Cardiac catheterisation in animals
The landmark experiments on cardiac catheterisation in animals were performed by the French physiologist Claude
Bernard ( Figure 1) who was the “father” of modern experimental physiology.
He performed cardiac catheterisation in animals to address a curious but crucial controversy in the 1840s:
In 1780, Lavoisier had suggested that animal heat was produced as a result of respiratory gas exchange during blood passage through the lungs. Subsequent advocates of Lavoisier’s theory concluded that the temperature of blood entering into the left heart was higher than that of the blood returning to the right heart and the pulmonary artery.
This concept was universally accepted for almost half a century, but in 1837 Gustav Magnus proposed an alternative hypothesis: namely that combustion takes place in the tissues. The two opposing theories were vigorously debated. The first hypothesis was strongly upheld by several famous proponents including Gay-Lussac and Magendie (1783-1855). Magendie was one of the prominent advocates of experimental medicine. Claude Bernard, an assistant to Magendie, designed an experiment to determine which hypothesis was correct. He considered that measurement of blood temperature in each of the ventricular cavities would provide a conclusive answer. An initial observation was made in 1844 [11. Bernard C. Leçons sur la chaleur animale. In: fi ls JBB, ed. Paris. 1846;3. ] using a horse as the experimental subject. After incising the carotid artery, Claude Bernard introduced a long mercury thermometer into the left ventricle through the incision and recorded the temperature of the blood. Then he incised the jugular vein and advanced the thermometer into the right ventricle. He observed that the temperature was slightly (by a few tenths of a degree) higher on the right side of the heart. This invalidated the pulmonary combustion hypothesis and suggested that combustion occurred in all the tissues of an organism.
Over the next 30 years, Claude Bernard repeated the experiments with more accurate devices, such as the thermometer conceived by Walferdin, a specialist in temperature measurement, and a later modification by Becquerel, that could detect temperature differences of as little as 0.01°C. During the academic year 1871-1872, he delivered 22 lectures on this topic and published a book entitled “Leçons sur la chaleur animale” (“Observations on animal heat”). In the fifth and most striking chapter he carefully described the catheterisation technique in a dog.
Thus, as emphasised by Buzzi et al [22. Buzzi A. Claude Bernard on cardiac catherization. Am J Cardiol. 1959;4:405. ], Claude Bernard left behind a very detailed description of cardiac catheterisation with all the steps of the procedure.
On November 29, 1847, at the Collège de France, Claude Bernard performed the firrst measurement of intracardiac pressures in the presence of Magendie and Rayer. He opened the jugular vein of a small dog and introduced a glass tube into the right ventricle through the incision. He connected the glass tube to a “cardiodynamometer”, a pressure recording system developed by Poiseuille. He measured the right ventricular pressure and found it to be lower than that of the peripheral arteries. Autopsy showed a perforation of the right ventricle which was not surprising owing to the stiffness of the glass tube device.
Thus, one must acknowledge the major contribution of Claude Bernard. Not only was he able to solve a controversial enigma elegantly, but he also described in detail the technique of cardiac catheterisation in animals and emphasised the need to make physiological observations with a subject in the basal state. In addition, it is interesting to note that the Collège de France was unusual in that it allowed professors to decide their curricula. This encouraged free thinking and experimentation.
The next step was the investigation of intracardiac pressures by two French physicians, A. Chauveau and E.J. Marey [33. Chauveau A, Marey EJ. Détermination graphique du rapport du choc du coeur avec les mouvements des oreillettes et des ventricules. Expérience faite à l’aide d’un appareil enregistreur (sphygmographe) Compt. rend. des séances de l’Académie des sciences. 1861;3:622. , 44. Chauveau A, Marey EJ. Détermination graphique des rapports du choc du coer avec les mouvements des oreillettes et des ventricules. Compt. rend. des séances de l’Académie des sciences. 1862;4:32. , 55. Chauveau A, Marey EJ. Physiologie médicale de la circulation du sang. Delahaye, Paris. 1863. ]. Again, this was a result of a physiological controversy; on this occasion, the problem concerned the nature and timing of the cardiac apex beat:
Harvey and later Laennec suggested that the impulse felt under the left nipple was due to ventricular contraction and began with ventricular systole. However, its exact timing was a matter of controversy. Auguste Chauveau ( Figure 2 ) was a professor of veterinary medicine in Lyon. He was particularly interested in the relationship between heart sounds and cardiac events. In a book published in 1856 by J.B. Baillière entitled “Nouvelles recherches expérimentales sur les mouvements et les bruits normaux du coeur envisagés du point de vue de la physiologie médicale” (New experimental insights into the movements and normal sounds of the heart from a physiological viewpoint) he refuted theories proposed by several previous authors such as Beau, Senac, Hunter and Béclard; his conclusions were in agreement with those of Harvey and Laennec.
Chauveau met a young engineer, Etienne Jules Marey ( Figure 3 ) who was also a physician and a technical genius in the field of recording and analysing motion. Marey had already designed a sphygmograph with which he was able to record arterial pulse transmission. In his doctoral thesis, he provided a physiological interpretation of the dicrotic notch recorded on the pressure wave form of peripheral arteries.
To clarify the timing of the apical beat, Chauveau and Marey, disciples of Claude Bernard’s experimental physiology, planned to introduce a pressure recording apparatus into the heart. The technique was described in their first presentation at the Academy of Sciences [33. Chauveau A, Marey EJ. Détermination graphique du rapport du choc du coeur avec les mouvements des oreillettes et des ventricules. Expérience faite à l’aide d’un appareil enregistreur (sphygmographe) Compt. rend. des séances de l’Académie des sciences. 1861;3:622. ]. In fact, they used a system of levers connected to a continuous recorder, which was initially described by Karl Vierordt from Tuebingen, a student of Ludwig who had invented a kymograph in 1847. Unfortunately, the system conceived by Chauveau and Marey was not a success due to the inertia and friction of the long column of fluid inside the tube. Hence, Chauveau and Marey modified the transmitting device. They used “two long tubes tied together, and each closed at both extremities by a thin rubber balloon, inflated with air”. These tubes were introduced through the jugular vein of an unanaesthetised horse ( Figure 4 ). One catheter was positioned in the right ventricle and the other, 12 cm shorter, was postioned in the atrium. An additional apparatus recorded the apex beat. They obtained simultaneous recordings of pressure changes and the apical heart beat. They concluded that “these tracings demonstrate irrefutably that the apical heart beats is an effect of ventricular systole”. Their novel double-lumen technique is regarded as the true precurser of modern intracardiac pressure recording techniques.
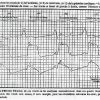
In 1863, Chauveau and Marey presented a definitive account of intracardiac pressure recordings and their interpretation ( Figure 5 ). It contained numerous reproductions of intraventricular recordings. They described the first simultaneously recorded tracing in the left ventricle and the aorta and were the first to describe the isometric phase of ventricular contraction.
In 1863, they published a book describing a dedicated catheter introduced via the carotid artery into the left ventricle. They also defined the normal values of pressures recorded in the right atrium, the right ventricle, left ventricle and aorta.
A footnote in the book is of particular interest: Marey stated that “one can be reassured of the innocuity of this method by examining the horse who is scarcely disturbed, walks and eats as usual. In only a few instances, the pulse is slightly increased, especially at the time of the introduction of catheters within the heart cavities”.
Marey received the prestigious physiology prize of the Institut de France in 1875 and, in his nomination speech, Claude Bernard remarked that “the most striking proof of Mr. Marey’s success is found in the fact that his procedures have become working and research tools it will no longer be possible to do without”. It was a remarkable premonition on the part of a great scientist and a century later this premonition would be extended to the clinical arena.
From 1864 to 1900, several papers and books criticised the work of Chauveau on intracardiac blood pressure recording. This was mainly due to the work of Adolf Fick (1829-1901). He was the anatomy demonstrator for Carl Ludwig at the Institute of Physiology in Zurich where he developed a pressure recording device. With this new device Fick started a study of morphology and measurement of the absolute values of intracardiac pressure curves. Adolf Fick felt that this new recording system was superior to the device described by Chauveau and Marey. He said that he had noted several artefacts in their published tracings and he criticised their calibration methods.
In the late 1880s, cardiac catheterisation came to be used routinely in physiology laboratories and gained prominence as an investigational technique. Nevertheless, there were protracted debates concerning the influence of catheters on the quality of the signals transmitted to the manometer: several authors critically analysed the role of friction, damping, etc. These technical issues were addressed at the end of the 19th century by Otto Franck. He laid down the mathematical and theoretical basis for accurate recordings. He described in detail the prerequisites for accurate reproduction of cardiac events, in form, magnitude and timing.
While at the University of Würzburg, Adolf Fick [66. Fick A. Ein neuer Blutwellenzeichner. Arch. f. Physiologie. 1864;563. ], who was well versed in mathematics, physics and physiology, tried to elucidate in quantitative terms the principles involved in the calculation of the cardiac output. In fact, Fick’s name is immortalised in cardiology because of a brief (one printed page) and obscure contribution at the Society of Physiology and Medicine of Würzburg in 1870 (Proceedings of the Würzburg Physicalische Medizinische Gesellschaft, July 9, 1870). It should be mentioned that this brief note did not state that the mixed blood of the pulmonary artery should be used for the formula CO=VO2/Ca-Cv to estimate cardiac output according to the Fick principle.
Adolf Fick never personally performed experiments in animals. It was only 16 years later that Grehant and Quinquaud [77. Grehant N, Quinquaud CE. Recherches expérimentales sur la mesure du volume du sang qui traverse les poumons en un temps donné. Compt rend. des séances de hebdomadaires de la Société de Biologie. 1886;5:159. ] reported the first measurements, performed in 6 dogs, at the Société de Biologie.
Zuntz and Hagmann [88. Zuntz N. Methode zur Messung der zirkulierenden Blutmenge und der Arbeit des Herzens. Pfluegers Archiv Europ J Physiol. 2009; 55:521-524. , 99. Zuntz N, Hagemann O. Untersuchungen über den Stoffwechsel des Pferdes bei Ruhe und Arbeit Landwirtschaftliche Jahrbücher, Zeitschrift für wissenschaftliche Landwirtschaft und Archiv des Königlich Preussischen Landes Ökonomie Collegiums 1898; Berlin: Paul Parey:1-438. ] described meticulously the correct technique for measuring blood flow according to the Fick principle. They attempted to combine blood flow measurements with direct recording of blood pressure in the pulmonary artery and aorta. In spite of all these refinements, it took more than 60 years to see the Fick principle applied to the measurement of cardiac output in man.
Cardiac catheterisation in humans
EARLY DEVELOPMENT
In the first two decades of the 20th century, cardiac catheterisation disappeared, at least partially, from the physiological arena. It was perhaps because attention was diverted to other great discoveries such as the description of x-rays by the German physicist Wilhelm Roentgen [1010. Roentgen WC, Über eine neue Art von Strahlen. In: Soiciety WPM, ed, 1895 ] on November 8, 1895, and the production of fluoroscopic images of the beating heart by Williams in 1896. In the same year, Haschek and Lindenthal described the first arteriogram obtained by injection of mercury compounds in the brachial artery of a cadaver, followed 3 years later by the first coronary arteriograms performed in cadaver animal hearts. In 1897, Stewart and Hamilton described the principle and method of cardiac output measurement, using the indicator dilution method.
Meanwhile, several investigators (Bleichroder, Unger and Loeb) attempted human catheterisation but did not disseminate their work for several years until the first heart catheterisation was performed and documented by Werner Forssmann on himself. Reportedly, the Portuguese neurologist Egas Moniz developed the technique of cerebral catheterisation and angiography in 1927.
THE FIRST CARDIAC CATHETERISATION
Werner Forssmann ( Figure 6 ) was born on August 29, 1904. In 1922, he entered the medical school at the Friedrich Wilhelm University in Berlin. In 1928, he prepared his doctoral thesis on the influence of liver extract on blood chemistry and started his first self-experiment by consuming one litre of that extract daily.
Immediately after graduation, he started a surgical residency at the Auguste Victoria Hospital in Eberswalde near Berlin. At the beginning of his medical studies Forssmann came across the experimental work of Claude Bernard, Chauveau and Marey. He was particularly fascinated by an old print in the papers of Marey, showing a man passing a tube through the jugular vein of a horse to measure changes in ventricular pressure. When he started to think about human experiments, he did not adopt the jugular vein approach but instead decided to try an approach via the cubital vein that involved passing a ureteric catheter towards the heart with the arm elevated.
The chief of Forssmann’s department was Dr. Schneider, a surgeon well versed in obstetrics, gynaecology and internal medicine. In the summer of 1929, Forssmann began to discuss with his colleagues and chief his plans concerning cardiac catheterisation. Schneider was reluctant, since he anticipated strong resistance from the academic community, but he encouraged Forssmann to do preliminary animal research to assess the safety of the procedure. Forssmann, stubborn and enthusiastic, was convinced that the procedure was safe and decided to carry on and proceed on himself without prior research, despite Schneider’s advice. He made a first attempt with the help of his colleague Peter Romeis. He opened his left cubital vein and inserted a lubricated ureteral catheter which he pushed for about 35 cm. The catheter got stuck and Peter Romeis, thinking that the experiment was becoming dangerous, urged Forssmann to stop the procedure.
Forssmann, disappointed by this initial failure, discussed his venture with Gerda Dizen, a surgical nurse supervisor. She could be convinced to participate and was made to believe that she would be the volunteer subject for this new attempt. She preferred to remain seated but Forssmann explained that it was better to work in a supine position, owing to the possible side effects of the local anaesthesia. As soon as she was lying on the table, he strapped her down to prevent her from seeing that he introduced the local anaesthesia into his own arm. Forssmann cut down his left arm vein and introduced the ureteral catheter for about 30 cm. He then released the nurse who was furious to discover that the catheter had been introduced into Forssmann’s arm. He covered the incision with a sterile drape and persuaded her to help him to get to the x-ray department, one floor below. With the nurse holding a mirror, Forssmann, behind the screen, was able to see the catheter which was in the area of the shoulder. He advanced it further up to the 60 cm mark and saw its tip in the region of the right atrium ( Figure 7 ). He could not move it any further having run out of length.
Within hours, the entire hospital learned about the event. The first reaction of Schneider was to reprimand Forssmann severely for his disobedience but he also realised that a publication would be of great interest. However, he felt that the manuscript should incorporate a therapeutic, in addition to a diagnostic application. To that end, Schneider authorised a second catheterisation which was performed in a woman dying of puerperal sepsis with shock. The goal was to observe the response to an intracardiac injection of adrenaline and strophanthin. The catheter was advanced without fluoroscopy and they measured the length of the inserted catheter. When they thought it was in place, they injected the drugs. Post-mortem examination showed that the catheter must have reached the right ventricle.
A paper was prepared and submitted for publication in Klinische Wochenschrift. This article, entitled “Die Sondierung des rechten Herzens” (“Catheterisation of the right heart”), was published in November 1929 [1111. Forssmann W. Die Sondierung des rechten Herzens. Klin. Wschr. 1929;8:2085. ].
Forssmann cited as additional objectives the possibility of using the method for diagnostic studies of the heart but he did not specify these.
Based on this publication, Ernst Unger from Berlin accused Forssmann of plagiarism, because of prior intra-arterial drug injections performed in 1912. However, the chief editor of the Klinische Wochenschrift had searched the medical literature and backed Forssmann’s authenticity.
Schneider tried to obtain a position for Forssmann at the Berlin School of Medicine. He first recommended him to Wilhelm His, suggesting that Forssmann perform intracardiac electrocardiographic studies. His refused. Later, Forssmann was successfully recommended to Ferdinand Sauerbruch, the head of the surgical department at the Charité Hospital in Berlin. Forssmann moved to Berlin with the hope of an academic career and he took an unpaid job in October 1929. He found little support but plenty of hostility in this institution. When, one month later, the seminal paper was published, Sauerbruch fired him instantly, proclaiming that “he could lecture in a circus but never at a respectable German university”. He was allowed to return to Eberswalde where he continued his work. He carried out at least six (some recall nine) additional self-catheterisations. He studied direct injection of contrast medium (Uroselectan 40%) through a cardiac catheter positioned in the right atrium initially in rabbits and later in dogs. Many years later, he admitted that, if he had started with experiments in rabbits, he would never have tried it on himself. These studies were reported in the Münchener Medizinische Wochenschrift in 1931. In that year, Sauerbruch asked him to return to Berlin where he stayed until 1932 when he moved to the Städtisches Krankenhaus in Mainz. Later, he started a career as a urologist at the Rudolf-Virchow-Krankenhaus in Berlin. After World War II, he continued as a urologist in Bad Kreuznach. In October 1956, he was awarded the Nobel Prize in Medicine or Physiology jointly with André Cournand and Dickinson Richards. The comments of Prof. Liljestrand at the presentation of the Prize speak for themselves: “It is true that the method was adopted in a few places, but on the whole Forssmann was not given the necessary support: he was, on the contrary, subjected to criticisms of such severity that it robbed him of any inclination to continue. A contributory cause in this instance was presumably that Forssmann was working in a milieu that did not clearly grasp the great value of his idea”.
Finally, the Medical Faculty of the University of Mainz granted Forssmann the position of honorary professor. He died on June 1, 1979.
Several applications of Forssmann’s technique were launched in a variety of countries.
In 1930, Jimenez Diaz and Cuenca described a successful attempt to introduce an ureteral catheter through a cannula (a first introducer sheath) into the arm vein of a moribund patient and suggested many possible utilisations of this technique: sampling of mixed venous blood for determination and comparison with peripheral venous blood of different substances such as glucose or lactic acid, measurement of atrial pressure, or injection of contrast medium for visualisation of the pulmonary circulation.
On August 1, 1930, Otto Klein reported the first measurements of cardiac output in humans on whom he had performed cardiac catheterisations [1212. Klein O. Zur Bestimmung des zirkulatorischen Minutenvolumens nach dem Fickschen Prinzip. Münch Med Wochenschr. 1930;77:1311. ]. Klein ( Figure 8 ) was born in Pilsen in 1891. He graduated from the German University of Prague. The work was performed when he was “Privat Dozent” (assistant professor) at the Second German University Clinic of Prague.
In this paper, he provides many details concerning the catheterisation procedure: the size of the catheter, the site of introduction into a medial vein instead of a lateral vein, the position of the arm during the passage of the catheter into the thorax, how to avoid suction when sampling blood, the discarding of the initial blood withdrawal, and the transfer of the collected blood under oil. Of 18 attempts to introduce a catheter into the heart, 11 cases were successful. In three cases, the Fick principle was applied for the measurement of cardiac output. These measurements were performed in two patients with normal circulation and in one with leukaemia and anaemia. In the first two, “normal” subjects the cardiac output was measured at 4.5 and 5.6 l/min, respectively, whilst it reached 6.9 and 6.7 l/min in the patient with anaemia. In 1939, Otto Klein emigrated to Argentina where he continued to work at the Durand Hospital in Buenos Aires. He died in 1968. It went down in history that Werner Forssmann was the first to perform therapeutic while Otto Klein was the first to perform diagnostic catheterisation of the heart.
In 1932, Padilla, Cossio and Berconsky at the University of Buenos Aires published a series of four papers on cardiac catheterisation. The first reported the technique, the second was related to the identification of the superior vena cava, and the third was on cardiac output. They listed a number of possible applications in the fourth.
From 1932 to 1935, activities concerning the techniques of cardiac catheterisation slackened off slightly, although there were several publications about pulmonary angiography in Portugal, Latin America and France. The next step was the discovery of clinical cardiopulmonary physiology with the work of André Cournand.
André Cournand ( Figure 9 ) was born in Paris on September 24, 1895. His medical studies were interrupted by World War I. He became an intern in 1924. From 1924 to 1930, he published several papers in different medical areas as (co-)author, from the use of intracardiac adrenalin in the resuscitation of young children to blood transfusion for bleeding in typhoid fever.
In 1930, he moved to the USA and worked for 4 months at the Trudeau Sanatorium of Saranac Lake before taking up a position as resident in the Chest and Tuberculosis Service directed by James A. Miller at Bellevue Hospital, Columbia Division, in New York.
André Cournand was chief resident when he was asked by Miller in 1932 to create a small unit for the study of pulmonary function. He started to work with the American physician Dickinson W. Richards and they decided to perform a systematic and comprehensive examination of cardiopulmonary function. Their working hypothesis was based on a proposal by Lawrence Henderson: “the lungs, heart and circulation form a single system for the exchange of respiratory gases between the atmosphere and the tissues of the organism”. In 1936, they considered whether right heart catheterisation might provide help in getting the mixed venous blood needed for determination of respiratory gas concentration.
Cournand went to Paris and visited G. Ameuille who had already performed more than a hundred pulmonary angiograms [1313. Ameuille G, Ronneaux G, Hinauet V, Degrez V, Lemoine J. Remarques sur quelques d’arteriographies pulmonaires chez l’homme vivant. Bull Mem Soc Med Hop Paris. 1935;60:729. ]. Convinced of the safety of this technique, Cournand and Richards started a series of experiments in dogs and in a chimpanzee. They adapted the methodology described by George Wright who had advanced ureteral catheters under fluoroscopic control into the right atrium of cadavers and correlated the catheter tip to a mark on the anterior chest wall on a lateral x-ray projection. In 1940, their first attempts on a patient failed because the catheter could not advance through an axillary vein compressed by large metastatic lymph nodes.
In 1941, they reported on cardiac output measurements (32 patients) comparing the Fick and the ballistocardiographic methods [1414. Cournand A, Ranges H. Catheterization of the right auricle in man. Proc Soc Exp Biol Med. 1941;46:462-466. ]. This report stressed several points: the need for a metabolically stable patient, the need for simultaneous and prolonged blood and air measurements, the reproducibility of the results and the safety of the procedure. Between 1941 and 1945, Cournand and Richards published a number of technical advances [1414. Cournand A, Ranges H. Catheterization of the right auricle in man. Proc Soc Exp Biol Med. 1941;46:462-466. , 1515. Cournand A. Some aspects of the pulmonary circulation in normal man and in chronic cardiopulmonary diseases. Circulation. 1950;2:641-657. , 1616. Cournand A. Cardio-pulmonary function in chronic pulmonary disease. Harvey Lect. 1950-1951; Series 46:68-97. , 1717. Cournand A. Newer methods in the diagnosis of congenital cardiac anomalies Bull N Y Acad Med. 1951;27:277-294. , 1818. Cournand A. A discussion of the concept of cardiac failure in the light of recent physiology studies in man. Ann Intern Med. 1952;37:649-663. , 1919. Cournand A. Dickinson Woodruff Richards, 1895-1973. Trans Assoc Am Physicians. 1973;86:33-38. , 2020. Cournand A. Cardiac catheterization; development of the technique, its constributions to experimental medicine, and its initial applications in man. Acta Med Scand Suppl. 1975;579:3-32. , 2121. Cournand A. The code of the scientist and its relationship to ethics. Science. 1977;198:699-705. , 2222. Cournand A. Historical details of Claude Bernard’s invention of a technique for measuring the temperature and the pressure of the blood within the cavities of the heart. Trans N Y Acad Sci. 1980;39:1-14. , 2323. Cournand A. Origin and historical development of clinical physiology in pulmonary disease. Bull Eur Physiopathol Respir. 1985;21:205-214. , 2424. Cournand A, Donato L, Durand J, Rochester DF, Parker JO, Harvey RM, Lewis ML. Separate performance of both ventricles in man during the early phase of exercise, as analyzed by the method of selective radiocardiography. Trans Assoc Am Physicians. 1960;73:283-296. , 2525. Cournand A, Ferrer MI, Harvey RM, Richards DW. Cardiocirculatory studies in pulsus alternans of the systemic and pulmonary circulation. Circulation. 1956;14:163-174. , 2626. Cournand A, Fritts HW Jr, Harris P, Himmelstein A. Preliminary observations on the effects in man of continuous perfusion with acetylcholine of one branch of the pulmonary artery upon the homolateral pulmonary blood flow. Trans Assoc Am Physicians. 1956;69:163-170. , 2727. Cournand A, Richards DW Jr, Bader RA, Bader ME, Fishman AP. The oxygen cost of breathing. Trans Assoc Am Physicians. 1954;67:162-173. , 2828. Cournand AF. Pulmonary circulation; its control in man, with some remarks on methodology Am Heart J. 1957;54:172-181. , 2929. Cournand AF. Applications of prospective thinking and method to medical education: the initial results of a practical experiment. Stud Gen. 1971;24:1405-1418. , 3030. Cournand AF. Dickinson Woodruff Richards: 1895- 1973. A survey of his contributions to the physiology and physiopathology of respiration in man. Am J Med. 1974;57:312-328. , 3131. Cournand AF, Zuckermann H. The code of science. Analysis and some refl ections on its future. Stud Gen. 1970;23:941-962. ]: a new catheter to facilitate intracardiac manipulation, a new pressure recorder with a Hamilton manometer and a console including an electrocardiograph. All these improvements resulted in better, safer and more reliabile intracardiac recordings.
They subsequently (1942) advanced the catheter tip into the right ventricle and two years later into the pulmonary artery. A new double lumen catheter was designed for simultaneous blood sampling and pressure recording in the right atrium and ventricle or in the right ventricle and pulmonary artery.
From 1942 to 1944, the two pioneers studied different forms of haemodynamic shock with a complete analysis of mechanisms and effects of different treatments. More than 100 cases were studied with intracardiac and arterial blood pressures, cardiac output, blood volume, respiratory gas exchanges, blood gases and pH, and, in some cases, renal blood flow. These elegant studies were reported in a series of papers.
In the midst of World War II, Sir John McMichael, who by 1942 had become aware of Cournand’s latest publication, introduced cardiac catheterisation in England and started to study shock, vasovagal syndrome and heart failure. He was the first to study the effects of intravenous digoxin.
In France, Jean Lenègre and Pierre Maurice started to perform cardiac catheterisation in occupied Paris. They were unaware of the pioneering work of Cournand in the USA and McMichael in London. Nevertheless, Lenègre proposed to Maurice the following topic for his Medical Doctor thesis: “The right ventricular pressure in man (normal and diseased)”. They started with very basic material, including tapered rubber catheters with three distal holes. They used a vertical fluoroscopy system requiring frequent transfer of the patient from the bed to the vertical x-ray device. Catheters were connected to a Claude manometer and were filled with citrate solution. Despite their primitive equipment they were able to describe pressure curves, their normal values and their changes in various forms of acquired or congenital heart disease. Maurice defended his thesis in 1946. The document comprises a complete description of right heart catheterisation, the choice of the brachial vein, and the technical difficulties [3232. Lenègre J, Maurice P. Premières recherches sur la pression ventriculaire droite. Bull Mem Soc Med Hop Paris. 1944;80:239. ]. Maurice and Lenègre were also the first to record an endocardial electrocardiogram in the right ventricle [3333. Lenègre J, Maurice P. La dérivation directe intracavitaire des courants électriques de l’oreillette et du ventricule droit. Paris Méd. 1945;35:23. ]. They studied the origin of ventricular extrasystoles, bundle branch blocks and, later, septal activation. Lenègre and Maurice published the first x-ray picture of a catheter residing in the pulmonary artery.
In 1946 and 1947, Dexter et al published studies performed on patients with congenital heart disease. They reported the results of pressure and oxygen content in the right heart cavities and the oxygen content of “pulmonary capillary” blood. They were the first to record pulmonary wedge pressure by wedging the tip of the catheter in the distal part of a pulmonary artery branch where they also measured oxygen saturation of the blood.
In the Nobel Lecture 1956, also speaking on behalf of Cournand and Richards, Forssmann stated “So besides the epoch of cellular and humoral pathology and many others, we can now, perhaps, speak of an age of cardiological and circulatory investigation”.
In the following years, numerous improvements occurred in the procedure and specific tools were created. In 1947, a synthetic polymer (polyethylene) replaced rubber. The company USCI provided new catheters with different diameters, i.e., 6, 7, 8, and 9 Fr. The term “French” was introduced by English scientists ill at ease with the pronunciation and spelling of the original “Charrière” (1 Charrière = 0.33 mm) unit.
Later, new catheters made from standard radiopaque woven Dacron were used. A French company (TELCO) manufactured specific tools designed for heart catheterisation. Similar tools were manufactured by Sanborn in the United States. A Statham strain gauge called P23DB (Statham Laboratories Inc., Hato Rey, Puerto Rico) was used in the 1970s.
Later on, concerns regarding the quality of pressure recordings were obviated by using electronic tip micromanometers. It was considered that most of the problems (oscillation, damping, transmission delay) with fluid-filled catheters could be solved if a tiny manometer was placed at the tip of the catheter. However, building such a device was quite a challenge. Gauer and Gienapp in the USA, Verhagen and Palm in the Netherlands and Yamakawa in Japan addressed this problem. In 1949, Allard and Laurens, two engineers, started to build a high-frequency tip micromanometer at Pierre Soulié’s department of cardiology in Paris. In 1954, at the second World Congress of Cardiology in Washington, Pierre Soulié and Paul Laurens showed the first experimental results. Further developments and human applications were performed by F. Bouchard and J. Forman. This technique offered the advantages of recording high-sensitivity and high-fidelity curves at the tip of the catheter without any delay, as well as heart sounds inside the heart chambers. Later, the micromanometer of Allard and Laurens was replaced by the tip micromanometer of Millar.
The next period starting at the end of the 1950s was characterised by the development of cine-angiography and, in particular, coronary angiography.
CORONARY ANGIOGRAPHY
Indirect visualisation of the coronary arteries during injection into the ascending aorta had been popular since a publication of G. Jonsson in 1949 [3434. Jonsson G. Thoracic aortography by means of a cannula inserted percutaneously into the common carotid artery. Acta Radiol. 1949;31:376-386. , 3535. Di Guglielmo L, Guttadauro M. Radiological visualization of the coronary arteries in vivo; review of 413 cases. Radiol Med. 1954;40:945-975. ]. For better visualisation, Charles Dotter suggested occluding the ascending aorta with a balloon during injection [3636. Dotter CT, Frische LH. Visualization of the coronary circulation by occlusion aortography: a practical method. Radiology. 1958;71:502-524. ] or temporarily arresting the heart [3737. Dotter CT, Frische LH, W.S. H, Kawashima E, Phillips RW. Coronary arteriography during induced cardiac arrest and aortic occlusion. Arch Intern Med. 1959;104:720-729. ]. Sven Paulin suggested a catheter with a horizontal corkscrew tip to improve opacification of the sinus of Valsalva [3838. Paulin S. Coronary angiography. A technical, anatomic and clinical study. Acta Radiol Diagn (Stockh). 1964;Suppl 223:1+. ].
In 1957, Arnulf proposed the introduction of the contrast medium via a long needle introduced by punction of the aortic root behind the left clavicle. When the needle was in the lumen of the aorta, acetylcholine was intravenously injected and, as soon as the asystole was observed, the contrast medium was injected and a series of images were obtained. Another method which was widely applied was the Nordenström technique. The principle behind this technique was to get a transient increase of the intra-bronchial pressure inducing bradycardia and an important hypotension, then the dye was injected and filled the coronary arteries.
Selective coronary angiography described by Mason Sones ( Figure 10 ) on October 30, 1958, ushered in the modern era of cardiac catheterisation [3939. Sones F, Shirey E, Proudfi t W, Wescott R. Cine coronary arteriography. Circulation. 1959;20:773-774. ]. Standing in a recess underneath the catheterisation table, he witnessed a catheter used for a supravalvular aortic injection slipping into the proximal coronary artery and producing the first selective coronary angiogram.
The initial Sones catheter used for that purpose resembled the Cournand catheter. Kurt Amplatz ( Figure 11 ) added a secondary curve, improving its performance [4040. Amplatz K. Technics of coronary arteriography Circulation. 1963;27:101-106. ]. In 1967, Melvin Judkins ( Figure 12 ) published his femoral
approach [4141. Judkins MP. Selective coronary arteriography. Radiology. 1967;89:815-824. ] (based on Sven Seldinger's ( Figure 13 ) technique [4242. Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39:368-376. ]) using 2 characteristic catheter curves for the left and right coronary arteries respectively.
The coronary arteries soon became the most frequently examined vessels, using mainly preshaped femoral catheters by Judkins, but also those by Bourassa, Schoonmaker, King, El Gamal and many others.
LEFT HEART CATHETERISATION
The development of selective coronary angiography was heightened by advances in vascular access techniques and pre-shaped catheters.
Retrograde aortic approach
In the late 1950s, left heart catheterisation was performed through a cut-down approach at the brachial artery popularised by Sones [3939. Sones F, Shirey E, Proudfi t W, Wescott R. Cine coronary arteriography. Circulation. 1959;20:773-774. ]. The respective catheters were modifications of those of Cournand and were named Sones, Eppendorf, Lehman or NIH catheters. The percutaneous transfemoral approach emerged in the mid 1960s as the most popular method for left heart catheterisation. In 1953, Sven Seldinger ( Figure 13 ), working at the Karolinska Institute in Stockholm, had introduced a technique for percutaneous arterial puncture and catheter substitution of the needle over a flexible guidewire [4242. Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39:368-376. ]. However, for several reasons, however, retrograde left heart catheterisation using the percutaneous femoral approach did not become popular until almost a decade later. The percutaneous transfemoral approach was first introduced in 1962 by Ricketts and Abrams in a small series of patients. In 1967, both Amplatz ( Figure 11 ) and Judkins [4343. Judkins MP. Description of selective coronary angiography with pre-shaped catheters that popularuzed the technique. Radiology. 1967;89:815-824. ] ( Figure 12 ) demonstrated the feasibilty of a percutaneous femoral approach in a larger series of cases.
In the case of aortic stenosis, left ventricular cannulation remained a challenge. Techniques for entering the left side of the heart included left atrial suprasternal, posterior transthoracic and transbronchial punctures, as well as direct left ventricular puncture.
The transseptal approach
John Ross observed that it was easy to cross an atrial septal defect (ASD) to enter the left ventricle. However, in the absence of an ASD, this required a puncture of the interatrial septum. He used a long needle with a curved tip in a dog. He observed that it was relatively easy to pass this needle upward through a catheter positioned in the right atrium via the femoral vein, to rotate the catheter tip against the interatrial septum with the needle withdrawn, and then to enter the left atrium by pushing the needle forward through the septum. The position of the needle tip was then verified by an angiogram with left atrial injection of contrast medium. A series of animal studies followed, with passage of a small plastic catheter through the needle to enter the left ventricle. Later post-mortem studies of the animals demonstrated healing of the puncture site. This work was presented at a surgical meeting in 1958 and published the following year. Then Ross started clinical studies and asked Beckton, Dickinson and Company to manufacture the needle. He finally performed the first transseptal catheterisation on a young man [4444. Ross J Jr. Transseptal left heart catheterization: A new method of left atrial puncture. Ann Surg. 1959;149:395-401. ].
The radial approach
Based on the description of thoracic angiography through the radial artery published in 1948 by Stig Radner [4545. Radner S. Thoracal aortography by catheterization from the radial artery; preliminary report of a new technique. Acta Radiol. 1948;29:178-180. ], in 1974 Michel Bertrand et al [4646. Bertrand M, Ketelers J, Carre A, Ginestet A, Lemaire P, Warembourg H. Une nouvelle voie d’abord des cavités cardiaques gauches utilisant l’artère radiale au dessous du pli du coude. Coeur et Médecine Interne. 1974;13:345-346. ] proposed the use of the radial artery for coronary angiography and left ventriculography, approaching it through an incision below the elbow and ligating it after the procedure. In 1992, Ferdinand Kiemeneij introduced the percutaneous radial approach which is now largely used in Europe and elsewhere. It became popular thanks to the efforts of Hamon and McFadden [4747. Hamon M, McFadden E, eds. Transradial approach for cardiovascular interventions. ESM Editor. 2010. ].
RIGHT HEART CATHETERISATION AT THE BEDSIDE
The need for x-ray guidance confined the practice of cardiac catheterisation to rooms equipped with an image intensifier. Therefore, it had to be accepted until 1965 that right heart catheterisation was impossible in several specific situations
such as shock, recent myocardial infarction, and the early postoperative period after cardiac surgery: these were typical situations in which precise haemodynamic measurements would have been very useful.
An initial but incomplete approach was the use of very small catheters capable of being introduced through a needle thus avoiding surgical cutdown and sacrifice of the vessel.
Théodor Grandjean proposed the use of very flexible tubes. The polyethylene tubes manufactured by Clay-Adams provided the required characteristics: excellent flexibility, easy withdrawal of blood samples and easy introduction through the lumen of a needle (18 gauge). Connected to a standard strain gauge, this probe provided accurate pressure curves without harmonic distortion.
The procedure of microcatheterisation initiated by Grandjean [4848. Grandjean T. A microtechnic of right heart catheterization useful at the bedside without fluoroscopic monitoring. Cardiology. 1967;51:184-192. ] was remarkably simple, easy and fast. He made broad use of this technique combined with an exercise test for the evaluation of left heart disease, such as valvular, but also ischaemic heart disease, particularly after an acute myocardial infarction. In the early 1960s catheterisation of the right heart at the bedside with a microcatheter was certainly a milestone in catheterisation since it replaced a relatively invasive technique performed under x-ray control by a minimally non-invasive technique, without the need for a venous cutdown. This was the “catheterisation laboratory inside the coronary care unit or the surgical theater and resuscitation room”, allowing safe monitoring of the haemodynamic profile of high-risk patients with acute myocardial infarction or in the perioperative period.
Zohman and Williams, as well as Dotter and Bradley had strived since 1959 to replace the semi-rigid Cournand cathcatheter by flexible probes, floating downstream from peripheral venous vessels to the pulmonary artery and avoiding the risk of vascular trauma. Such interventions could be performed without x-ray control.
In 1970, their procedure was replaced by the Swan-Ganz technique which offered numerous advantages ( Figure 14 ). Jeremy Swan made several attempts with a thin catheter but he recognised that the low forward flow velocity was inadequate to carry the catheter into and through a dilated right ventricle. A soft catheter of high flexibility with an effective flotation device such as a sail or parachute at its tip, passed into the pulmonary circulation consistently, rapidly and without catheter manipulation. Single lumen balloon-tipped catheters appeared even more suitable and were produced by Edwards and tested by William Ganz in animals. They were rapidly perfected to double lumen flexible balloon catheters. A small lumen allowed balloon inflation with air, while the larger permitted recording of pressure at the catheter tip. The first such catheter was advanced to the right atrium of a healthy dog. On inflation of the balloon, the catheter disappeared from the fluoroscopic screen, showing a low pressure. Neither right ventricular nor pulmonary artery pressure could account for that. In one systole, the catheter had been transported to a wedge, i.e., the “pulmonary artery occluded” position and had appropriately reflected the pressure in the left atrium. After some additional experiments in animals, Ganz and Marcus used the device for human right heart catheterisation in a standard catheterisation laboratory, with and without fluoroscopy, with equally gratifying results. The effectiveness of right heart and pulmonary artery catheterisation using the balloon catheter without fluoroscopy or catheter manipulation was proved within a week.
Construction and attachment of the balloon were modified to ensure that the catheter tip remained below the inflated balloon surface. The results of the first 100 patients using the double lumen catheter were published in the New England Journal of Medicine on August 27, 1970 [4949. Swan HJ, Ganz W, Forrester J, Marcus H, Diamond G, Chonette D. Right heart catheterisation at the bedside with the later named Swan-Ganz catheter. N Engl J Med. 1970;283:447-451. ], and became one of the most quoted references in the medical literature over the next two years.
In 1971, Grandjean proposed a new technique to reach the left ventricle [5050. Grandjean T. Left heart microcatheterization feasible in the patient’s bed by means of reference marking with continuous endoaortic electrocardioscopy. Arch Mal Coeur Vaiss. 1972;65:1335-1341. ]. It was characterised by intravascular electrocardiographic guidance. The material included a thin guidewire introduced inside the lumen of a thin 3.6 Fr polyethylene catheter. The wire was connected to the precordial electrode of the ECG. The progression and the direction of the catheter were followed by the ECG profiles. Introduced through a needle into the brachial artery, the catheter coming from the subclavian artery arrived into the brachiocephalic trunk and the ascending aorta. In these vessels, the ECG profile was similar to the aVR lead tracing. The amplitude increased as soon as the catheter was getting close to
the aortic valve. Once the catheter crossed the aortic valve, the ECG profile was characterised by a huge QS wave indicating the position in the left ventricle. In cases where the catheter was going in the wrong direction, i.e., down the descending aorta, the ECG profiles became similar to those recorded in the leads aVL and aVF, respectively. Thus, it was possible to follow the trajectory of the microcatheter using ECG guidance. Later, the intravascular ECG found later clinical applications in the realm of percutaneous coronary interventions [5151. Meier B, Rutishauser W. Coronary pacing during percutaneous transluminal coronary angioplasty. Circulation. 1985;71:557-561. ].














Great history . Amazing book . How human generation have been struggling to get to the point where we are today
Special
It is rely great and valuable
It is a great book. I recommend widely
awesome
great book
This book is great !