Summary
Percutaneous closure of paravalvular leak (PVL) is a complex procedure that requires multiple imaging modalities to visualise the three-dimensional relationship of intracardiac structures and the operator’s ability to navigate within 3-dimensional space. Three approaches can be employed in order to cross the defect and deliver the closure device: transseptal, retrograde transaortic, and direct transapical. Despite the big variety of available devices, there are no dedicated devices for paravalvular leak closure. Results of percutaneous closure appear to be superior to surgical outcomes with lower complication rates and higher success rates.
Introduction
Paravalvular leak (PVL) is a regurgitant jet that originates between the outer margin of the prosthetic ring and the native tissues around the valve. It is a well-known complication of valve replacement and has been found to occur in as many as 10% of prosthetic valves in the aortic position [11. Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36:1152-8. , 22. Ionescu A, Fraser AG, Butchart EG. Prevalence and clinical significance of incidental paraprosthetic valvar regurgitation: a prospective study using transoesophageal echocardiography. Heart. 2003;89:1316-21. ] and 17% of prosthetic valves in the mitral position [11. Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36:1152-8. , 22. Ionescu A, Fraser AG, Butchart EG. Prevalence and clinical significance of incidental paraprosthetic valvar regurgitation: a prospective study using transoesophageal echocardiography. Heart. 2003;89:1316-21. , 33. Genoni M, Franzen D, Vogt P, Seifert B, Jenni R, Künzli A, Niederhäuser U, Turina M. Paravalvular leakage after mitral valve replacement: improved long-term survival with aggressive surgery?. Eur J Cardiothorac Surg. 2000;17:14-9. ]. The majority of patients with PVL remain asymptomatic; however, 1% to 5% of patients will present with symptoms. Although surgical management (replacing the dysfunctional valve with a new valve or repairing the paravalvular defect) carries a high mortality and morbidity risk [44. de Almeida Brandão CM, Pomerantzeff PM, Souza LR, Tarasoutchi F, Grimberg M, Ramires JA, Almeida de Oliveira S. Multivariate analysis of risk factors for hospital mortality in valvular reoperations for prosthetic valve dysfunction. Eur J Cardiothorac Surg. 2002;22:922-6.
In this study authors analyse risk factors for hospital mortality in patients undergoing valvular reoperations for prosthetic valve dysfunction, 55. Echevarria JR, Bernal JM, Rabasa JM, Morales D, Revilla Y, Revuelta JM. Reoperation for bioprosthetic valve dysfunction. A decade of clinical experience. Eur J Cardiothorac Surg. 1991;5:523-6; discussion 527. , 66. Expósito V, García-Camarero T, Bernal JM, Arnáiz E, Sarralde A, García I, Berrazueta JR, Revuelta JM. Repeat mitral valve replacement: 30-years’ experience. Rev Esp Cardiol. 2009;62:929-32.
Authors describe outcomes of repeat mitral valve replacement], surgery is considered a gold standard and the American Heart Association (AHA)/American College of Cardiology (ACC) guidelines gave surgery a Class I recommendation in operable patients with mechanical heart valves with intractable haemolysis or heart failure (HF) due to severe paravalvular regurgitation [77. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Jun 10;63(22):2438-88. ]. Percutaneous repair of PVL is reasonable in patients with intractable hemolysis or New York Heart Association (NYHA) Class III/IV HF who are at high risk for surgery and have anatomical features suitable for catheter-based therapy when performed in centers with expertise in the procedure.
Clinical manifestations and indications for closure
Patients with paravalvular leak may present with symptoms of congestive heart failure, haemolysis or, in most cases, a combination of both. Congestive heart failure is a result of volume overload caused by the regurgitation through the paravalvular leak, and it is proportional to the defect size (single or the sum of multiple defects). Haemolysis results from sheer stress on the red blood cells during passage of blood through the paravalvular leak, and does not correlate with the size of the defect. Haemolysis can be significant even with small defects, especially if multiple defects are present. Mechanical haemolytic anaemia that requires blood transfusions or erythropoietin injections to maintain a haemoglobin level over 10 g/dL is another indication for PVL closure. Truly asymptomatic patients should not be considered as candidates for the percutaneous closure because of the small but definite risk of procedural complications.
Nomenclature of anatomical location of paravalvular
For the description of paravalvular leaks an adaptation of the accepted surgical nomenclature can be used [88. De Cicco G, Lorusso R, Colli A, Nicolini F, Fragnito C, Grimaldi T, Borrello B, Budillon AM, Gherli T, Beghi C. Aortic valve periprosthetic leakage: anatomic observations and surgical results. Ann Thorac Surg. 2005;79: 1480-5. , 99. De Cicco G, Russo C, Moreo A, Beghi C, Fucci C, Gerometta P, Lorusso R. Mitral valve periprosthetic leakage: Anatomical observations in 135 patients from a multicentre study. Eur J Cardiothorac Surg. 2006;30:887-91.
Authors analyse anatomical factors that contribute to the occurrence of paravalvular leak after mitral valve replacement]. Each valve can be compared to a clock, so there are two clocks horizontally inverted one to another: one is in the aortic valve position and the other in the mitral valve position as seen from a cephalad position. The 12 o’clock in both clocks corresponds to the mitral-aortic fibrous continuity, and from there each location is named in a clockwise fashion ( Figure 1 ).
For the aortic valve, the left coronary cusp is located between 11 and 3 o’clock, the right coronary cusp between 3 and 7 o’clock, and the non-coronary cusp between 7 and 11 o’clock. The highest rate of PVLs, is found at the right coronary cusp (between 7 and 11 o’clock), which corresponds to the membranous septum and the right trigone [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up].
For the mitral valve, the 3 o’clock corresponds to the area of the interatrial septum, the 6 o’clock corresponds to the posterolateral free wall, and the 9 o’clock corresponds to the region of the left atrial appendage (LAA). In one series, mitral PVLs were most frequently located between 10 and 2 o’clock, which corresponds to the mitro-aortic fibrous continuity, and between 6 and 10 o’clock, which corresponds to the posterior wall [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up].
Diagnostic and interventional imaging
The PVL Academic Research Consortium (PVLARC) provided recommendations for the assessment of the disease severity which are summarized in the following sections (Ruiz CE et al. Clinical Trial Principles and Endpoint Definitions of Therapies of Paravalvular Leaks in Surgical Prosthesis: A Consensus Document from the Paravalvular Leak Academic Research Consortium. JACC, In press)
After a baseline transthoracic echocardiogram (TTE) within 1-6 months of surgical valve replacement, further testing is dependent on the presence of PVL and symptoms. Symptomatic PVL should prompt a more extensive investigation including imaging characterization, functional assessment, and hematological/biomarker characterization. Echocardiography remains central to the diagnosis and assessment of PVLs. Various other non-echocardiographic imaging modalities like computed tomographic angiography (CTA), magnetic resonance imaging (MRI), and nuclear studies can aid in characterizing PVLs, assessing the prosthetic valve function, and ruling out active endocarditis. Additionally, biomarkers like high-molecular-weight von Willebrand factor may have a role as a sensor of PVL following valve surgery [1212. Van Belle E, Rauch A, Vincentelli A, Jeanpierre E, Legendre P, Juthier F, Hurt C, Banfi C, Rousse N, Godier A, Caron C, Elkalioubie A, Corseaux D, Dupont A, Zawadzki C, Delhaye C, Mouquet F, Schurtz G, Deplanque D, Chinetti G, Staels B, Goudemand J, Jude B, Lenting PJ, Susen S. Von Willebrand factor as a biological sensor of blood flow to monitor percutaneous aortic valve interventions. Circ Res. 2015 Mar 27;116(7):1193-201. ].
ECHOCARDIOGRAPHY
Evaluation:
TTE can be used to assess chamber sizes and function, transvalvular gradients. Transesophageal echocardiography (TOE) can be used to evaluate PVL better but is limited by the need for conscious sedation or anesthesia. The comprehensive qualitative and quantitative evaluation of PVL should combine the 2-dimentional (2D), 3-dimensional (3D), pulse and continuous wave Doppler, and 2D/3D color-Doppler modalities.
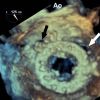
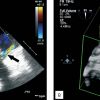
The 3D Echo modalities (Live 3D, real-time 3D zoom, full volume etc.) provide useful information about the exact location of the valvular dehiscence, its size and its shape ( Figure 2 , Moving image 1 ). The 3D full volume modality with colour flow imaging further confirms the leak ( Figure 3 ), can distinguish between paravalvular and valvular jets, and defines the severity of the regurgitation. Special attention is paid to potential contraindication to PVL closure such as intracavitary clots or severe transvalvular regurgitation. The PVLARC group proposed echo criteria to assess the severity of PVL as below.
Mild aortic and mitral PVL: Primary criteria - 1) Normal sewing ring motion, 2) Jet features: narrow jet width, infrequently multiple, no proximal flow convergence, 3) % LVOT diameter <30%, and 4) Circumferential extent <10%. Secondary criteria – 1) Normal left ventricular (LV) size, 2) Vena contracta width <4 mm, 2) Incomplete or faint spectral Doppler, 3) PHT >500 msec, and 4) Diastolic flow reversal is absent or brief. Quantitative criteria – 1) RVol <30 mL, 2) RF <30%, and 3) EROA <0.1 cm2.
Severe aortic and mitral PVL: Primary criteria - 1) Sewing ring motion abnormality, 2) Jet features: wide jet width, frequently multiple, proximal flow convergence, 3) % LVOT diameter ≥60%, and 4) Circumferential extent ≥30%. Secondary criteria – 1) Moderate to severely dilated LV, 2) Vena contracta width ≥6 mm, 2) Dense spectral Doppler, 3) PHT <200 msec, and 4) Holodiastolic flow reversal (end-diastolic velocity >20-30 cm/s). Quantitative criteria – 1) RVol ≥60 mL, 2) RF ≥50%, and 3) EROA ≥0.3 cm2.
Intraprocedure: continuous 2D and 3D TOE monitoring is performed. The location of the PVL is reassessed. The operator uses the 2D and 3D TOE images to plan the approach to the PVL and to select the optimal device for closure. The real-time 3D TOE demonstrates the entire intracardiac portion of the catheters and closure device(s). Thus, the anatomical relations between the catheter tip, the device and the cardiac structures are evaluated in real time ( Figure 4 ).
In most cases, images of the valves are arranged in the “surgical view” to facilitate standardisation of the images and to create better communication between the imaging specialist and the operator. If required, the transseptal needle position is monitored for site specific puncture to facilitate crossing of the defect.
The tip of the catheter can be followed and guided into the dehiscence site. After the device is deployed in a satisfactory position (before its release) a careful evaluation of the valve gradient and the degree of PVL and transvalvular regurgitation is again performed to ascertain no interference of the closure device with prosthetic valve function. In case of newly created valvular stenosis or regurgitation, the device should be repositioned or removed. Large residual PVL may call for either a larger device or multiple simultaneously deployed devices. The last of these is our preferred approach.
The role of echocardiography during the procedure
- Real time confirmation of defect crossing with guidewire or delivery sheath
- Ruling out interference of closure device with prosthetic valve function
- Accurately detect and quantify residual leaks
- Excellent tool for site specific puncture
Post procedure: immediately post procedure (and before the TOE probe removal) a screening for possible procedure-related complications is obtained. These include evaluation of possible new effusion (pericardial and/or pleural), puncture-related new atrial septal defects and intracardiac clots. Follow-up TTE is performed routinely within 24 hours.
COMPUTED TOMOGRAPHIC ANGIOGRAPHY
Assessment of dynamic anatomical interrelations is critical in the evaluation process of percutaneous interventions. Therefore, reviewing the anatomy using 3D/4D volume-rendered post-processing images should be mandatory. In a Structural Heart Disease centre, all patients with known paravalvular leak (leaks) should undergo cardiac computed tomographic angiography (CTA), as it plays an important role in the delineation of the defects and the planning of the procedure.
Scanning protocol: a recommended protocol uses helical scan acquisition with retrospective ECG-gated 16-phase reconstruction with 6.25% increments from R-R interval. 70 to 120 ml of contrast media is administered through the antecubital or femoral vein at the rate of 4-6 mls /second. Acquisition delay time is determined by a bolus tracking protocol.
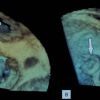
Post-processing: the 3D volume rendering of single phase provides valuable information about the entire thoracic and cardiac anatomy. It also allows a detailed description of the structural defect including location, shape, size and number of the defects ( Figure 5A ). The 4D volume rendering, where the fourth dimension is a time factor, provides the opportunity to observe dynamic changes throughout the cardiac cycle and the assessment of prosthetic valve and ventricular function
( Moving image 2 ). This way of reviewing cardiac anatomy is important to predict challenges that may occur during the procedure depending on the chosen access approach, closure device size, and deployment technique. When planning a transapical approach, the direct LV access site is chosen from the post-processed CTA images to enter the LV through the anterior wall, away from the apex, and at the most perpendicular plane to the defect. Attention is paid to avoid puncturing through lung tissue and epicardial coronary arteries ( Figure 6 ).
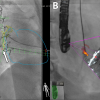
Intra procedure: 4D CTA reconstructed images can be used to facilitate the crossing of the defect. The CTA images are displayed side-by-side to the fluoroscopy image, using a greyscale preset that can be called “fluoro-like” because of its similarities with the live fluoroscopy image. The PVL(s) is marked with a target landmark which remains at the same 3D location regardless of image orientation ( Figure 7 ). The reconstructed images are rotated and angulated according to the movement of the fluoroscopy image intensifier, allowing the CTA and the fluoroscopy images to be congruent throughout the procedure. The 4D images can also be used to determine the most useful fluoroscopic view for best visualisation of the defect that can be reproduced by the image intensifier.
The role of the CTA
- Best imaging tool for planning of the access and precise location of the defects
- CTA overlay facilitates defect crossing and can be used for the transapical puncture
- The CTA is not a real time and therefore has no value in device positioning
Post procedure: a follow-up CTA is performed to confirm the device position and screening for possible procedure-related complications within 24 hours after the procedure ( Figure 5, Moving image 3 ).
Fusion Imaging: Fluoroscopy still remains the main imaging modality used for procedures in the catheterisation lab. Limitations of fluoroscopy in delineation of soft tissues and 3D anatomy, however, are well known. Advancements in technology may allow overcoming current limitations. Recently developed fusion imaging allows combining imaging datasets from different sources into the one image, providing an additive benefit of each modality ( Figure 8 ).
The fusion of CT images with fluoroscopy is done using a dedicated imaging workstation (HeartNavigator, Philips, Netherlands) that segments previously acquired CT scan to create a 3D model of the chest structures and overlays it over the fluoroscopy screen. At the beginning of the procedure the 3D model is co-registered with live fluoroscopy and from that point the overlaid image is congruent throughout the procedure, providing a 3D navigation.
The fusion of TOE with fluoroscopy is done by registering the TOE probe. This allows projecting the dataset acquired by the TOE probe onto the fluoroscopy image. Being the real time, the fusion of echo-fluoroscopy provides a real time feedback information and may overcome limitations encountered with CT-fluoroscopy fusion imaging: changes in patient position and volume status and cardiac movement from respiration and contraction.
Both technologies are at an early stage of development but results are promising.
Interventional techniques
There are three potential approaches to left-sided paravalvular leaks: (1) retrograde, (2) transseptal, and (3) transapical, with the approach chosen depending on the location of the leak. All procedures are meticulously pre-planned utilising 4D CTA reconstruction and are monitored with 3D TOE intraoperatively.
1) Retrograde approach. The retrograde approach is typically utilised for closing aortic paravalvular leaks. Following routine arterial access, the aortic leak is approached with a catheter directed towards the defect. The defect is crossed with a straight or angled hydrophilic guidewire with the catheter then passed over the wire and across the leak. The hydrophilic guidewire is then exchanged for a heavy-duty extra-support wire (Lunderquist™ Extra Stiff Wire; Cook Medical Inc., Bloomington, IN, USA) over which is placed a hydrophilic delivery sheath (Shuttle®-SL 90 cm; Cook Medical Inc.). With Amplatzer type devices, the distal disc is then deployed in the ventricle and anchored within the defect. Prior to the release of the device, meticulous attention must be paid to the prosthetic valve to ensure that there is no interference with valve function. Such interference is invariably accompanied by haemodynamic compromise. The retrograde approach is most applicable for aortic paravalvular leaks but may also be utilised for mitral paravalvular leaks closure for defects located between 10 and 1 o’clock. If additional support is required to advance the delivery sheath through the defect, an arterial-venous rail may be established using an exchange glidewire that is snared in the aorta and exteriorised through a sheath in the femoral artery ( Figure 9 ).
2) Transseptal approach. The transseptal approach is typically utilised for mitral PVL between six and eleven o’clock. Access to the left atrium is achieved by the standard transseptal technique that has been described previously [1313. Brockenbrough E, Braunwald E. A new technique for left ventricular angiography and transseptal left heart catheterization. Am J Cardiol. 1960;6:219-31.
Authors describe a new percutaneous approach for closure of mitral paravalvular leaks via transapical puncture]. Once a transseptal sheath is placed in the left atrium, the mitral paravalvular leak may be crossed with a hydrophilic guidewire guided by a pre-shaped catheter or a moveable tip catheter. After the defect has been crossed with the catheter into the left ventricle, the glidewire is exchanged for an extra-support wire such as an Amplatz Super Stiff Wire (Boston Scientific, Natick, MA, USA) or a Lunderquist Extra Stiff Wire (Cook Medical Inc.). If this does not provide sufficient support to advance the delivery sheath, an arterial-venous rail can be used ( Illustrative case 1 ).
3) Transapical approach. The transapical approach is typically chosen for mitral paravalvular leaks between eleven and six o’clock to avoid complications associated with excessive forces on the septal wall from the delivery catheter that may result in a septal tear due to the sharp angle required to cross the defect. The precise site on the chest wall of the transapical puncture that is perpendicular to the plane of the prosthetic valve is planned utilising 4D CTA. In the majority of cases this is on the anterior wall of the LV between the two papillary muscles and away from any major epicardial vessel. A 21-gauge micropuncture needle and a 0.018 inch guidewire are used to enter the left ventricle and to place a 5 Fr sheath. The paravalvular leak may then be crossed retrograde typically using a Berenstein catheter (AngioDynamics, Queensbury, NY, USA) and an angled or straight 0.035 inch glidewire. After the catheter is placed in the left atrium, the glidewire is exchanged for an extra-support wire, typically the Inoue wire (Toray International America Inc., Houston, TX, USA). An appropriately sized delivery sheath is advanced over the guidewire and across the defect and an Amplatzer occlusive device is placed as noted above. Again, prior to release of the device, particular attention should be paid to the prosthetic valve to be certain there is no interference with valvular function. If this is the case, the device cannot be deployed and should be removed. Once the defect has been closed, the delivery sheath is removed and the transapical puncture site typically closed with an Amplatzer 6/4 mm ADO device (AGA Medical Corporation, Golden Valley, MN, USA). In one reported experience now consisting of over 30 cases of transapical approach using delivery systems of up to 12 Fr for closure of mitral PVL, this approach has resulted in a significant decrease in fluoroscopic and overall procedural time without major risk of procedural complications [1414. Jelnin V, Dudiy Y, Einhorn BN, Kronzon I, Cohen HA, Ruiz CE. Clinical experience with percutaneous left ventricular transapical access for interventions in structural heart defects a safe access and secure exit. JACC Cardiovasc Interv. 2011;4:868-74. ] ( Illustrative case 2 ).
Hopscotch technique
Small and round PVLs may be closed with a single device. Most of the PVLs, however, are crescent shaped, and to adequately close these defects several closure devices are frequently needed. The delivery of subsequent devices can be challenging because of the risk of dislodgment of the previously deployed device and often times the presence of an intact suture line or tissue within the PVL. In such instances, a ‘hopscotch’ technique can be of help. With this approach, once the first device is positioned across the defect and before it is released, the adjacent PVL is crossed with the guidewire advanced through the same delivery sheath. Then first device is released and the second device is delivered. This process may be iterated until adequate closure is obtained.
Selection of approach for mitral paravalvular leak closure
- Transseptal approach for leaks located at 6-11 o’clock
- Retrograde approach for leaks located at 10-1 o’clock
- Transapical approach for leaks located at 11-6 o’clock
Available devices
The Rashkind double umbrella device (USCI Angiographics, Billerica, MA, USA) was used for the first cases of percutaneous closure of the PVL by Hourihan et al [1515. Hourihan M, Perry SB, Mandell VS, Keane JF, Rome JJ, Bittl JA, Lock JE. Transcatheter umbrella closure of valvular and paravalvular leaks. J Am Coll Cardiol. 1992;20:1371-7.
First report of percutaneous closure of paravalvular leak]. Since then, there have been reported uses of the CardioSEAL Clamshell device (Nitinol Medical Technologies, Inc., Boston, MA, USA), the AMPLATZER family of devices (AMPLATZER® Septal Occluder or ASO, AMPLATZER® Duct Occluder, AMPLATZER® Muscular Ventricular Septal Defect Occluder or MVSD, AMPLATZER® Vascular Plug [unavailable in the USA] [AGA Medical Corporation, Golden Valley, MN, USA]), vascular occlusion devices and coils (Gianturco; Cook Medical Inc.) [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 1616. Eisenhauer AC, Piemonte TC, Watson PS. Closure of prosthetic paravalvular mitral regurgitation with the Gianturco-Grifka vascular occlusion device. Catheter Cardiovasc Interv. 2001;54:234-8. , 1717. Martinez CA, Rosen R, Cohen H, Ruiz CE. A novel method for closing the percutaneous transapical accesstract using coils and gelatin matrix. J Invasive Cardiol. 2010;22:E107-9. , 1818. Pate G, Webb J, Thompson C, Munt B, Chugh S, Carere R, Moss R. Percutaneous closure of a complex prosthetic mitral paravalvular leak using transesophageal echocardiographic guidance. Can J Cardiol. 2004;20:452-5. , 1919. Piechaud JF. Percutaneous closure of mitral paravalvular leak. J Interv Cardiol. 2003;16:153-5. , 2020. Nietlispach F, Johnson M, Moss RR, Wijesinghe N, Gurvitch R, Tay EL, Thompson C, Webb JG. Transcatheter closure of paravalvular defects using a purpose-specific occluder. JACC Cardiovasc Interv. 2010;3:759-65. ] ( Figure 10 ).
The waist of the ASO (3-4 mm) is shorter than the waist of the MVSD Occluder (7 mm) and the Duct Occluder (5-8 mm). The Duct Occluder and the MVSD are preferred for leaks closer to the valve because the difference between the disc and the waist (5-8 mm) is smaller than for the ASO (up to 12-14 mm)9. The AMPLATZER® Vascular Plug III (unavailable in the USA) is the device which perhaps adapts best to a larger type of defects. Outside the US, the Amplatzer vascular plug III (AVP-III, CE marked in Europe) is an oblong-shaped device that may better conform to crescent or oval shaped PVLs. The AVP-IV consists of two conical-shaped nitinol mesh joined by central articulation.
The fist dedicated device for PVL closure Occlutech PLD (Occlutech GmbH., Jena, Germany) has recently obtained CE marking. This device consists of two discs of square or rectangular shape with wide elliptic or narrow cylindrical waist ( Figure 11).
Procedural and clinical outcomes
Experience with percutaneous closure of paravalvular leaks is still limited. The procedural success rate in currently available series varies from 63% to 95% [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 1515. Hourihan M, Perry SB, Mandell VS, Keane JF, Rome JJ, Bittl JA, Lock JE. Transcatheter umbrella closure of valvular and paravalvular leaks. J Am Coll Cardiol. 1992;20:1371-7.
First report of percutaneous closure of paravalvular leak, 2121. Cortés M, García E, García-Fernandez MA, Gomez JJ, Perez-David E, Fernández-Avilés F. Usefulness of transesophageal echocardiography in percutaneous transcatheter repairs of paravalvular mitral regurgitation. Am J Cardiol. 2008;101:382-6.
The effect of transoesophageal echocardiographic guidance on success of closure of mitral paravalvular leak, 2222. García-Borbolla Fernández R, Sancho Jaldón M, Calle Pérez G, Gómez Menchero AE, de Zayas Rueda R, Arana Granado R, Marante Fuertes E, Cabeza Laínez P. Percutaneous treatment of mitral valve periprosthetic leakage. An alternative to high-risk surgery?. Rev Esp Cardiol. 2009;62:438-41. , 2323. Hein R, Wunderlich N, Robertson G, Wilson N, Sievert H. Catheter closure of paravalvular leak. EuroIntervention. 2006;2:318-25. , 2424. Pate GE, Al Zubaidi A, Chandavimol M, Thompson CR, Munt BI, Webb JG. Percutaneous closure of prosthetic paravalvular leaks: case series and review. Catheter Cardiovasc Interv. 2006;68:528-33.
Review of paravalvular leak closure in series of 21 patients] and is mainly determined by anatomical location of the leak and available closure devices ( Table 1 ). Clinical success can be achieved from 50% to 86% of patients [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 1515. Hourihan M, Perry SB, Mandell VS, Keane JF, Rome JJ, Bittl JA, Lock JE. Transcatheter umbrella closure of valvular and paravalvular leaks. J Am Coll Cardiol. 1992;20:1371-7.
First report of percutaneous closure of paravalvular leak, 2121. Cortés M, García E, García-Fernandez MA, Gomez JJ, Perez-David E, Fernández-Avilés F. Usefulness of transesophageal echocardiography in percutaneous transcatheter repairs of paravalvular mitral regurgitation. Am J Cardiol. 2008;101:382-6.
The effect of transoesophageal echocardiographic guidance on success of closure of mitral paravalvular leak, 2222. García-Borbolla Fernández R, Sancho Jaldón M, Calle Pérez G, Gómez Menchero AE, de Zayas Rueda R, Arana Granado R, Marante Fuertes E, Cabeza Laínez P. Percutaneous treatment of mitral valve periprosthetic leakage. An alternative to high-risk surgery?. Rev Esp Cardiol. 2009;62:438-41. , 2323. Hein R, Wunderlich N, Robertson G, Wilson N, Sievert H. Catheter closure of paravalvular leak. EuroIntervention. 2006;2:318-25. , 2424. Pate GE, Al Zubaidi A, Chandavimol M, Thompson CR, Munt BI, Webb JG. Percutaneous closure of prosthetic paravalvular leaks: case series and review. Catheter Cardiovasc Interv. 2006;68:528-33.
Review of paravalvular leak closure in series of 21 patients]. After the successful closure, symptoms of congestive heart failure usually resolve or improve within the first few weeks. Haemolysis, on the other hand, may continue or even worsen after the closure for the first few months until device endothelisation. Therefore, we recommend waiting at least six months to assess the need for further intervention or surgery.
Sorajja et al [2525. Sorajja P, Cabalka AK, Hagler DJ, Rihal CS. Percutaneous repair of paravalvular prosthetic regurgitation: acute and 30-day outcomes in 115 patients. Circ Cardiovasc Interv. 2011;4:314-21.
Short-term results of paravalvular leak closure in 115 patients] reported experience with percutaneous repair of 141 paravalvular defects in 115 patients. The procedural success rate was 89% with short-term clinical success in 77% of patients. Recently, the same group reported the long-term follow-up in 126 patients with mortality rate of 23% and clinical success in 72% of patients who survived. The most common cause of death was heart failure (37% of deaths); non-cardiac causes accounted for 9 deaths (30% of deaths) [2626. Sorajja P, Cabalka AK, Hagler DJ, Rihal CS. Long-term follow-up of percutaneous repair of paravalvular prosthetic regurgitation. J Am Coll Cardiol. 2011; 58:2218-24.
Long-term outcomes after percutaneous closure of paravalvular leak].
In our recently reported experience on 57 closure attempts of 47 defects (38 mitral and 11 aortic leaks) in 43 consecutive patients, overall procedural success was 86%, and clinical success among patients with a successfully deployed device was 89% with follow-up to 42 months. The 30-day mortality rate was 4.6%, and freedom from cardiac-related death at 18 months was 91.9% [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up]. Compare these results to surgical outcomes of 13%, 15%, and 37% hospital mortality after the first, second and third reoperation, respectively [55. Echevarria JR, Bernal JM, Rabasa JM, Morales D, Revilla Y, Revuelta JM. Reoperation for bioprosthetic valve dysfunction. A decade of clinical experience. Eur J Cardiothorac Surg. 1991;5:523-6; discussion 527. ] and 10-year survival of only 30% [2727. Akins CW, Bitondo JM, Hilgenberg AD, Vlahakes GJ, Madsen JC, MacGillivray TE. Early and late results of the surgical correction of cardiac prostethic perivalvular leaks. J Heart Valve Dis. 2005;14:792-9. ].
Cortés et al [2121. Cortés M, García E, García-Fernandez MA, Gomez JJ, Perez-David E, Fernández-Avilés F. Usefulness of transesophageal echocardiography in percutaneous transcatheter repairs of paravalvular mitral regurgitation. Am J Cardiol. 2008;101:382-6.
The effect of transoesophageal echocardiographic guidance on success of closure of mitral paravalvular leak] presented a series where they analysed the probability of success in relation to the location of the leak, and found that crossing the leak was unsuccessful in 2 of the 3 patients with PVL in the lateral internal region of the ring and in 3 of 6 patients with anterior or lateral external leaks. By contrast, 83% of the leaks in the posterior ring could be successfully closed. Clinical status improved in 59% of the patients with a successfully implanted device. Adverse events were also carefully reported in this series and are presented in Table 1 . One month post procedure, regurgitation grade had improved in 8 of 17 successfully treated patients.
In the series by Pate et al [2424. Pate GE, Al Zubaidi A, Chandavimol M, Thompson CR, Munt BI, Webb JG. Percutaneous closure of prosthetic paravalvular leaks: case series and review. Catheter Cardiovasc Interv. 2006;68:528-33.
Review of paravalvular leak closure in series of 21 patients], complete closure of the PVL was finally achieved in 5 of 10 patients; four patients had required two procedures. Furthermore, despite successful device deployment in two additional patients, residual leak persisted. Similarly, in spite of a success rate of 95% reported in the series by Hein et al [2323. Hein R, Wunderlich N, Robertson G, Wilson N, Sievert H. Catheter closure of paravalvular leak. EuroIntervention. 2006;2:318-25. ], three patients required a second procedure because of residual leak with haemolysis, and significant shunt was reported in 45% of the patients at the end of the observation period (14±12 months). In this same study, during the initial procedure the closure device had to be replaced for a smaller one in five patients due to interference with the valve or device instability.
Noble et al., [2929. Noble S, Jolicoeur EM, Basmadjian A, Levesque S, Nozza A, Potvin J, Crépeau J, Ibrahim R. “Percutaneous paravalvular leak reduction: procedural and long-term clinical outcomes,”. Can J Cardiol. 2013;29:1422-8. ] presented their experience with 56 consecutive patients (44 mitral and 12 aortic PVL) that underwent percutaneous closure. The total technical success was 75.4 %, with 40% (two out of five patients) success rate in patients with significant haemolysis only versus 78.4 % (40 out of 51 patients) in patients when the indication involved heart failure with or without haemolysis. Clinical success with improvement in NYHA functional class and decrease in haemolysis was achieved in 69 % and 54.8% at 3 and 12 months respectively. However, during the follow up period 50 % (21 of 42) patients with a successful PVL closure died with 38% within the first year. Despite this, the group of patients with successful PVL closure performed better compared to unsuccessful closure group in regards of survival, re-hospitalisation and need for surgical re-interventions (HR 0.34, CI 0.17-0.71). The 30 day mortality in patients that underwent successful percutaneous closure of PVL was 4.8 % (2 out of 42 patients). One patient died from embolisation of ADO device from mitral position to mechanical aortic valve causing immediate death and second patient died from retroperitoneal bleeding on day 12.
A meta-analysis by Millan et al., [3030. Millán X, Skaf S, Joseph L, Ruiz CE, García,E, Smolka G, Noble S, Cruz-González I, Arzamendi, D, Serra A, Kliger C, Sia Y, Asgar A, Ibrahim R, Jolicoeur ME, “Transcatheter Reduction of Paravalvular Leaks: A Systematic Review and Meta-analysis,”. Can J Cardiol. In print, doi: 10. 1016/j. cjca. 2014. 12.
Millán X, Skaf S, Joseph L, Ruiz CE, García,E, Smolka G, Noble S, Cruz-González I, Arzamendi, D, Serra A, Kliger C, Sia Y, Asgar A, Ibrahim R, Jolicoeur ME, “Transcatheter Reduction of Paravalvular Leaks: A Systematic Review and Meta-analysis,”. Can J Cardiol. In print, doi: 10.1016/j.cjca.2014.12.012. ] included 12 non-randomised studies with a total of 362 patients (274 mitral PVLs and 88 aortic PVLs). Technical success was achieved in 86.5 % with reduction of paravalvular regurgitation in 76.5 % patients. Improvement in NYHA or haemolysis was achieved in 71 % of patients with a successful procedure. A successful PVL reduction was associated with a lower cardiac mortality (OR=0.08, 95% CI from 0.01 to 0.90) and a superior NYHA class improvement (OR=72.24, 95% CI from 5.09 to 693) compared to failed reduction.
Recently outcomes of several national registries were reported [3131. García E, Arzamendi D, Jimenez-Quevedo P, Sarnago F, Martí G, Sanchez-Recalde A, Lasa-Larraya G, Sancho M, Iñiguez A, Goicolea J, Garcia-San Roman K, Alonso-Briales JH, Molina M, Calabuig J, Freixa X, Berenguer A, Valdes-Chavarri M, Vazquez N, Diaz JF, Cruz-Gonzalez I. Outcomes and predictors of success and complications for paravalvular leak closure. An analysis of the SpanisH real-wOrld paravalvular LEaks closure registry (HOLE registry). EuroIntervention. 2016 Dec 15. , 3232. Calvert PA, Northridge DB, Malik IS, Shapiro L, Ludman P, Qureshi SA, Mullen M, Henderson R, Turner M, Been M, Walsh KP, Casserly I, Morrison L, Walker NL, Thomson J, Spence MS, Mahadevan VS, Hoye A, MacCarthy PA, Daniels MJ, Clift P, Davies WR, Adamson PD, Morgan G, Aggarwal SK, Ismail Y, Ormerod JO, Khan HR, Chandran SS, de Giovanni J, Rana BS, Ormerod O, Hildick-Smith D. Percutaneous Device Closure of Paravalvular Leak: Combined Experience From the United Kingdom and Ireland. Circulation. 2016 Sep 27;134(13):934-44. , 3333. Smolka G, Pysz P, Kozłowski M, Jasiński M, Gocoł R, Roleder T, Kargul A, Ochała A, Wojakowski W. Transcatheter closure of paravalvular leaks using a paravalvular leak device - a prospective Polish registry. Postepy Kardiol Interwencyjnej. 2016;12(2):128-34. ]. The Spanish registry included 514 attempts in 469 patients performed in 19 centres. Reported technical and procedural success was 86.6% and 73.2% respectively. In a multivariate analysis the independent predictors for procedural success for mitral paravalvular leaks were the type of device used (Amplatzer AVP III vs others, HR 2.68 (1.29-5.54), p 0.008) and the number of procedures performed at the centre (top quartile vs others HR 1.93 (1.051-3.53), p 0.03). For aortic leaks the only predictor of procedural success was the leak size (≥10 mm vs <10 mm, HR 3.077 (1.13-8.33) p 0.027). The overall major adverse event rate (death or emergency surgery or stroke) at 30-days was 5.6% [3131. García E, Arzamendi D, Jimenez-Quevedo P, Sarnago F, Martí G, Sanchez-Recalde A, Lasa-Larraya G, Sancho M, Iñiguez A, Goicolea J, Garcia-San Roman K, Alonso-Briales JH, Molina M, Calabuig J, Freixa X, Berenguer A, Valdes-Chavarri M, Vazquez N, Diaz JF, Cruz-Gonzalez I. Outcomes and predictors of success and complications for paravalvular leak closure. An analysis of the SpanisH real-wOrld paravalvular LEaks closure registry (HOLE registry). EuroIntervention. 2016 Dec 15. ]. The combined United Kingdom and Ireland registry included 308 attempts and 259 patients in 20 centers. Successful implantation of the device was achieved in 91% of patients. Mean New York Heart Association class improved from 2.7±0.8 preprocedure to 1.6±0.8 (P<0.001) after a median follow-up of 110 (7–452) days. All-cause mortality during the follow up was 16%, 6% of patients required redo valve surgery and device embolisation occurred in one patient (0.4%) [3232. Calvert PA, Northridge DB, Malik IS, Shapiro L, Ludman P, Qureshi SA, Mullen M, Henderson R, Turner M, Been M, Walsh KP, Casserly I, Morrison L, Walker NL, Thomson J, Spence MS, Mahadevan VS, Hoye A, MacCarthy PA, Daniels MJ, Clift P, Davies WR, Adamson PD, Morgan G, Aggarwal SK, Ismail Y, Ormerod JO, Khan HR, Chandran SS, de Giovanni J, Rana BS, Ormerod O, Hildick-Smith D. Percutaneous Device Closure of Paravalvular Leak: Combined Experience From the United Kingdom and Ireland. Circulation. 2016 Sep 27;134(13):934-44. ].
Procedural failures and complications
The main reason for procedural failure is the inability to cross the defect, mostly with the delivery sheath, although sometimes crossing with a guidewire is not feasible either, as has been shown in nearly all series [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 2121. Cortés M, García E, García-Fernandez MA, Gomez JJ, Perez-David E, Fernández-Avilés F. Usefulness of transesophageal echocardiography in percutaneous transcatheter repairs of paravalvular mitral regurgitation. Am J Cardiol. 2008;101:382-6.
The effect of transoesophageal echocardiographic guidance on success of closure of mitral paravalvular leak, 2222. García-Borbolla Fernández R, Sancho Jaldón M, Calle Pérez G, Gómez Menchero AE, de Zayas Rueda R, Arana Granado R, Marante Fuertes E, Cabeza Laínez P. Percutaneous treatment of mitral valve periprosthetic leakage. An alternative to high-risk surgery?. Rev Esp Cardiol. 2009;62:438-41. , 2323. Hein R, Wunderlich N, Robertson G, Wilson N, Sievert H. Catheter closure of paravalvular leak. EuroIntervention. 2006;2:318-25. , 2424. Pate GE, Al Zubaidi A, Chandavimol M, Thompson CR, Munt BI, Webb JG. Percutaneous closure of prosthetic paravalvular leaks: case series and review. Catheter Cardiovasc Interv. 2006;68:528-33.
Review of paravalvular leak closure in series of 21 patients, 2828. Alonso-Briales JH, Muñoz-García AJ, Jiménez-Navarro MF, Domínguez-Franco AJ, Melero-Tejedor JM, Rodríguez-Bailón I, Hernández-García JM, de Teresa-Galván E. Closure of perivalvular leaks using an Amplatzer occluder. Rev Esp Cardiol. 2009;62:442-6. ]. Instability of the device with risk of device migration [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 2424. Pate GE, Al Zubaidi A, Chandavimol M, Thompson CR, Munt BI, Webb JG. Percutaneous closure of prosthetic paravalvular leaks: case series and review. Catheter Cardiovasc Interv. 2006;68:528-33.
Review of paravalvular leak closure in series of 21 patients] and device interference [1010. Ruiz CE, Jelnin V, Kronzon I, Dudiy Y, Del Valle-Fernandez R, Einhorn BN, Chiam PT, Martinez C, Eiros R, Roubin G, Chen HA. Clinical outcomes in patients undergoing percutaneous closure of periprosthetic paravalvular leaks. J Am Coll Cardiol. 2011;58:2210-7.
Large series of percutaneous closure of paravalvular leaks with follow-up, 2323. Hein R, Wunderlich N, Robertson G, Wilson N, Sievert H. Catheter closure of paravalvular leak. EuroIntervention. 2006;2:318-25. , 2525. Sorajja P, Cabalka AK, Hagler DJ, Rihal CS. Percutaneous repair of paravalvular prosthetic regurgitation: acute and 30-day outcomes in 115 patients. Circ Cardiovasc Interv. 2011;4:314-21.
Short-term results of paravalvular leak closure in 115 patients] with the function of the prosthesis are two major reasons for device retrieval before definite deployment, and therefore one more common reason for the procedure failure. To decrease the risk of interference with the prosthetic valve function in some cases, especially with the crescent-shaped or large leaks, placement of two small simultaneously deployed devices can be used.
Paravalvular leaks with transcatheter aortic valves
Paravalvular leak is a frequent complication of transcatheter aortic valve replacement (TAVR). The reported incidence of mild PVL ranges from 7 to 70 percent and 0 to 24 percent for moderate or severe PVL [3434. Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014;371:967-8. , 3535. Athappan G, Patvardhan E, Tuzcu EM et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol 2013;61:1585-95. , 3636. Gilard M, Eltchaninoff H, Iung B et al. Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med 2012;366:1705-15. , 3737. Kodali SK, Williams MR, Smith CR et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012;366:1686-95. ]. The incidence of PVL is higher with the Core Valve (9% to 21%) than the Edwards (6% to 13.9%) valves [3838. Abdel-Wahab M, Zahn R, Horack M et al. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart 2011;97:899-906. , 3939. Mack MJ, Leon MB, Thourani VH et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med 2019;380:1695-1705. , 4040. Moat NE, Ludman P, de Belder MA et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U.K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol 2011;58:2130-8. , 4141. Popma JJ, Deeb GM, Yakubov SJ et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med 2019;380:1706-1715. , 4242. Walther T, Kasimir MT, Doss M et al. One-year interim follow-up results of the TRAVERCE trial: the initial feasibility study for trans-apical aortic-valve implantation. Eur J Cardiothorac Surg 2011;39:532-7. ]. The newer generation valves have reported significantly lower rates of moderate or severe PVL [3939. Mack MJ, Leon MB, Thourani VH et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med 2019;380:1695-1705. , 4040. Moat NE, Ludman P, de Belder MA et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U.K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol 2011;58:2130-8. , 4141. Popma JJ, Deeb GM, Yakubov SJ et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med 2019;380:1706-1715. ]. Five-year results from the PARTNER 2 trial showed that even mild PVL was associated with significant mortality [3737. Kodali SK, Williams MR, Smith CR et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012;366:1686-95. ]. Moderate or severe PVL was associated with almost a threefold increase in 30-day mortality and a 2.3-fold increase in one-year mortality following TAVR [4343. Kodali S, Pibarot P, Douglas PS et al. Paravalvular regurgitation after transcatheter aortic valve replacement with the Edwards sapien valve in the PARTNER trial: characterizing patients and impact on outcomes. Eur Heart J 2015;36:449-56. ]. Mismatch of the valve annulus and prosthesis diameter sizes, aortic root calcification, and suboptimal device implantation were identified as the major causes for PVL after TAVR [3535. Athappan G, Patvardhan E, Tuzcu EM et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol 2013;61:1585-95. ]. Echocardiography and angiography can be used to assess the PVL during the procedure or at follow up.
Severe calcification of the native valve might prevent the implanted valve from expanding completely and result in significant PVL. Balloon valvuloplasty prior to valve implantation, especially with self-expanding valves, may help with leaflets mobilization and valve expansion. Post-implantation balloon dilation of the prosthesis should be considered as the initial option for the patient with PVL. This approach should not be used for the prostheses deployed high within the annulus as the valve will foreshorten and may embolize. A valve-in-valve (ViV) procedure may be required to address this issue. The conventional way of plugging the leak may also be used if the above measures are not effective. In cases where the valve-in-valve procedure is planned in addition to PVL closure, crossing the leak and device positioning should be done first.
Most common cause of failure
Most common cause of failure is inability to cross the leak with guidewire or delivery catheter
Most complications are common to other percutaneous procedures and they include:
- Access site-related complications: bleeding, vessel dissection or rupture, thromboembolisms, rarely pseudoaneurysm, arteriovenous fistula and infection with vascular access. Complications of the transseptal approach include cardiac perforation and pericardial tamponade, haemothorax, tear of the interatrial septum, conduction abnormalities and arrhythmias. Tamponade, haemothorax, injury to the coronary arteries damage and myocardial infarction are possible complications of the transapical approach.
- Device-related complications: acute or subacute embolisation of the occlusive devices after the deployment, device interference with the prosthetic valve, air embolisation, and device erosion.
- Other: cerebrovascular complications, including transient ischaemic attack and stroke due to thromboembolism/air embolism, calcium detachment and embolisation, haemorrhage as a consequence of procedural heparinisation. Endocarditis is a rare but potentially lethal complication and therefore prophylactic antibiotic is recommended. Persistence or development of the new haemolysis caused by residual leaks around the closure device or shunt through the device itself may persist for several months, until complete endothelisation occurs.
Most common complications
- Access related:
- Bleeding
- Vessel dissection
- Cardiac perforation
- Arrhythmias
- Device related:
- Acute/subacute device embolisation
- Interference with the prosthetic valve
- Other:
- TIA/Stroke
- Worsening haemolysis
Personal perspective - Carlos E. Ruiz
Currently, results of percutaneous closure of paravalvular leaks are limited by the absence of dedicated closure devices and limitation of available integrated imaging modalities, even though percutaneous closure results appear to be superior to surgical outcomes. With the introduction of new, specifically designed closure devices and development of new imaging techniques, results will only improve.
Online data supplement
Illustrative case 1
Mitral paravalvular leak closure - Mixed retrograde and transseptal approach
Moving image 1
Evaluation of paravalvular leak using echocardiography
Moving image 2
Evaluation of patient with mitral bioprosthesis using volume rendered CTA
Moving image 3
Post-procedure volume rendered CTA












The highest rate of PVLs, is found at the right coronary cusp (between 7 and 11 o’clock), despite the right cusp is between 3 and 7 ????