the STent versus directional coronary Atherectomy Randomized Trial (START). J Am Coll Cardiol. 1999;34:1050-1057. ]) showed a small improvement but the rate of restenosis (16%-29%) was judged to be higher than that with stent implantation which was being investigated in parallel.
TRANSLUMINAL EXTRACTION ATHERECTOMY
The transluminal extraction atherectomy catheter (TEC) was designed by Stack [2424. Sketch MH, Jr., Phillips HR, Lee MM, Stack RS. Coronary transluminal extraction-endarterectomy. J Invasive Cardiol. 1991;3:13-18. ]. The concept of this device was based upon cutting and aspiration of atheroma and debris. The transluminal extraction catheter (TEC) is a torque-controlled catheter that incorporates an aspiration device into a distal rotational cutter ( Figure 16 ).
The device is an over-the-wire system including a conical extremity with two stainless steel blades attached at the end of a hollow torque tube. At the proximal extremity of the catheter there is a motor-driven unit connected to a vacuum reservoir to store excised atheroma and debris. After experimental studies in normal animal segments and in atherosclerotic cadaver arteries, the TEC was used in peripheral vessels and later in native coronary arteries and saphenous vein grafts. The device was approved by the FDA in 1989 for peripheral vascular disease, and for revascularisation of saphenous vein grafts in 1992. The device was also used in acute myocardial infarction because of its ability to remove fresh thrombus. Soon, use of the device was reduced to the treatment of complex, fragile, friable lesions of venous conduits. Several papers reported the results obtained with the TEC [2525. Popma JJ, Leon MB, Mintz GS, Kent KM, Satler LF, Garrand TJ, Pichard AD. Results of coronary angioplasty using the transluminal extraction catheter. Am J Cardiol. 1992;70:1526-1532. ]. With the increasing number of stent implantations, the TEC became obsolete.
THE KENSEY CATHETER
The Kensey catheter, a high-speed rotational recanalisation device, was used in 110 patients in a multicentre trial. Technical success was reported in 77% of patients and clinical success in 55% of patients, with follow-up periods of 3 months to 1 year [2626. Wholey M, Jarmolowski C. New reperfusion devices: the Kensey catheter, the atherolytic reperfusion and the transluminal extraction catheter. Radiology 1989;172:947-952. ].
ROTATIONAL ATHERECTOMY
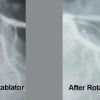
High-speed rotational coronary atherectomy has a different and unique mechanism: it removes plaque by abrading the atherosclerotic material producing millions of tiny particles which are dispersed into the distal coronary circulation. The concept was developed by Auth, a biomedical engineer. In the early 1980s, Auth, working at the time in the field of laser surgery, began to investigate the possibility of using a rotational device as a mechanical alternative for debulking atherosclerotic plaque. Rotary ablation preferentially attacked hard and even calcified atherosclerotic plaque because of its selective differential cutting effect. The burr ( Figure 17) spinning at 160,000 to 200,000 rpm pulverises atherosclerotic plaque into tiny particles, the size of which should be of no concern for the prospective coronary circulation. Different studies conducted with different devices found no deleterious effect on global or segmental left ventricular wall motion. However, too low a speed (<75,000 rpm) of rotation was notorious for generating larger particles and heat was generated by forceful advancement of the burr leading to a deceleration >5000 rpm. After several experimental animal studies in vitro and in vivo, the first case of rotational atherectomy (rotablation) in humans was performed in peripheral arteries by Zacca [2727. Zacca NM, Raizner AE, Noon GP, Short D, 3rd, Weilbaecher D, Gotto A, Jr., Roberts R. Treatment of symptomatic peripheral atherosclerotic disease with a rotational atherectomy device. Am J Cardiol 1989;63:77-80. ] in Houston. The first coronary rotablation on January 6, 1988, by Fourrier and Bertrand [2828. Fourrier JL, Bertrand ME, Auth DC, Lablanche JM, Gommeaux A, Brunetaud JM. Percutaneous coronary rotational angioplasty in humans: preliminary report. J Am Coll Cardiol. 1989;14:1278-82. ] was performed in a 68-year-old woman with stable angina pectoris. The coronary angiography showed a tight, relatively discrete narrowing of the proximal left anterior descending coronary artery. A 1.75 mm burr was used and, after several passes, there was a very modest enlargement of the lumen ( Figure 18 ). The procedure was then completed with balloon dilatation.
Rotablation became quite popular in the early 1990s. A number of trials were launched: the ERBAC trial [2929. Reifart N, Vandormael M, Krajcar M, Gohring S, Preusler W, Schwarz F, Storger H, Hofmann M, Klopper J, Muller S, Haase J. Randomized comparison of angioplasty of complex coronary lesions at a single center. Excimer Laser, Rotational Atherectomy, and Balloon Angioplasty Comparison (ERBAC) Study. Circulation. 1997;96:91-98. ], DART study, COBRA, ARTIST [3030. vom Dahl J, Radke PW, Haager PK, Koch KC, Kastrau F, Reffelmann T, Janssens U, Hanrath P, Klues HG. Clinical and angiographic predictors of recurrent restenosis after percutaneous transluminal rotational atherectomy for treatment of diffuse in-stent restenosis. Am J Cardiol. 1999;83:862-867. ] and ROSTER [3131. Sharma SK, Kini A, Mehran R, Lansky A, Kobayashi Y, Marmur JD. Randomized trial of Rotational Atherectomy Versus Balloon Angioplasty for Diffuse In-stent Restenosis (ROSTER). Am Heart J. 2004;147:16-22. ] trials produced ambiguous results and it was thought at that time that rotablation could not compete with vascular brachytherapy which was emerging as a transitory “gold” standard for prevention and treatment of in-stent restenosis.
Again, with the use of stent implantation being virtually by default, the practice of rotablation rapidly declined. The rate of procedures is now inferior to 1% and reserved to resistant or to severely calcified lesions.
ROTACS SYSTEM
In the first years of coronary interventional cardiology, it appeared that total chronic complete occlusion was a limiting factor for nonsurgical recanalisation procedures. With conventional methods and traditional guidewires, recanalisation had a very low success rate. Vallbracht [3232. Vallbracht C, Liermann DD, Prignitz I, Beinborn W, Roth FJ, Kollath J, Landgraf H, Kaltenbach M. Low-speed rotational angioplasty in chronic peripheral artery occlusions: experience in 83 patients. Work in progress. Radiology. 1989;172:327-330. ] and Kaltenbach invented a new system which was specifically designed for chronic total occlusion. Basically, it was an electrically driven rotating catheter, consisting of four steel coil wires (0.2 mm each) with an inner lumen allowing an exchange of wires and the injection of contrast medium. Covered by a very flexible Teflon tube, the catheter had an olive-shaped blunt tip ( Figure 19). The wire rotated at very low speed, usually 200 rpm, induced by a small hand-held motor unit ( Figure 20). The two pioneers started to work with this device in Frankfurt in 1984. They started in patients with total chronic coronary occlusion and from April 1987 to February 1988 they used this technique in 20 patients [3333. Kaltenbach M, Vallbracht C. [Rotation angioplasty of chronic coronary artery stenosis]. Herz. 1990;15:292-298. ]. In 1991, Kaltenbach and Vallbracht [3434. Kaltenbach M, Vallbracht C, Hartmann A. [Recanalization of chronically obstructed coronary vessels using ROTACS (low-speed rotational angioplasty. Early and long-term results in 152 patients following unsuccessful conventional angioplasty]. Fortschr Med. 1991;109:331-336, 340. ] published their experience in 152 patients: the success rate was 55%. The angiographically determined long-term success was 72%. However, new wires and new techniques sent that technique to oblivion in the mid 1990s.
LASER ANGIOPLASTY
Laser (Light Amplification by Stimulated Emission of Radiation) systems are producing energy. They have been used in several medical areas. Laser was introduced in interventional cardiology at the beginning of the 1980s. In 1981, Lee reported a “laser dissolution” of coronary atherosclerotic obstruction. Similar experiments performed by Abela and Conti and later by Choy made the same observations in cadaver hearts.
From September 19 to 22, 1983, in Toulouse, France, Marco, Choy and Stertzer performed laser recanalisation of occluded coronary arteries during surgical interventions performed by Fournial in 5 patients. The first patient had a complete chronic obstruction of the right coronary artery. An attempt at laser recanalisation was carried out, and for safety reasons a venous graft was implanted on this vessel. These preliminary results were presented during the first live course demonstration in Toulouse (September 22-23, 1983) and later at the American College of Cardiology meeting in Dallas (March 25-29, 1984).
After these preliminary experiments, laser radiation was investigated extensively in interventional cardiology. The first generation used continuous wave lasers with Nd:YAG laser in Europe and Argon laser in the USA. It appeared that the thermal excess was creating important arterial damage, responsible for a high rate of restenosis. This led to the discontinuation of the device.
The technique resurfaced when Grundfest [3535. Grundfest WS, Litvack F, Forrester JS, Goldenberg T, Swan HJ, Morgenstern L, Fishbein M, McDermid IS, Rider DM, Pacala TJ, et al. Laser ablation of human atherosclerotic plaque without adjacent tissue injury. J Am Coll Cardiol. 1985;5:929-933. ] proposed the delivery of excimer laser energy through optical fibres. Later, a second generation of pulsed wave lasers was shown to induce only limited thermal injury to the surrounding tissue. In the end, Excimer, Holmium, or CO2 devices were used.
A number of registries were opened. The Spectranetics excimer laser registry [3636. Bittl JA. Clinical results with excimer laser coronary angioplasty. Semin Interv Cardiol. 1996;1:129-134. ] included 2,432 patients. Another registry conducted by Litvack [3737. Litvack F, Eigler N, Margolis J, Rothbaum D, Bresnahan JF, Holmes D, Untereker W, Leon M, Kent K, Pichard A. Percutaneous excimer laser coronary angioplasty: results in the first consecutive 3,000 patients. The ELCA Investigators. J Am Coll Cardiol. 1994;23:323-329. ] enrolled 3,000 patients with 84% procedural success; however, several procedural complications were noted with death, myocardial infarction, and the need for emergency bypass surgery in 3.8% of cases. The restenosis rate was 58%. Several randomised trials compared laser angioplasty with other techniques of interventional cardiology (ERBAC trial [2929. Reifart N, Vandormael M, Krajcar M, Gohring S, Preusler W, Schwarz F, Storger H, Hofmann M, Klopper J, Muller S, Haase J. Randomized comparison of angioplasty of complex coronary lesions at a single center. Excimer Laser, Rotational Atherectomy, and Balloon Angioplasty Comparison (ERBAC) Study. Circulation. 1997;96:91-98. ], AMRO study, LAVA study [3838. Appelman YE, Koolen JJ, Piek JJ, Redekop WK, de Feyter PJ, Strikwerda S, David GK, Serruys PW, Tijssen JG, van Swijnregt E, Lie KI. Excimer laser angioplasty versus balloon angioplasty in functional and total coronary occlusions. Am J Cardiol. 1996;78:757-762. ]): none of these trials showed a benefit of laser angioplasty over the comparable techniques.
The overall results were not convincing and laser angioplasty has been almost completely abandoned, mostly in favour of better coronary guidewires and routine use of coronary stenting.
LINEAR EVERTING BALLOON
In 1981, Fogarty [3939. Fogarty TJ, Kinney TB. Intraoperative coronary artery balloon-catheter dilatation. Am Heart J. 1984;107:845-851. ] introduced the concept of the linear extrusion catheter. This device included a pliable, nonelastomeric balloon which was inverted within the lumen of the catheter. The catheter was advanced in front of the stenosis. Fluid injection (4-6 atm) into the catheter induced extrusion of the balloon which was anchored in the artery, and complete extrusion was obtained while pushing on the proximal system. In a way, it was a kind of automatic crossing of the lesion. The combination of the application of dilating forces reduced the shear stress ( Figure 21 ). In 1984, Fogarty [4040. Fogarty TJ, Kinney TB, Finn JC. Current status of dilatation catheters and guiding systems. Am J Cardiol. 1984;53:97C-101C. ] and Kinney reported the results of a multicentre study of peripheral adjunctive intraoperative dilations with the linear extrusion catheter. They obtained an 81% primary success rate. Yet it soon appeared that the everting balloon was generally pushing the atherosclerotic material into the distal part of the artery: the procedural success rate was very low. Complications (occlusive dissection) were frequent and the technique was discarded.
CUTTING BALLOON
Restenosis remained the major concern of coronary angioplasty. A number of trials conducted to prevent neointimal proliferation failed. The problem of recoil and remodelling was studied again more carefully. In this context, Barath introduced the concept of a balloon dilatation with microsurgical blades creating a notch across the area of hoop tension of the plaque ( Figure 22 and Figure 23 ). This device included a number of challenges such as the size of the dilatationmicro blades and the flexibility of the system. This required a number of technical innovations. Finally, the first case was performed in man by Hosakawa. A comparative trial was launched by Bonan et al [4141. Mauri L, Bonan R, Weiner BH, Legrand V, Bassand JP, Popma JJ, Niemyski P, Prpic R, Ho KK, Chauhan MS, Cutlip DE, Bertrand OF, Kuntz RE. Cutting balloon angioplasty for the prevention of restenosis: results of the Cutting Balloon Global Randomized Trial. Am J Cardiol. 2002;90(10):1079-1083. ] and failed to demonstrate a significantly lower rate of restenosis. Later, a number of trials were launched and overall it appeared that the benefit in terms of prevention of restenosis was minimal and only observed in particular patients. Later, it was suggested that the cutting balloon might be useful as a preliminary treatment in very stiff lesions or in lesions where conventional balloons tended to slip out (melon seed phenomenon).
BRACHYTHERAPY
Intracoronary brachytherapy was an attempt to reduce restenosis. Because of its intricacy, it was essentially reserved to in-stent restenosis treatment. Gamma and beta radiation were explored after a first patient had been treated by Condado in 1996 [4242. Condado JA, Waksman R, Gurdiel O, Espinosa R, Gonzalez J, Burger B, Villoria G, Acquatella H, Crocker IR, Seung KB, Liprie SF. Long-term angiographic and clinical outcome after percutaneous transluminal coronary angioplasty and intracoronary radiation therapy in humans. Circulation. 1997;96:727-732. ]. While gamma radiation needed substantial protection measures for the personnel who essentially had to leave the room, beta radiation hardly increased radiation outside the patient. To prevent one patient from having to come back for repeat balloon angioplasty, 10 patients had to be irradiated. This was clearly not a bargain and the technique would not have survived even if its clinical evaluation had not fallen during the time of the introduction of drug-eluting stents (DES). In addition, there was clearly a late catch-up of restenosis with a certain risk of late stent thrombosis, not unlike that of the first generation DES.
THERAPEUTIC ULTRASOUND
After having his teeth cleaned with ultrasound technology, Siegel considered the interest of ultrasound energy to debulk coronary arteries blocked by atherosclerotic material. Baxter laboratories provided ultrasound probes initially designed for the percutaneous fragmentation of kidney stones. In the first animal experiments it was observed that the device ( Figure 24 and Figure 25 ) generated a lot of heat but turned the rigid, hard atherosclerotic aortic wall into a compliant and soft tissue [4343. Siegel R, Fishbein M, Forrester JS. Ultrasonic ablation: a new method for recanalization of partially or totally occluded arteries. Circulation. 1988;78:1443-1448. ]. With Cumberland he performed the first human experiment in Sheffield in April 1989 [4444. Gunn J, Wales C, Baig W, Siegel R. Clinical trial of percutaneous periheral ultrasound angioplasty. J Am Coll Cardiol. 1993;22:480. ]. Later, the device was used for intracoronary ultrasound thrombolysis by Hamm [4545. Hamm CW. Intravascular therapeutic ultrasound thrombolysis in a patient with acute myocardial infarction. Am J Cardiol 1997;80:200-204. ] (1994). Finally, a registry named CRUSADE collected cases from France, Germany and the UK for recanalisation of chronic total occlusion [4646. Steffen W, Bertrand M, Hamm CW. Multicenter experience with therapeutic ultrasoundcoronary angioplasty in symptomatic patients. 1995;92:1570. ]. Therapeutic intracoronary ultrasound has since been abandoned.
Coronary stenting
After the golden era of new innovative technologies, coronary angioplasty was still facing two major challenges: acute occlusion during the procedure leading to emergency CABG (which in most cases was accompanied by a large infarction and had a high mortality risk), and the problem of restenosis. Coronary stenting has brought a solution to both these major problems. There is still debate concerning the origin of the word stent. By common belief, the word derives from the name of Charles Stent, an English dentist. It was proposed by Johannes "Jan" Fredericus Samuel Esser (1877-1946), a Dutch plastic surgeon who pioneered innovative methods of reconstructive surgery on soldiers wounded in the First World War. He is thought to have coined the term "stent" in 1917 to describe his use of a dental impression compound invented in 1856 by the English dentist Charles Stent (1807–1885) to create a form for facial reconstruction. The term "stent" was later extended to mean a device to expand constricted tubes of body tissue. In 1912, Carrel suggested “The permanent intubation of a large vessel is a simple operation. It may become practical, if the shape and the nature of the tube be modified as to avoid laceration (…). The question of the application of this method to human surgery may then, possibly, be considered.”
The history of the first coronary stent is based upon the meeting of two Swedish individuals. The first, Wallsten, was the designer of a revolutionary machine intended to manufacture paper, while the other, Senning, was a prominent cardiovascular surgeon. During a party, Dr Senning explained to Wallsten the difficulties of treating aortic dissection and marvelled at his concept of a mechanical scaffolding of the arterial wall by a latticed metallic tube. Wallsten, very excited, decided to tackle the problem of endovascular arterial prostheses. He created the Wallstent, but he had some difficulty finding a solution for a percutaneous approach. This was achieved by Christian Imbert. He created a system where the metallic self-expandable prosthesis is constrained by a kind of sleeve ( Figure 26 ). The removal of the sleeve results in the deployment of the prosthesis. The self-expandable stent was thus implanted via a percutaneous femoral approach. Imbert contacted Sigwart in Lausanne, where the company Medivent was located, and Puel in Toulouse for clinical testing in animals, peripheral arteries, and ultimately coronary arteries.
They performed some experiments on sheep and dogs. At a first glance, these experiments showed that it was easy to implant the endocoronary prosthesis percutaneously. They also confirmed rapid endothelialisation of the struts. However, these animal experiments failed to predict the high risk of subsequent thrombosis. The first stent implantation was performed by Puel on March 28, 1986 [4747. Puel J, Joffre F, Rousseau H. Endoprothèses coronaires dans la prévention de la restenose post dilatation. Resultats préliminaires. Arch Mal coeur. 1987;80:1311-2. ] ( Figure 27 ). The history of this first patient is quite simple. He was a 63-year-old male with arterial hypertension, and a symptomatic restenosis 6 months after balloon treatment of the mid LAD. The patient was not given preparatory antiplatelet drugs or statins. He only received subcutaneous heparin during the procedure and over the next 6 weeks. Fortunately, he had no stent thrombosis or in-stent restenosis. However, he did not escape the progression of the atherosclerotic process since he has had recurrent episodes of angina pectoris related to a new lesion on the ostium of the LAD and another one on the left circumflex coronary artery which was treated in 2004 by a new stent implantation. In the following weeks, seven other patients received a self-expandable Wallstent by Puel and Sigwart without any complications.
Initial results were, however, misleading since the next four patients developed a subacute stent thrombosis. With a single antithrombotic treatment based upon full doses of heparin, the risk of thrombosis was very high.
Later, Sigwart [4848. Sigwart U, Puel J, Mirkovitch V, Joffre F, Kappenberger L. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med. 1987;316:701-6. ] performed stent implantation under full anticoagulation with heparin followed by oral anticoagulation with warfarin. He used a combination of heparin, coumadin, dextran, acetylsalicylic acid, dipyridamole and was even suggesting the use of sulphinpyrazone. This medical treatment decreased the risk of stent thrombosis but it remained high (between 5% and 10%). Coronary stenting was initially mainly used to treat acute or impending coronary occlusion after PCI, which carries a high risk of reocclusion per se. In an initial paper of 1991, Serruys [4949. Serruys P, Strauss B, Beatt K. Angiographic follow-up after placement of a self-expanding coronary artery stent. N Engl J Med. 1991;324:13-17. ] gave details of the first 105 patients treated in different centres and reported a rate of subacute thrombosis of over 20%. Of note, these were mainly bail-out situations. Pleasingly, the rate of restenosis was only 14%, far below the level of that of balloon angioplasty.
It was necessary to wait nearly 10 years to minimise the risk of subacute thrombosis with the expansion of the indication to elective cases and the use of dual antiplatelet treatment (acetylsalicylic acid and ticlopidine). The benefit of this combined treatment was discovered by chance. There was at that time a French registry collecting cases of stent implantation and the different regimens of anticoagulation used in the management of these patients [5050. Karrillon GJ, Morice MC, Benveniste E, Bunouf P, Aubry P, Cattan S, Chevalier B, Commeau P, Cribier A, Eiferman C, Grollier G, Guerin Y, Henry M, Lefevre T, Livarek B, Louvard Y, Marco J, Makowski S, Monassier JP, Pernes JM, Rioux P, Spaulding C, Zemour G. Intracoronary stent implantation without ultrasound guidance and with replacement of conventional anticoagulation by antiplatelet therapy. 30-day clinical outcome of the French multicenter registry. Circulation. 1996;94:1519-1527. ]. Surprisingly, Barragan from Marseille had very few cases of stent thrombosis [5151. Barragan P, Pietri P, Villain P, Silvestri M, Roquebert PO. Antiplatelet therapy during coronary endoprosthesis placement. Arch Mal Coeur. 1996;89:1515-1520. ]. A careful analysis of the regimen used in his centre revealed that the single difference from other centres was the simultaneous prescription of acetylsalicylic acid and ticlopidine. This resulted from a trial named TACT initiated by Bertrand [5252. Bertrand M, Allain H, Lablanche J. A randomized trial of ticlopidine vs. placebo for prevention of acute closure and restenosis after PTCA: The TACT study. Circulation. Supp I 1990:190. ]comparing ticlopidine and acetylsalicylic acid for prevention of restenosis. The trial was negative regarding recurrence but showed a significant reduction of major cardiac events when the patients received acetylsalicylic acid and ticlopidine. After completion of the trial, Barragan continued to use dual antiplatelet treatment and as a result achieved the lowest rate of subacute stent thrombosis in the French registry [5151. Barragan P, Pietri P, Villain P, Silvestri M, Roquebert PO. Antiplatelet therapy during coronary endoprosthesis placement. Arch Mal Coeur. 1996;89:1515-1520. ]. This combination was not ubiquitously adopted for two reasons. Simultaneously in Italy, Colombo claimed that in general the deployment of the stents was less than perfect (as he observed in a large series of intravascular ultrasound (IVUS) performed after stent implantation). Investigators were, however, reluctant to perform IVUS systematically due to cost and additional risk. The alternative recommendation was to complete every procedure by high pressure inflation. The second reason came from the company manufacturing ticlopidine. They were approached by a number of “angioplasters” who eagerly wished to launch a randomised trial comparing full anticoagulation with K antagonists vs. acetylsalicylic acid plus ticlopidine. The company was not interested because they were preparing the launch of clopidogrel, the safer successor to ticlopidine. Finally, two trials (ISAR [5353. Schömig A, Neuman F, Kastrati A. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary stents. N Engl J Med. 1996;334:1084-1089. ] and FANTASTIC [5454. Bertrand ME, Legrand V, Boland JP. randomized multicenter comparison of conventional anticoagulation vs. antiplatelet therapy in unplanned and elective coronary stenting. The FANTASTIC study. Circulation. 1998;98 1597-603. ]) were conducted without support. They established the superiority of the dual antiplatelet treatment once and for all with a rate of stent thrombosis around 0.5%. Two additional trials, MATTIS and STAR, confirmed these results. The next milestones were the BENESTENT (I and II) trials [5555. Serruys PW, de Jaegere P, Kiemeneij F, Macaya C, Rutsch W, Heyndrickx G, Emanuelsson H, Marco J, Legrand V, Materne P, Belardi J, Sigwart U, Colombo A, Goy JJ, van den Heuvel P, Delcan J, Morel MA. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331:489-95. , 5656. Serruys PW, van Hout B, Bonnier H, Legrand V, Garcia E, Macaya C, Sousa E, van der Giessen W, Colombo A, Seabra-Gomes R, Kiemeneij F, Ruygrok P, Ormiston J, Emanuelsson H, Fajadet J, Haude M, Klugmann S, Morel MA. Randomised comparison of implantation of heparin-coated stents with balloon angioplasty in selected patients with coronary artery disease (Benestent II). Lancet. 1998;352:673-681. ] conducted in Europe and the STRESS trial [5757. Fishman D, Leon M, Baim D. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. The STRESS trial. N Engl J Med. 1994;331:496-501. ] conducted in the USA. These trials definitely established that bare metal stents (BMS) were able to reduce the risk of restenosis markedly. Moreover, these trials demonstrated that the mechanism of restenosis was at least as much dependent on negative remodelling (prevented by the scaffolding prosthesis) as on neointimal proliferation.
Meanwhile, a number of new stents were proposed - the Palmaz-Schatz ( Figure 28 ), Wiktor, Gianturco-Roubin, NIR, Multi-link, etc. Improvement of stent platforms is still ongoing.
During a meeting in Salzburg in 1996, Serruys and his colleagues launched a new trial comparing multivessel stenting and bypass surgery in patients with multivessel disease. The trial started in 1997, was completed in 1998, and 1-year follow-up was presented at the European Society of Cardiology meeting in 1999 [5858. Serruys PW, Unger F, van Hout BA, van den Brand MJ, van Herwerden LA, van Es GA, Bonnier JJ, Simon R, Cremer J, Colombo A, Santoli C, Vandormael M, Marshall PR, Madonna O, Firth BG, Breeman A, Morel MA, Hugenholtz PG. The ARTS study (Arterial Revascularization Therapies Study). Semin Interv Cardiol. 1999;4:209-219. ] and results published in the New England Journal of Medicine in 2001 [5959. Serruys PW, Unger F, Sousa JE, Jatene A, Bonnier HJ, Schonberger JP, Buller N, Bonser R, van den Brand MJ, van Herwerden LA, Morel MA, van Hout BA. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117-1124. ]. It was demonstrated that in these particular patients that coronary stents and surgery had the same rate of mortality and myocardial infarction, but that surgery induced more strokes in the perioperative period. The marked difference was the rate of re-intervention, which was significantly lower after surgery than after multi-stenting.
During the last five years of the 20th century, a number of companies were very active in developing DES. A first approach was a stent coated with heparin used in BENESTENT II [5858. Serruys PW, Unger F, van Hout BA, van den Brand MJ, van Herwerden LA, van Es GA, Bonnier JJ, Simon R, Cremer J, Colombo A, Santoli C, Vandormael M, Marshall PR, Madonna O, Firth BG, Breeman A, Morel MA, Hugenholtz PG. The ARTS study (Arterial Revascularization Therapies Study). Semin Interv Cardiol. 1999;4:209-219. ] but this new device was not convincing. In 1999, Cordis laboratory introduced a stent eluting a drug named rapamycin. The first implantations in men were conducted in Sao Paulo and Rotterdam with follow-up at 4 or 6 months using quantitative coronary angiography and quantitative motorised intravascular ultrasound pullback. The preliminary results were very exciting: for the first 15 patients, there was no restenosis and no neointimal hyperplasia on IVUS analysis of the stent. In September 2001, the results of RAVEL [6060. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, Molnàr F, Falotico R; RAVEL Study Group. Randomized Study with the Sirolimus-Coated Bx Velocity Balloon-Expandable Stent in the Treatment of Patients with de Novo Native Coronary Artery Lesions. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Eng J Med. 2002;346:1773-1780. ], a study of 238 patients comparing the use of a drug-eluting stent (CYPHER® sirolimus-eluting stent) vs. a bare metal stent, were presented in Vienna. The results were flabbergasting: restenosis rate with CYPHER®: 0. This led to a number of sceptical comments: “zero risk does not exist in medicine!”. Later, a new stent eluting paclitaxel was proposed and a number of studies with sirolimus and paclitaxel stents were performed: SIRIUS [6161. Holmes DR, Jr., Leon MB, Moses JW, Popma JJ, Cutlip D, Fitzgerald PJ, Brown C, Fischell T, Wong SC, Midei M, Snead D, Kuntz RE. Analysis of 1-year clinical outcomes in the SIRIUS trial: a randomized trial of a sirolimus-eluting stent versus a standard stent in patients at high risk for coronary restenosis. Circulation. 2004;109:634-640. ], E-SIRIUS [6262. Schofer J, Schluter M, Gershlick AH, Wijns W, Garcia E, Schampaert E, Breithardt G. Sirolimus-eluting stents for treatment of patients with long atherosclerotic lesions in small coronary arteries: double-blind, randomised controlled trial (E-SIRIUS). Lancet. 2003;362:1093-1099. ], C-SIRIUS [6363. Schampaert E, Cohen EA, Schluter M, Reeves F, Traboulsi M, Title LM, Kuntz RE, Popma JJ. The Canadian study of the sirolimus-eluting stent in the treatment of patients with long de novo lesions in small native coronary arteries (C-SIRIUS). J Am Coll Cardiol .2004;43:1110-1115. ], TAXUS I, II, III, IV [6464. Halkin A, Stone GW. Polymer-based paclitaxel-eluting stents in percutaneous coronary intervention: a review of the TAXUS trials. J Interv Cardiol 2004;17:271-282. ], clearly establishing that restenosis was not completely abolished but markedly reduced to an acceptable rate with the sirolimus or the paclitaxel stents.
Over the following years, many new DES were proposed, i.e., second generation DES using new eluting drugs such as everolimus, zotarolimus, biolimus. A further step was achieved with the SYNTAX study [6565. Serruys P, Morice M, Kappetein A, Colombo A, Holmes D, Mack M, Ståhle E, Feldman T, van den Brand M, Bass E, Van Dyck N, Leadley K, Dawkins K, Mohr F; SYNTAX Investigators. Percutaneous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Eng J Med 2009;360:961-972. ], a trial of 1,800 patients comparing the paclitaxel stent vs. surgery in patients with multivessel disease and/or with unprotected left main stenosis. It was the first time that a randomised trial had been launched in an area which was considered to be an uncontested domain of surgery. The SYNTAX trial was designed as a non-inferiority trial with a primary objective of a combination of death, MI, stroke, and target lesion revascularisation. In view of the fact that the combined endpoint included TLR, PCI was unable to meet the criteria for non-inferiority, which led many people to judge PCI inferior to surgery. Nevertheless, considering the second endpoint of death, MI and stroke, it appears that multistenting was not inferior to surgery in the lower risk segments of the trial, and the rate of stroke was lower after PCI than after surgery. Comparing the higher risk tertiles of the SYNTAX trial to typical DES study patients, it became apparent that they are not usually stented in studies, let alone in real life. Hence, this confirms that the current indications for stenting in multivessel disease are reasonable. The SYNTAX trial was a landmark trial which has had 3 major consequences: 1) the need in this area to have a heart team including several investigators (“angioplasters”, surgeons, anaesthesiologists and others) who decide the optimal strategy; 2) a SYNTAX score [6666. Dawkins KD, Morel MA, Serruys PW. Counting the score: the SYNTAX Score and coronary risk. EuroIntervention. 2009;5:33-35. ] based on a careful analysis of coronary anatomy, permitting the separating out of indications for PCI in case of a low or medium SYNTAX score; and 3) the feasibility and safety of PCI for the treatment of unprotected left main stent narrowing was demonstrated [6767. Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010; 121:2645-2653. ], which has led to a recommendation in the ESC guidelines with a level of evidence IIa C [6868. Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Follguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on myocardial revascularization. Task force on myocardial revascularization of the European Society of cardiology (ESC) and the European Association for cardio-thoracic surgery (EACTS);European Association for percutaneous cardiovascular interventions (EAPCI). Eur Heart J. 2010;31:2051-2555. ].
Today, research essentially focuses on new designs, new drug for eluting, and bioabsorbable stents. Bioabsorbable stents are certainly the most exciting area for future developments, despite the often heard phrase: “Bioabsorbable stents are the future of PCI, and they always will be!”
Further reading
Readers who are interested in more historical detail on coronary intervention are invited to explore 'The History of Coronary Angioplasty' by Philippe Gaspard: