Summary
Patients undergoing saphenous vein graft (SVG) intervention usually present with degenerated SVGs, are often older, and suffer significant comorbidities. SVG intervention carries a higher risk of distal embolization and poorer outcome than native coronary vessel intervention, despite advances in embolic protection and pharmacotherapy. Although, embolic protection devices have demonstrated to decrease the risk of embolization after SVG intervention, their value in contemporary practice have been questioned. However, in many cases those devices are not utilised or cannot be used. This article describes the natural history of disease involving SVGs, discusses the risk-benefit of SVG interventions, reviews prevention strategies for no-reflow, and offers a perspective on the utility of percutaneous SVG intervention in both elective and acute settings.
Introduction
The utility of aorto-coronary saphenous vein grafts (SVGs) is limited by gradual attrition, regardless of the territory bypassed: approximately 10% of SVGs occlude before hospital discharge or within 30 days, 65% to 80% are patent at 5 years, and 50% to 60% are patent at 10 years [11. Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616-26. , 22. Goldman S, Zadina K, Moritz T, Ovitt T, Sethi G, Copeland JG, Thottapurathu L, Krasnicka B, Ellis N, Anderson RJ, Henderson W. VA Cooperative Study Group. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs Cooperative Study. J Am Coll Cardiol. 2004;44:2149-56. , 33. Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years. Ann Thorac Surg. 2004;77:93-101. ]. This is evidenced by the recurrence of angina in 25% of coronary artery bypass graft (CABG) patients at 1 year [44. Cameron AA, Davis KB, Rogers WJ. Recurrence of angina after coronary artery bypass surgery: predictors and prognosis (CASS Registry). Coronary Artery Surgery Study. Journal of the American College of Cardiology. 1995;26:895-9. ]. Degenerated SVGs thus present a clinical dilemma. Compared to first-time CABG, re-operative CABG results in higher rates of mortality, less relief of angina, and more frequent graft failure [11. Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616-26. , 55. Loop FD, Lytle BW, Cosgrove DM, Woods EL, Stewart RW, Golding LA, Goormastic M, Taylor PC. Reoperation for coronary atherosclerosis; Changing practice in 2509 consecutive patients. Ann Surg. 1990;212:378-85; discussion 385-6. , 66. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916-31.
This manuscript provides a comprehensive review of the pathogenesis process of the saphenous vein graft disease and the clinical basis for medical therapy.]. Patients with degenerated SVGs are often older and suffer significant comorbidities, thereby adding to their surgical risk. Percutaneous coronary intervention (PCI) of SVGs, however, also results in higher rates of mortality, periprocedural myocardial infarction (MI) and restenosis when compared to native vessel PCI [77. Frimerman A, Rechavia E, Eigler N, Payton MR, Makkar R, Litvack F. Long-term follow-up of a high risk cohort after stent implantation in saphenous vein grafts. Journal of the American College of Cardiology. 1997;30:1277-83. , 88. Watson PS, Hadjipetrou P, Cox SV, Pyne CT, Gossman DE, Piemonte TC, Eisenhauer AC. Angiographic and clinical outcomes following acute infarct angioplasty on saphenous vein grafts. American Journal of Cardiology. 1999;83:1018-21. , 99. Pucelikova T, Mehran R, Kirtane AJ, Kim YH, Fahy M, Weisz G, Lansky AJ, Moussa I, Gray WA, Collins MB, Kodali SK, Stone GW, Moses JW, Leon MB, Dangas G. Short- and long-term outcomes after stent-assisted percutaneous treatment of saphenous vein grafts in the drug-eluting stent era. American Journal of Cardiology. 2008;101:63-8. ]. An important reason for poorer outcomes of PCI in SVGs is the embolization of atherothrombotic debris into the native coronary circulation, often resulting in periprocedural MI or reduced antegrade flow (the “no-reflow” phenomenon). Strategies for addressing this distal embolization problem include both proximal and distal protection devices, as well as adjunctive pharmacology and new stenting approaches. Despite these advances, rates of restenosis and target vessel failure of degenerated SVGs remain relatively high. The objective of this chapter is to discuss the risk-benefit of SVG interventions, review the prevention strategies for the no-reflow phenomenon, and offer a perspective on the utility of percutaneous SVG intervention in both elective and acute settings.
Natural history of vein graft disease
The “saphenous vein graft disease” process involves 3 interlinked pathophysiological phenomena that lead to the progressive degeneration: thrombosis, intimal hyperplasia, and atherosclerosis.
THROMBOSIS
About 10% of SVGs occlude, with or without symptoms, within the first month after CABG [. ]. This early phenomenon seems to be related to severe endothelial cell loss and medial damage during harvesting,[1010. Roubos N, Rosenfeldt FL, Richards SM, Conyers RA, Davis BB. Improved preservation of saphenous vein grafts by the use of glyceryl trinitrate-verapamil solution during harvesting. Circulation. 1995;92:II31-6. ] which has been linked to reduced production of nitric oxide and prostacyclins, both potent inhibitors of platelet activations [1010. Roubos N, Rosenfeldt FL, Richards SM, Conyers RA, Davis BB. Improved preservation of saphenous vein grafts by the use of glyceryl trinitrate-verapamil solution during harvesting. Circulation. 1995;92:II31-6. ]. In addition, this prothrombotic stage of SVG may be amplified by technical factors that reduce graft flow, such as intact venous valves, anastomosis stricture, and graft anastomosis proximal to diseased segments. Also, by-passing non-obstructive diseased territories or non-ischemic inducing coronary stenosis may cause competitive flow from native arteries prompting the grafts to fail [9595. Roh JH, Kim YH, Yang DH, Han S, Yun SC, Yang DH, Park GM, Lee PH, Ahn JM, Kang JW, Lim TH, Moon DH, Kim JB, Jung SH, Chung CH, Choo SJ, Lee JW, Kang SJ, Park DW, Lee SW, Lee CW, Park SW, Park SJ. Fate of Grafts Bypassing Nonischemic Versus Ischemic Inducing Coronary Stenosis. Am J Cardiol. 2018;122(7):1148-1154]. ]. The early use of P2Y12 receptor antagonist with or without aspirin after CABG has become common strategy in many centers to prevent early SVG thrombosis [1212. Gao C, Ren C, Li D, Li L. Clopidogrel and aspirin versus clopidogrel alone on graft patency after coronary artery bypass grafting. Ann Thorac Surg. 2009;88:59-62. ]. Several small studies have showed conflicting results on the effectiveness of dual antiplatelet therapy on SVG patency following CABG [9696. Rao C, Ren C, Li D, Li L. Clopidogrel and aspirin versus clopidogrel alone on graft patency after coronary artery bypass grafting. Ann Thorac Surg. 2009;88(1):59-62. , 9797. Gao G, Zheng Z, Pi Y, Lu B, Lu J, Hu S. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery a single-center, randomized, controlled trial. J Am Coll Cardiol. 2010;56(20):1639-1643]. , 9898. Sun J C, Teoh K H, Lamy A, et al. Randomized trial of aspirin and clopidogrel versus aspirin alone for the prevention of coronary artery bypass graft occlusion: the Preoperative Aspirin and Postoperative Antiplatelets in Coronary Artery Bypass Grafting study. Am Heart J. 2010;160(6): 1178-1184]. , 9999. Saw J, Wong G C, Mayo J, et al. Ticagrelor and aspirin for the prevention of cardiovascular events after coronary artery bypass graft surgery. Heart. 2016;102(10):763-769]. ]. The Compared the Efficacy of Different Antiplatelet Therapy Strategy After Coronary Artery Bypass Graft Surgery (DACAB) trial, reported in 500 stable patients randomized (1:1:1) that patients treated with the combination of ticagrelor (90 mg twice daily) + aspirin (100 mg once daily) (n = 168) resulted in better graft patency after 1-year follow-up as compared to ticagrelor (90 mg twice daily) (n = 166) or aspirin (100 mg once daily) (n = 166) alone within 24 hours post-CABG [100100. Zhao Q, Zhu Y, Xu Z, Cheng Z, Mei J, Chen X, Wang X. Effect of Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone on Saphenous Vein Graft Patency 1 Year After Coronary Artery Bypass Grafting: A Randomized Clinical Trial. JAMA. 2018; 319(16):1677-1686]. ]. Large randomized clinical trials informing on clinical endpoints are needed to make clear and routine or selective recommendations on this topic, when balancing the ischemic versus the bleeding endpoints.
INTIMAL HYPERPLASIA
Accumulation of smooth muscle cells and extracellular matrix in the intimal space – a process known as intimal hyperplasia – is the main disease process that occurs during the first months after implantation, and appears to be related to transient ischaemia incurred during explantation and reperfusion after grafting [66. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916-31.
This manuscript provides a comprehensive review of the pathogenesis process of the saphenous vein graft disease and the clinical basis for medical therapy.]. The pronounced increase in wall stress by exposure to arterial pressures seems to be another important factor promoting intimal fibrosis [66. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916-31.
This manuscript provides a comprehensive review of the pathogenesis process of the saphenous vein graft disease and the clinical basis for medical therapy.]. Although this process rarely produces significant stenosis, it represents the foundation for later development of SVG atherosclerosis.
ATHEROSCLEROSIS
In the first year after CABG, atherosclerosis is the dominant process involved in SVG disease, but recurrent symptoms due to SVG disease rarely occur before 3 years after grafting [66. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916-31.
This manuscript provides a comprehensive review of the pathogenesis process of the saphenous vein graft disease and the clinical basis for medical therapy.]. Morphologically, vein graft atherosclerosis tends to be diffuse, concentric, and friable with a poorly developed or absent fibrous cap and little evidence of calcification
( Figure 1 ) [1313. Kalan JM, Roberts WC. Morphologic findings in saphenous veins used as coronary arterial bypass conduits for longer than 1 year: necropsy analysis of 53 patients, 123 saphenous veins, and 1865 five-millimeter segments of veins. Am Heart J. 1990;119:1164-84. ]. Angiographic studies have shown that atherosclerotic vein graft disease is the culprit lesion in 70% to 85% of the acute coronary syndromes presented after CABG [1414. Chen L, Theroux P, Lesperance J, Shabani F, Thibault B, De Guise P. Angiographic features of vein grafts versus ungrafted coronary arteries in patients with unstable angina and previous bypass surgery. J Am Coll Cardiol. 1996;28:1493-9. ]. Late thrombotic occlusion resulting in ischaemic MI frequently occurs in old and degenerated SVGs [66. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916-31.
This manuscript provides a comprehensive review of the pathogenesis process of the saphenous vein graft disease and the clinical basis for medical therapy.]. A recently published large randomized clinical trial demonstrated the superiority of radial-artery grafts to SVGs using contemporary techniques. To a mean follow-up of 60±30 months 534 patients treated with radial-artery grafts were compared to 502 patients treated with SVGs. The use of radial-artery grafts was associated with a significant lower risk of graft occlusion (HR 0.44; 95% CI 0.28-0.70), lower risk myocardial infarction (HR 0.72; 95% CI 0.53-0.99) and lower repeated revascularization (HR 0.5; 95% CI 0.4-0.63) [101101. Gaudino M, Benedetto U, Fremes S, Biondi-Zoccai G, Sedrakyan A, Puskas JD, Angelini GD, Buxton B, Frati G, Hare DL, Hayward P, Nasso G, Moat N, Peric M, Yoo KJ, Speziale G, Girardi LN, Taggart DP; RADIAL Investigators. Radial-Artery or Saphenous-Vein Grafts in Coronary-Artery Bypass Surgery. N Engl J Med. 2018; 378(22):2069-2077]. ]. Therefore, radial-artery grafts should be strongly considered as the preferred second conduit to the left internal thoracic artery, particularly in young patients, female patients, patients without renal insufficiency, diabetes or chronic obstructive lung disease [102102. Shapira OM. Radial Artery as the Preferred Second Conduit for Coronary Bypass. N Engl J Med. 2018; 378(22):2134-2135]. ]. Aggressive lipid controlling therapy remains a cornerstone of medical treatment to avoid SVG disease progression and to maintain the long-term graft patency. [5656. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. The Post Coronary Artery Bypass Graft Trial Investigators. N Engl J Med. 1997;336:153-62. , 5757. Hata M, Takayama T, Sezai A, Yoshitake I, Hirayama A, Minami K. Efficacy of aggressive lipid controlling therapy for preventing saphenous vein graft disease. Ann Thorac Surg. 2009;88:1440-4. , 5858. Hong YJ, Mintz GS, Kim SW, Lee SY, Kim SY, Okabe T, Pichard AD, Satler LF, Waksman R, Kent KM, Suddath WO, Weissman NJ. Disease progression in non-intervened saphenous vein graft segments a serial intravascular ultrasound analysis. Journal of the American College of Cardiology. 2009;53:1257-64. , 103103. Brilakis ES, de Lemos JA, Cannon CP, et al. Outcomes of patients with acute coronary syndrome and previous coronary artery bypass grafting (from the pravastatin or atorvastatin evaluation and infection therapy [PROVE IT-TIMI 22] and the Aggrastat to Zocor [A to Z]trials). Am J Cardiol. 2008: 102: 552–558]. ] Compared to moderate statin therapy, long-term aggressive statin therapy has been demonstrated to lower the LDL-C level significantly, further decreasing the atherosclerotic progression of SVG, and reducing the risks of repeated myocardial infarction and coronary revascularization after CABG. [104104. Kang S, Liu Y, Liu XB. Effects of aggressive statin therapy on patients with coronary saphenous vein bypass grafts: a systematic review and meta-analysis of randomized, controlled trials. Clin Ther. 2013;35(8):1125-36]. ] Therefore, long-term aggressive statin therapy remains as a mandatory component of the medical treatment after CABG.
Natural history of vein graft disease
- Thrombosis
- early phenomenon, related to vein damage and technical issues
- about 10% of vein grafts are occluded and are frequently asymptomatic in the first month after CABG
- Intima hyperplasia
- occurrs in the first months after CABG
- represents the basis for later atherosclesosis
- Atherosclerosis
- dominant disease process involving the vein graft after 1 year
- usually symptomatic for 3 years after CABG
- morphologically characterised by diffuse, concentric, and friable plaques with a poorly developed or absent fibrous cap and little evidence of calcification
Correlates and clinical outcomes after percutaneous saphenous vein graft intervention
The predictors of 30-day major cardiac events after SVG intervention were explored in the pooled analysis of 3,958 patients from 5 randomised clinical trials and 1 registry [1515. Coolong A, Baim DS, Kuntz RE, O’Malley AJ, Marulkar S, Cutlip DE, Popma JJ, Mauri L. Saphenous vein graft stenting and major adverse cardiac events: a predictive model derived from a pooled analysis of 3958 patients. Circulation. 2008;117:790-7.
Pooled analysis of 3958 patients enrolled in 5 randomized, controlled trials and 1 registry of embolic protection devices, identified 2 angiographic measures of plaque burden, plaque volume and a graft degeneration score, age and tobacco use as the most important predictors for major 30-days adverse events.]. This pooled analysis reported the degree of SVG degeneration assessed by the SVG degeneration score (p <0.0001), the estimated plaque volume (p <0.0001), angiographic evidence of thrombus (p=0.003), increasing patient age (p <0.005), glycoprotein IIb/IIIa inhibitor use (p=0.02), and current smoking (p=0.03) as those correlates associated with the 30-day composite outcome of death, MI and target lesion revascularisation (TLR) [1515. Coolong A, Baim DS, Kuntz RE, O’Malley AJ, Marulkar S, Cutlip DE, Popma JJ, Mauri L. Saphenous vein graft stenting and major adverse cardiac events: a predictive model derived from a pooled analysis of 3958 patients. Circulation. 2008;117:790-7.
Pooled analysis of 3958 patients enrolled in 5 randomized, controlled trials and 1 registry of embolic protection devices, identified 2 angiographic measures of plaque burden, plaque volume and a graft degeneration score, age and tobacco use as the most important predictors for major 30-days adverse events.] ( Table 1 ).
As previously mentioned, patients undergoing PCI on SVGs have poorer outcomes. A pooled analysis of 5 randomised glycoprotein IIb/IIIa inhibitor trials showed that PCI in SVGs carries a significant increase in mortality compared to native vessels at 30 days (2.1% vs. 1.0%) and 6 months (4.7% vs. 2.0%) 16]. Only a few retrospective series have addressed the long-term follow-up after PCI performed on SVGs. In the largest published series, Keeley et al reported a 54% rate of the composite end point (death-MI-repeat revascularisation) at 3 years from PCI performed in 1,062 patients, including death in 9%, Q-wave-MI in 9% and target vessel revascularisation in 36% by either surgery or PCI [1717. Keeley EC, Velez CA, O’Neill WW, Safian RD. Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J Am Coll Cardiol. 2001;38:659-65.
Largest clinical series providing on the long-term clinical outcomes following saphenous vein graft PCI. The data confirm the poor prognosis of this population suggesting that the late outcome dependents on the extent and progression of atherosclerosis and not the target lesion per se.] ( Figure 2 ).
The rate of angioplasty failure has been significantly improved after the introduction of stents. Plain balloon angioplasty has been associated with restenosis rates of 42% compared to 27% for bare metal stents (BMSs) after 240 days’ follow-up in the only controlled comparative data available on SVGs [Saphenous Vein De Novo (SAVED) trial] [1818. Savage MP, Douglas JS Jr, Fischman DL, Pepine CJ, King SB 3rd, Werner JA, Bailey SR, Overlie PA, Fenton SH, Brinker JA, Leon MB, Goldberg S. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts; Saphenous Vein De Novo Trial Investigators. N Engl J Med. 1997;337:740-7. ]. Larger observational studies have confirmed the stenting benefit [1717. Keeley EC, Velez CA, O’Neill WW, Safian RD. Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J Am Coll Cardiol. 2001;38:659-65.
Largest clinical series providing on the long-term clinical outcomes following saphenous vein graft PCI. The data confirm the poor prognosis of this population suggesting that the late outcome dependents on the extent and progression of atherosclerosis and not the target lesion per se., 1919. Brener SJ, Ellis SG, Apperson-Hansen C, Leon MB, Topol EJ. Comparison of stenting and balloon angioplasty for narrowings in aortocoronary saphenous vein conduits in place for more than five years. Am J Cardiol. 1997;79:13-8. ]. The particular issue of the risk-benefit of using drug-eluting stents (DESs) or BMSs to treat SVGs will be addressed in a dedicated subsection of this chapter.
Different subsets of SVG lesions and presentations require specific consideration in terms of percutaneous interventions and the related outcomes:
EARLY ISCHAEMIA AFTER CABG SURGERY.
Early graft occlusion (within the first 30 days) occurs in up to 10%, is usually thrombotic, and is related to technical issues involving the anastomosis or graft manipulation during the harvesting [11. Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616-26. , 2020. Dauerman HL, Cutlip DE, Sellke FW. Intracoronary thrombolysis in the treatment of graft closure immediately after CABG. Ann Thorac Surg. 1996;62:280-3. ]. This process is different from tissue oedema surrounding the anastomosis, giving angiographic stenosis, as it resolves spontaneously with time. The risk of acute graft occlusion seems to be reduced by early use of DAPT after CABG [1212. Gao C, Ren C, Li D, Li L. Clopidogrel and aspirin versus clopidogrel alone on graft patency after coronary artery bypass grafting. Ann Thorac Surg. 2009;88:59-62. , 9696. Rao C, Ren C, Li D, Li L. Clopidogrel and aspirin versus clopidogrel alone on graft patency after coronary artery bypass grafting. Ann Thorac Surg. 2009;88(1):59-62. , 9797. Gao G, Zheng Z, Pi Y, Lu B, Lu J, Hu S. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery a single-center, randomized, controlled trial. J Am Coll Cardiol. 2010;56(20):1639-1643]. , 9898. Sun J C, Teoh K H, Lamy A, et al. Randomized trial of aspirin and clopidogrel versus aspirin alone for the prevention of coronary artery bypass graft occlusion: the Preoperative Aspirin and Postoperative Antiplatelets in Coronary Artery Bypass Grafting study. Am Heart J. 2010;160(6): 1178-1184]. , 9999. Saw J, Wong G C, Mayo J, et al. Ticagrelor and aspirin for the prevention of cardiovascular events after coronary artery bypass graft surgery. Heart. 2016;102(10):763-769]. , 100100. Zhao Q, Zhu Y, Xu Z, Cheng Z, Mei J, Chen X, Wang X. Effect of Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone on Saphenous Vein Graft Patency 1 Year After Coronary Artery Bypass Grafting: A Randomized Clinical Trial. JAMA. 2018; 319(16):1677-1686]. ]. About 3% to 6% of patients develop clinical ischaemia as manifested by significant ischaemic electrocardiogram abnormalities, haemodynamic instability (low output) and/or ventricular arrhythmias [2121. Fabricius AM, Gerber W, Hanke M, Garbade J, Autschbach R, Mohr FW. Early angiographic control of perioperative ischemia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 2001;19:853-8. , 2222. Rasmussen C, Thiis JJ, Clemmensen P, Efsen F, Arendrup HC, Saunamäki K, Madsen JK, Pettersson G. Significance and management of early graft failure after coronary artery bypass grafting: feasibility and results of acute angiography and re-re-vascularization. Eur J Cardiothorac Surg. 1997;12:847-52. ]. However, when patients undergo urgent angiography due to significant ischaemia after CABG, SVG occlusion is demonstrated in 37% to 56% and internal mammary occlusion in 12% to 29% [2121. Fabricius AM, Gerber W, Hanke M, Garbade J, Autschbach R, Mohr FW. Early angiographic control of perioperative ischemia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 2001;19:853-8. , 2222. Rasmussen C, Thiis JJ, Clemmensen P, Efsen F, Arendrup HC, Saunamäki K, Madsen JK, Pettersson G. Significance and management of early graft failure after coronary artery bypass grafting: feasibility and results of acute angiography and re-re-vascularization. Eur J Cardiothorac Surg. 1997;12:847-52. ]. Either surgical or percutaneous revascularisation in this situation carries higher risk. PCI is associated with higher rates of bleeding complications, especially when patients are treated very soon after the surgery [2323. Price MJ, Housman L, Teirstein PS. Rescue percutaneous coronary intervention early after coronary artery bypass grafting in the drug-eluting stent era. Am J Cardiol. 2006;97:789-91. ]. The 2005 American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines recommend PCI if feasible in patients with early ischaemia after CABG [2424. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, King SB 3rd, Morrison DA, O’Neill WW, Schaff HV, Whitlow PL, Williams DO, Antman EM, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention-summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). Circulation. 2006;113:156-75. ]. We generally recommend low pressure balloon angioplasty for the treatment of distal anastomosis, with stenting used only if the result is suboptimal.
STENOSIS OF THE DISTAL ANASTOMOSIS
The rate of restenosis at the anastomosis site seems to be lower than in the aorto-ostial or shaft locations. In a retrospective series of 182 patients who underwent either balloon angioplasty or stenting of the distal anastomosis, the in-hospital outcome was the same, with low rates of ischaemic complications [2525. Gruberg L, Hong MK, Mehran R, et al. In-hospital and long-term results of stent deployment compared with balloon angioplasty for treatment of narrowing at the saphenous vein graft distal anastomosis site. Am J Cardiol. 1999;84:1381-4.
Retrospective series of 182 patients who underwent either balloon angioplasty or stenting of the distal anastomosis showed similar clinical outcomes. The study suggests that percutaneous revascularization of the SVG distal anastomosis site can be performed with a high rate of procedural success and favorable outcomes.]. After an average of 17 months’ follow-up, mortality rates were similar for patients who underwent balloon angioplasty and stenting (11.6% vs. 13%, p=NS) and Q-wave MI rates were also similar (1% vs. 0%, p=NS). Percutaneous revascularisation of the SVG distal anastomosis site can be performed with a high rate of procedural success and favorable outcomes. Stent deployment may further improve long-term outcome by reducing the need for repeat revascularisation.
INTERNAL MAMMARY ARTERY GRAFT DISEASE
The internal mammary artery (IMA) is considered the vascular conduit of choice for patients undergoing surgical revascularisation to the left anterior descending artery. We have learned that IAM disease involving the anastomosis site has to be preferentially treated with balloon angioplasty alone. In a retrospective series of 174 patients who underwent 202 lesions interventions on IMA, balloon angioplasty (n=163) was compared to stenting PCI (n=39) [2626. Gruberg L, Dangas G, Mehran R, Hong MK, Waksman R, Mintz GS, Kent KM, Pichard AD, Satler LF, Lansky AJ, Stone GW, Leon MB. Percutaneous revascularization of the internal mammary artery graft: short- and long-term outcomes. J Am Coll Cardiol 2000;35:944-8.
Retrospective series of 174 patients who underwent 202 lesions interventions on internal mammary artery grafts, balloon angioplasty (n=163) was compared to stenting PCI (n=39). Repeated revascularization of the anastomotic site was significantly lower by using balloon alone as compared to stenting.]. For the anastomotic site, TLR was 4.3% for patients treated with balloon PCI and 33% for those treated with stents. Based on this study we strongly recommend balloon angioplasty as the procedure of choice to treat stenosis involving the anastomotic site on IMAs.
CHRONIC TOTALLY OCCLUDED SVG
Reported success rates of intervention in chronically occluded SVGs range from 58% to 77% [2727. Stone GW, Reifart NJ, Moussa I, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation. 2005;112:2530-7. ]. Studies have demonstrated poor long-term results after recanalisation of occluded SVGs [2727. Stone GW, Reifart NJ, Moussa I, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation. 2005;112:2530-7. ]. Thus the risk/benefit ratio has to be carefully assessed before PCI of an occluded SVG is undertaken. If recanalisation of the underlying native vessel is not possible, unless the patient has life-impairing symptoms or a large jeopardised myocardial territory, medical management should initially be pursued for most occluded SVGs [2727. Stone GW, Reifart NJ, Moussa I, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation. 2005;112:2530-7. ]. Current trends show that treatment of the native artery is the preferred choice in chronically occluded SVGs. Improved techniques and results for CTO treatment allow for this option in ways not present a few years ago. [105105. Galassi AR, Werner GS, Boukhris M, Azzalini L, Mashayekhi K, Carlino M, Avran A, Konstantinidis NV, Grancini L, Bryniarski L, Garbo R, Bozinovic N, Gershlick AH, Rathore S, Di Mario C, Louvard Y, Reifart N, Sianos G. Percutaneous Recanalization of Chronic Total Occlusions: 2019 Consensus Document from the EuroCTO Club. EuroIntervention. 2019;15: EIJ-D-18-00826]. ]
Specific graft lesion intervention subtypes and the related outcomes
- Early ischaemia after CABG surgery (within the first 30 days)
- early graft occlusion, usually thrombotic, occurs in up to 10%
- 3% to 6% of patients develop clinically significant ischaemia
- in symptomatic patients, 37% to 56% SVG are occluded on angiogram
- PCI is recommended in the presence of clinical evidence of relevant ischaemia
- Stenosis of the distal anastomosis
- PCI has particularly good results, better than ostial and shaft location results
- Internal mammary artery graft disease
- balloon PCI appears to be the procedure of choice to treat internal mammary artery stenosis
- Chronic totally occluded SVG
- related to poor short-term and long-term outcomes
- native recanalisation is preferred if possible
- PCI only justified in the presence of life-impaired symptoms or a large, jeopardised myocardium
When to intervene a saphenous vein graft
Due to the increased risk of periprocedural MI related to SVG interventions, PCI of the native grafted vessel is usually preferred over PCI of the degenerated SVG [1717. Keeley EC, Velez CA, O’Neill WW, Safian RD. Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J Am Coll Cardiol. 2001;38:659-65.
Largest clinical series providing on the long-term clinical outcomes following saphenous vein graft PCI. The data confirm the poor prognosis of this population suggesting that the late outcome dependents on the extent and progression of atherosclerosis and not the target lesion per se., 2020. Dauerman HL, Cutlip DE, Sellke FW. Intracoronary thrombolysis in the treatment of graft closure immediately after CABG. Ann Thorac Surg. 1996;62:280-3. , 2828. Stone GW, Reifart NJ, Moussa I, Hoye A, Cox DA, Colombo A, Baim DS, Teirstein PS, Strauss BH, Selmon M, Mintz GS, Katoh O, Mitsudo K, Suzuki T, Tamai H, Grube E, Cannon LA, Kandzari DE, Reisman M, Schwartz RS, Bailey S, Dangas G, Mehran R, Abizaid A, Moses JW, Leon MB, Serruys PW. Creatine kinase- MB enzyme elevation following successful saphenous vein graft intervention is associated with late mortality. Circulation. 1999;100:2400-5. ]. When PCI of the native vessel is not possible, however, the clinical benefit of a high-risk SVG intervention should be balanced against the risk of morbidity and mortality of repeating the surgical revascularisation (2-fold to 4-fold compared to the primary intervention) [3030. Salomon NW, Page US, Bigelow JC, Krause AH, Okies JE, Metzdorff MT. Reoperative coronary surgery; Comparative analysis of 6591 patients undergoing primary bypass and 508 patients undergoing reoperative coronary artery bypass. J Thorac Cardiovasc Surg. 1990;100:250-9; discussion 259-60. , 3131. Weintraub WS, Jones EL, Craver JM, Grosswald R, Guyton RA. In-hospital and long-term outcome after reoperative coronary artery bypass graft surgery. Circulation. 1995;92:II50-7. ]. Also, repeat CABG is less effective in terms of complete revascularisation and symptom control when compared to the first procedure.
Limited studies have compared the efficacy of PCI to repeat CABG. This issue was directly addressed by the Angina with Extremely Serious Operative Mortality Evaluation (AWESOME) trial/registry of 142 patients with refractory post-CABG ischaemia who were reasonable candidates for either PCI or CABG [3232. Morrison DA, Sethi G, Sacks J, Henderson WG, Grover F, Sedlis S, Esposito R. Percutaneous coronary intervention versus repeat bypass surgery for patients with medically refractory myocardial ischemia: AWESOME randomized trial and registry experience with post-CABG patients. J Am Coll Cardiol. 2002;40:1951-4. ]. Arterial grafts were used in 75% of repeated CABG and BMS in 54% of PCIs. Initial in-hospital mortality was higher in the CABG group (8% vs. 0%), but after 3-year follow-up there was no difference in the overall survival. Nonetheless, a benefit trend towards free-symptom survival was observed in the CABG group (65% vs. 48%) [3232. Morrison DA, Sethi G, Sacks J, Henderson WG, Grover F, Sedlis S, Esposito R. Percutaneous coronary intervention versus repeat bypass surgery for patients with medically refractory myocardial ischemia: AWESOME randomized trial and registry experience with post-CABG patients. J Am Coll Cardiol. 2002;40:1951-4. ]. A larger retrospective study described the results of 2191 patients from 1995-2000 with prior CABG who underwent multivessel revascularisation: 1,487 repeat CABG and 704 PCI [3333. Brener SJ, Lytle BW, Casserly IP, Ellis SG, Topol EJ, Lauer MS. Predictors of revascularization method and long-term outcome of percutaneous coronary intervention or repeat coronary bypass surgery in patients with multivessel coronary disease and previous coronary bypass surgery. Eur Heart J. 2006;27:413-8. ]. Complete revascularisation was achieved more frequently in the PCI group (89% vs. 71%, p <0.001). Periprocedural Q-wave MI was significantly higher in the CABG group (1.4% vs. 0.3%, p=0.01), however, similar mortality rates were observed at 30 days’ follow-up (2.8% in the CABG group vs. 1.7% in the PCI group, p=0.34). After 5-year follow-up, PCI was associated with a non-significant increase in the adjusted mortality (hazard ratio of 1.47, p=0.09). The most important factors involved in the choice of repeat CABG were more extensive SVG/native disease, previous MI, lower left ventricular ejection fraction, longer interval from first CABG and the absence of patent mammary graft.
Based on the described evidence, the last updated ACC/AHA/SCAI guidelines in this topic (2005) recommend PCI in the following circumstances:[2424. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, King SB 3rd, Morrison DA, O’Neill WW, Schaff HV, Whitlow PL, Williams DO, Antman EM, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention-summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). Circulation. 2006;113:156-75. ] ( Table 2 ).
Early ischaemia (usually within 30 days) after CABG, when technically feasible (Class I).
Ischaemia that occurs 1 to 3 years after CABG in patients with discrete lesions and preserved LV function. It is also reasonable in patients with diseased SVGs older than 3 years; and if feasible, in patients with patent left internal mammary artery and significant obstruction in other vessels (Class IIa).
PCI is not recommended in patients with total SVG occlusions, or multiple target lesions (native/SVG disease) and impaired LV function, unless repeat CABG poses excessive risk (Class III).
In addition, CABG is usually reserved for patients who cannot have adequate percutaneous revascularisation or for those who may gain an additional benefit from CABG, such as those with previously unused left IMA to left anterior descending artery. Indeed the 2004 ACC/AHA guidelines recommend repeat CABG in the following settings:[3434. Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, Lytle BW, Marlow RA, Nugent WC, Orszulak TA. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation. 2004;110:e340-437. ] ( Table 3 ).
Disabling ischaemia, despite optimal medical therapy (Class I).
Prior CABG without patent grafts and with a Class I indication for surgery due to native disease: left main disease left main equivalent, or 3-vessel disease (Class I).
Atherosclerotic vein grafts with >50% stenosis in vessels that supply the left anterior descending artery or large areas of myocardium (Class IIa). These indications for PCI are echoed in the ESC revascularisation guidelines (2014) [106106. Authors/Task Force members, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541-619]. ] ( Table 4 ). In addition, the European guidelines emphasise the importance of the Heart team in decision-making.
In summary, PCI is usually preferred over repeat CABG for early recurrent symptoms after CABG (<3 years). However, most symptomatic post-CABG patients present with extensive native and graft disease where the revascularisation strategy must be based on careful risk/benefit assessment of the procedure and the local experience.
Drug-eluting stent versus bare metal stent to treat saphenous vein grafts
DES use has been associated with a significant improvement in clinical outcomes by decreasing the restenosis rate in native coronary artery lesions when compared to BMSs. Several types of DESs are currently available: eluting sirolimus, paclitaxel, zotarolimus, everolimus and biolimus with durable or biodegradable polymers. DES have been increasingly utilised in SVG interventions without strong clinical evidence favoring their use [107107. Brilakis ES, Wang TY, Rao SV, Banerjee S, Goldman S, Shunk K, Kar B, Holmes DR Jr, Dai D, Chin CT, Harding TM, Roe MT. Frequency and predictors of drug-eluting stent use in saphenous vein bypass graft percutaneous coronary interventions: a report from the American College of Cardiology National Cardiovascular Data CathPCI registry. JACC Cardiovasc Interv. 2010;3:1068–1073]. ]. Five randomized clinical trials comparing BMS with DES have resulted in conflicting results. Four of them showed benefit (SOS, Stenting Of Saphenous Vein Grafts [4141. Brilakis ES, Lichtenwalter C, de Lemos JA, Roesle M, Obel O, Haagen D, Saeed B, Gadiparthi C, Bissett JK, Sachdeva R, Voudris VV, Karyofillis P, Kar B, Rossen J, Fasseas P, Berger P, Banerjee S. A randomized controlled trial of a paclitaxel-eluting stent versus a similar bare-metal stent in saphenous vein graft lesions the SOS (Stenting of Saphenous Vein Grafts) trial. J Am Coll Cardiol. 2009;53:919-28.
In the SOS trial 80 patients with 112 de novo and restenotic lesions in 88 grafts were enrolled: 41 patients received 62 paclitaxel-eluting stents (PES) for 57 lesions, whereas 39 patients received 62 BMSs for 55 lesions. Binary angiographic restenosis occurred in 51% of the BMS-treated lesions versus 9% of the PES-treated lesions (relative risk: 0.18)]; ISAR-CABG, Is Drug-Eluting-Stenting Associated with Improved Results in Coronary Artery Bypass Grafts [4444. Mehilli J1, Pache J, Abdel-Wahab M, Schulz S, Byrne RA, Tiroch K, Hausleiter J, Seyfarth M, Ott I, Ibrahim T, Fusaro M, Laugwitz KL, Massberg S, Neumann FJ, Richardt G, Schömig A, Kastrati A. Drug-eluting versus bare-metal stents in saphenous vein graft lesions (ISAR-CABG): a randomised controlled superiority trial. Lancet. 2011;378:1071-8. ]; BASKET-SAVAGE [108108. . BAsel Stent Kosten-Effektivitäts- Saphenous Vein Graft Angioplasty Using Glycoprotein 2b/3a Receptor Inhibitor and Drug-Eluting Stents. ESC Congress, Rome 2016. ]; and BASKET, BAsel Stent Kosten-Effektivitäts [3838. Brunner-La Rocca HP, Kaiser C, Pfisterer M. Targeted stent use in clinical practice based on evidence from the Basel Stent Cost Effectiveness Trial (BASKET). Eur Heart J. 2007;28:719-25. ]), whereas one showed to be harmful, due to an increase in mortality observed after 3-year follow-up (DELAYED-RRISC, Reduction of Restenosis In Saphenous Vein Grafts With Cypher Sirolimus-Eluting Stent trial [109109. Vermeersch P, Agostoni P, Verheye S, Van den Heuvel P, Convens C, Van den Branden F, Van Langenhove G; DELAYED RRISC (Death and Events at Long-term follow-up AnalYsis: Extended Duration of the Reduction of Restenosis In Saphenous vein grafts with Cypher stent) Investigators. Increased late mortality after sirolimus-eluting stents versus bare-metal stents in diseased saphenous vein grafts: results from the randomized DELAYED RRISC Trial. J Am Coll Cardiol. 2007;50:261–267]. ]). All these mentioned trials are limited by the relative small sample size, lack of blindness, routine angiographic follow-up, low use of embolic protection device and the use of first generation DES. Recently, the results of the DIVA (Drug-Eluting Stents Versus Bare-Metal Stents In Saphenous Vein Graft Angioplasty) were published, one of the largest randomized clinical trials compared blindly BMS versus contemporary DES in SVG-PCIs, by using relevant clinical endpoints, in contrast to the previous trials reporting angiographic endpoints [110110. Brilakis ES, Edson R, Bhatt DL, Goldman S, Holmes DR Jr, Rao SV, Shunk K, Rangan BV, Mavromatis K, Ramanathan K, Bavry AA, Garcia S, Latif F, Armstrong E, Jneid H, Conner TA, Wagner T, Karacsonyi J, Uyeda L, Ventura B, Alsleben A, Lu Y, Shih MC, Banerjee S; DIVA Trial Investigators. Drug-eluting stents versus bare-metal stents in saphenous vein grafts: a double-blind, randomised trial. Lancet. 2018; 391(10134):1997-2007]. ]. At 12-month follow-up the primary end-point was similar between DES vs BMS, with no differences in cardiac mortality, target vessel MI or TVR, and stent thrombosis. It should be mentioned that the early benefit observed in the ISAR-CABG trial was lost at 5-years due to higher attrition of DES efficacy over time [111111. Colleran R, Kufner S, Mehilli J, Rosenbeiger C, Schüpke S, Hoppmann P, Joner M, Mankerious N, Fusaro M, Cassese S, Abdel-Wahab M, Neumann FJ, Richardt G, Ibrahim T, Schunkert H, Laugwitz KL, Kastrati A, Byrne RA; ISAR-CABG Investigators. Efficacy Over Time With Drug-Eluting Stents in Saphenous Vein Graft Lesions. J Am Coll Cardiol. 2018; 71(18):1973-1982]. ]. The rate of death, cardiac death, MI and stent thrombosis remained similar at 5-years follow-up.
An updated meta-analysis of the randomized clinical trials comparing DES versus BMS in SVG interventions, compared the pooled results of the 6 mentioned trials [112112. Shah R, Jovin IS, Latham SB, Hesterberg K, Heckle MR, Rashid A, Vetrovec GW. A comprehensive meta-analysis of randomized controlled trials comparing drug-eluting stents with bare-metal stents in saphenous vein graft interventions. Catheter Cardiovasc Interv. 2018;92(7):1229-1236]. ]. The clinical characteristics and procedural details of the included randomized clinical trials are summarized in Table 5. Overall 1582 patients, 797 patients treated with DES were compared to 785 patients treated with BMS, with a follow-up ranging from 18 to 60 months. No significant differences were shown in terms of all-cause mortality (risk ratio [RR], 1.13; 95% CI, 0.74–1.71; P 5 0.554), cardiovascular mortality (RR. 0.66; 95% CI, 0.19–2.27; P=0.519), myocardial infarction (RR, 0.69; 95% CI, 0.43–1.10; P= 0.123) or stent thrombosis (RR, 0.61; 95% CI, 0.27–1.41; P=0.255). However, SVG interventions with DES reduced TVR (RR, 0.52; 95% CI, 0.30–0.88; P 5 0.017) and MACE rate (RR, 0.60; 95% CI, 0.42–0.87; P 5 0.007) compared to BMSs.
Several registries have assessed the mid-term and long-term safety and effectiveness of DESs in SVGs. The Veterans Affairs CART Program explored the long-term clinical outcomes in the largest series currently published. [4545. Aggarwal V, Stanislawski MA, Maddox TM, Nallamothu BK, Grunwald G, Adams JC, Ho PM, Rao SV, Casserly IP, Rumsfeld JS, Brilakis ES, Tsai TT. Safety and effectiveness of drug-eluting versus bare-metal stents in saphenous vein bypass graft percutaneous coronary interventions: insights from the Veterans Affairs CART program. J Am Coll Cardiol. 2014;64:1825-36. ] A cohort of 2,471 post-CABG veterans undergoing SVG-PCI between 2008 and 2011 at all Veterans Affairs hospitals were retrospectively studies. The clinical outcomes of between those receiving DES and BMS were compared. Clinical outcomes included procedural complications, myocardial infarction and all-cause mortality. Comparisons were made in a propensity-matched cohort using Cox proportional hazards regression models. DESs were used in 1,549 SVG-PCI patients (63%) as the use of DES increased progressively with each calendar year (50% in 2008 to 69% in 2011). Incidence of procedural complications was low and comparable in both groups (2.8% among BMS vs. 2.3% among DES patients; p=0.54). During long-term (>2 years) follow-up, use of DES was associated with lower mortality than BMS (hazard ratio [HR]: 0.72; 95% confidence interval [CI]: 0.57 to 0.89) and similar rates of myocardial infarction (HR: 0.94; 95% CI: 0.71 to 1.24) in the propensity-matched cohort. This large retrospective series showed a widespread and increasing use of DES during SVG-PCI. In long-term follow-up, compared with BMS, DES use was safe and effective in SVG-PCI patients.
Overall, the use of DES appears to be beneficial in terms of reducing TLR in the mid-term. Although the DES benefit on the longer term appears less evident. Consistently, no safety issues such as those shown in the long-term follow up of the RRISC trial have been shown in other registries and randomized clinical trials.
As a result, larger randomized clinical trials with longer follow-up using the current available DES technology is warranted to address final conclusions to the routine use of DES on SVG interventions. The different nature of the SVG disease to the native artery may be an important consideration. Possible delayed healing of SVG treated with DES may contribute to the late catch up observed in ISAR-CABG. Therefore, dedicated DES, exploring different drug doses might be required for SVGs, since DES development has been based on observations from implants made in arterial vessels in animal models and early human studies.
In conclusion, DESs have showed superiority over BMS in the setting of SVG PCIs. The large amount of evidence obtained from large registries and meta-analyses support the routine use of DES in SVGs lesions as a safe strategy in the long-term follow up.
Drug-eluting stents (DES) versus bare metal stents (BMS) to treat saphenous vein grafts
- DES have shown to be more effective that BMS by reducing the rate of TLR
- Initial concern about DES safety was raised by the long-term follow-up of a small-randomised trial
- Long-term safety of DES is supported by a large amount of data coming from large real-world series
Value of intravascular ultrasound in vein graft interventions
Conventional angiography underestimates the severity of vein graft remodelling and atheromatous plaque development compared to IVUS [5151. Nase-Hueppmeier S, Uebis R, Doerr R, Hanrath P. Intravascular ultrasound to assess aortocoronary venous bypass grafts in vivo. Am J Cardiol. 1992;70:455-8. ]. Early SVG evaluation after surgery has shown that significant wall thickening occurs by 6 months, accompanied by compensatory enlargement and preservation of the graft luminal diameter [5252. Higuchi Y, Hirayama A, Shimizu M, Sakakibara T, Kodama K. Postoperative changes in angiographically normal saphenous vein coronary bypass grafts using intravascular ultrasound. Heart Vessels. 2002;17:57-60. ]. Atheromatous plaque can be detected by IVUS as early as 8 to 10 months post grafting in association with both expansive and constrictive remodelling [5353. Hong MK, Mintz GS, Hong MK, Abizaid AS, Pichard AD, Satler LF, Kent KM, Leon MB. Intravascular ultrasound assessment of the presence of vascular remodeling in diseased human saphenous vein bypass grafts. Am J Cardiol. 1999;84:992-8. ].
It has been demonstrated that the time course of TLR following successful SVG angioplasty appears differently from that of native vessels and continues after 1 year [5454. Hong MK, Mehran R, Dangas G, Mintz GS, Lansky A, Kent KM, Pichard AD, Satler LF, Stone GW, Leon MB. Comparison of time course of target lesion revascularization following successful saphenous vein graft angioplasty versus successful native coronary angioplasty. Am J Cardiol. 2000;85:256-8. ]. As a result, it has been suggested that intermediate lesions, better identified by IVUS, might be treated avoiding early recurrence of symptoms attributed to those lesions. As a general rule IVUS is not used before stenting in degenerated grafts to prevent embolization. If the lesion is distal in a vein graft IVUS can be used proximally to assess vessel size. At our institution, IVUS is always performed after stenting to assess results. Lack of apposition of undersized stents is frequent and is not associated with any adverse clinical event [5555. Hong YJ, Pichard DA, Mintz GS, et al. Outcome of Undersized Drug-Eluting Stents for Percutaneous Coronary Intervention of Saphenous Vein Graft Lesions. Am J Cardiol. 2010;105:179-185.
Clinical series of 209 saphenous vein graft treated lesions using ‘undersized’ drug-eluting stents. The lesions were divided into 3 groups according to the ratio of the stent diameter to the average intravascular ultrasound reference lumen diameter: group I, 1.0. The plaque intrusion area and volume were smallest in group I. The incidence of a creatine kinase-MB elevation >3 times normal was 6% in group I, 9% in group II, and 19% in group III (p = 0.025). No significant differences were found in the incidence of 1-year target lesion revascularization (group I, 13%; group II, 9%; and group III, 15%; p = 0.5) among the 3 groups.].
Value of physiology assessment in vein grafts
Fractional flow reserve has proven to improve clinical results to guide intermediate native coronary lesions in stable patients [FAME]. Nonetheless, data on functional evaluation of stenosis severity in bypass grafts are limited. In a retrospective study, Di Serafino et al. [113113. Di Serafino L, De Bruyne B, Mangiacapra F, Bartunek J, Agostoni P, Vanderheyden M, Scognamiglio G, Heyndrickx GR, Wijns W, Barbato E. Long- term clinical outcome after fractional flow reserve- versus angio-guided percutaneous coronary intervention in patients with intermediate stenosis of coronary artery bypass grafts. Am Heart J. 2013;166:110–118. ] evaluated the long-term clinical outcome of 65 patients who underwent FFR- guided PCI of intermediate lesions (between 40% and 70% diameter stenosis at a visual estimation) involving an arterial or venous graft compared to 158 patients in whom PCI of the intermediate stenosis was performed based on angiography. At the multivariate analysis, MACE and cerebrovascular events rate were lower in the FFR-guided group as compared with the angiography-guided group, with a significant overall reduction in procedural costs. Later, Almomani A. et al. communicated retrospectively the clinical outcomes of 33 patients undergoing SVG FFR evaluation compared to 532 patients undergoing native vessel FFR assessment in whom intervention was deferred based on FFR value > 0.8 [113113. Di Serafino L, De Bruyne B, Mangiacapra F, Bartunek J, Agostoni P, Vanderheyden M, Scognamiglio G, Heyndrickx GR, Wijns W, Barbato E. Long- term clinical outcome after fractional flow reserve- versus angio-guided percutaneous coronary intervention in patients with intermediate stenosis of coronary artery bypass grafts. Am Heart J. 2013;166:110–118. ]. During a median follow-up of 3.2 years major adverse cardiac events was significantly higher in the SVG group (36% vs 21%, p=0.01), driven by higher TLR (27% vs 14%, p=0.01) [114114. Almomani A, Pothineni NV, Edupuganti M, Payne J, Agarwal S, Uretsky B, Hakeem A. Outcomes of Fractional Flow Reserve-Based Deferral in Saphenous Vein Graft Narrowing. Am J Cardiol. 2018;122(5):723-728]. ]. This study indicates that deferring revascularization of intermediate SVG lesions based on classic FFR value cut-off is associated with worse clinical outcome when comparing with deferred native coronary lesions. These findings suggest that using FFR assessment in SVG lesions with threshold derived from native coronary arteries, may not be appropriate. These findings are in alignment with the concept that intermediate SVG lesions have high chance to progress and determine further events. Therefore, those lesions might be treated avoiding early recurrence of symptoms [5454. Hong MK, Mehran R, Dangas G, Mintz GS, Lansky A, Kent KM, Pichard AD, Satler LF, Stone GW, Leon MB. Comparison of time course of target lesion revascularization following successful saphenous vein graft angioplasty versus successful native coronary angioplasty. Am J Cardiol. 2000;85:256-8. ].
Strategies to prevent no-reflow in SVG interventions
PHARMACOLOGIC METHODS
In comparison to the pharmacologic methods for treating native vessel atherosclerosis, the pharmacologic methods for treating SVG atherosclerosis and disease progression are relatively limited. It does appear that aggressive low density lipoprotein-lowering therapy with statins reduces progression of SVG atherosclerosis, as evaluated by both angiography and IVUS [5656. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. The Post Coronary Artery Bypass Graft Trial Investigators. N Engl J Med. 1997;336:153-62. , 5757. Hata M, Takayama T, Sezai A, Yoshitake I, Hirayama A, Minami K. Efficacy of aggressive lipid controlling therapy for preventing saphenous vein graft disease. Ann Thorac Surg. 2009;88:1440-4. , 5858. Hong YJ, Mintz GS, Kim SW, Lee SY, Kim SY, Okabe T, Pichard AD, Satler LF, Waksman R, Kent KM, Suddath WO, Weissman NJ. Disease progression in non-intervened saphenous vein graft segments a serial intravascular ultrasound analysis. Journal of the American College of Cardiology. 2009;53:1257-64. ]. Other treatments, however, have been less successful. Glycoprotein IIb/IIIa inhibitors (GPI) might be expected to improve outcomes in patients undergoing PCI of SVGs given their potent effects upon platelet aggregation. Studies have consistently shown, however, that GPIs increase bleeding rates in SVG PCI, without any benefit to periprocedural MI or survival [5858. Hong YJ, Mintz GS, Kim SW, Lee SY, Kim SY, Okabe T, Pichard AD, Satler LF, Waksman R, Kent KM, Suddath WO, Weissman NJ. Disease progression in non-intervened saphenous vein graft segments a serial intravascular ultrasound analysis. Journal of the American College of Cardiology. 2009;53:1257-64. ]. Similarly, intracoronary vasodilators (e.g., adenosine, sodium nitroprusside, nicardipine) are expected to improve microvascular spasm associated with the no-reflow phenomenon. Although studies have shown that such vasodilators can improve angiographic flow, they do not appear to improve ischaemic outcomes [6363. Fischell TA, Carter AJ, Foster MT, Hempsall K, DeVries J, Kim DH, Kloostra A. Reversal of “no reflow” during vein graft stenting using high velocity boluses of intracoronary adenosine. Cathet Cardiovasc Diagn. 1998;45:360-5. , 6464. Sdringola S, Assali A, Ghani M, Yepes A, Rosales O, Schroth GW, Fujise K, Anderson HV, Smalling RW. Adenosine use during aortocoronary vein graft interventions reverses but does not prevent the slow-no reflow phenomenon. Catheter Cardiovasc Interv. 2000;51:394-9. , 6565. Resnic FS, Wainstein M, Lee MK, Behrendt D, Wainstein RV, Ohno-Machado L, Kirshenbaum JM, Rogers CD, Popma JJ, Piana R. No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention. Am Heart J. 2003;145:42-6. ].
COVERED STENTS
“Covered” stents initially held some promise as a strategy for prevention of distal embolization during PCI in SVGs, as it was theorised that they might trap friable plaque between the stent and the SVG. Such stents are usually covered with polytetrafluoroethylene (PTFE), and as such might prevent plaque prolapse through stent struts. This theory, however, proved false; PTFE-covered stents, in comparison to BMSs, did not reduce the amount of embolic debris retrieved by the FilterWire™ (Boston Scientific, Natick, MA, USA) during SVG PCI [6666. Blackman DJ, Choudhury RP, Banning AP, Channon KM. Failure of the Symbiot PTFE-covered stent to reduce distal embolization during percutaneous coronary intervention in saphenous vein grafts. J Invasive Cardiol. 2005;17:609-12. ]. Even more, The Randomised Evaluation of polytetrafluoroethylene COVERed stent in Saphenous vein grafts (RECOVERS) trial showed a higher rate of major adverse of cardiac events in patients receiving PTFE-covered stents versus BMSs [6767. Stankovic G, Colombo A, Presbitero P, van den Branden F, Inglese L, Cernigliaro C, Niccoli L, Bartorelli AL, Rubartelli P, Reifart N, Heyndrickx GR, Saunamäki K, Morice MC, Sgura FA, Di Mario C. Randomized evaluation of polytetrafluoroethylene-covered stent in saphenous vein grafts: the Randomized Evaluation of polytetrafluoroethylene COVERed stent in Saphenous vein grafts (RECOVERS) Trial. Circulation. 2003;108:37-42. ]. This result was echoed by the BARRICADE trial, which randomised patients undergoing SVG PCI to BMS vs. the PTFE-covered JOSTENT (Abbott Vascular, Abbott Park, IL). This study showed a higher rate of major adverse cardiac events with the covered stent, and as such was terminated prematurely [6868. Stone GW, Goldberg S, Mehran R. A prospective, randomized US trial of the PTFE covered JOSTENT for the treatment of diseased saphenous vein grafts: the BARRICADE trial (abstr). J Am Coll Cardiol. 2005;45 Suppl A:27A. ]. A different iteration of a PTFE-covered stent, the self-expanding Symbiot™ stent (Boston Scientific, Natick, MA, USA) also failed to show any advantage over BMSs in SVG PCI, despite a relatively high-risk population [6969. Turco MA, Buchbinder M, Popma JJ, Weissman NJ, Mann T, Doucet S, Johnson WL Jr, Greenberg JD, Leadley K, Russell ME. Pivotal, randomized US study of the Symbiottrade mark covered stent system in patients with saphenous vein graft disease: eight-month angiographic and clinical results from the Symbiot III trial. Catheter Cardiovasc Interv. 2006;68:379-88. ]. This is in concert with data showing a much higher risk of stent thrombosis and restenosis with PTFE-covered stents in general [7070. Gercken U, Lansky AJ, Buellesfeld L, Desai K, Badereldin M, Mueller R, Selbach G, Leon MB, Grube E. Results of the Jostent coronary stent graft implantation in various clinical settings: procedural and follow-up results. Catheter Cardiovasc Interv. 2002;56:353-60. ]. Thus, the routine use of PTFE-covered stents in the treatment of SVGs cannot be recommended. Nonetheless, preliminary clinical experience using a dedicated system MGuardTM (InspireMD, Tel Aviv, Israel), comprising a BMS platform with a polymeric net attached to its surface, appears as a new strategy to prevent distal embolization and no-reflow in SVG PCI, which must be proven in larger clinical studies [7171. Maia F, Costa JR Jr, Abizaid A, Feres F, Costa R, Staico R, Siqueira D, Esteves V, Sousa A, Sousa JE. Preliminary results of the INSPIRE trial with the novel MGuard stent system containing a protection net to prevent distal embolization. Catheter Cardiovasc Interv.
76:86-92].
EMBOLIC PROTECTION DEVICES
Specific strategies to reduce distal embolization have been developed. In particular, the “mechanical” protection of the vasculature distal to the treated lesion appeared as a good approach to reduce the downstream spreading of material during the intervention on the graft lesion. So far, 3 typologies of devices have been developed with this scope.
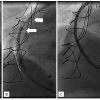
The first to be tested in SVGs is a distal occlusion device ( Figure 3). Its mechanism is as follows. A compliant balloon is positioned distal to the lesion before the PCI and is inflated at low pressure during the procedure. Suction of the stagnant blood/debris is done just after the PCI using an aspiration catheter inserted through the guiding catheter, and the balloon is then deflated. In the randomised Saphenous Vein Graft Angioplasty Free of Emboli Randomised (SAFER) trial including 801 patients, this device was shown to significantly reduce the incidence of major adverse clinical events at 30 days (9.6% vs. 16.5%, p=0.004) compared to the simple implantation of BMSs without distal protection. This benefit was largely driven by a reduction in the rate of periprocedural MI [7272. Baim DS, Wahr D, George B, Leon MB, Greenberg J, Cutlip DE, Kaya U, Popma JJ, Ho KK, Kuntz RE. Saphenous vein graft Angioplasty Free of Emboli Randomized (SAFER) Trial Investigators; Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts. Circulation. 2002;105:1285-90.
The SAFER trial was the first multicenter randomized trial to evaluate use of a distal embolic protection device during stenting of SVG lesions. Of 801 eligible patients, 406 were randomly assigned to stent placement over the shaft of the distal protection device, and 395 were assigned to standard stent placement. Patients assigned to use of embolic protection device had significantly reduced incidence of major adverse clinical events at 30 days (9.6% versus 16.5%, p=0.004) compared to the simple implantation of BMSs without distal protection. This benefit was largely driven by a reduction in the rate of periprocedural myocardial infarction.]. Some concerns were raised related to the safety of low-pressure inflation of a non-compliant balloon on the SVG vessel wall distal to the lesion to be treated [7373. Wu CJ, Yang CH, Fang CY, Chang HW, Chen SM, Hung WC, Chen CJ, Cheng CI, Chen YH, Chai HT, Yip HK. Six-month angiographic results of primary angioplasty with adjunctive PercuSurge GuardWire device support: evaluation of the restenotic rate of the target lesion and the fate of the distal balloon occlusion site. Catheter Cardiovasc Interv. 2005;64:35-42. ]. However, it has been proven in an angiographic study that this inflation, carefully performed in a non-angiographic diseased tract of the SVG, is safe and does not produce any major vascular effect acutely and at 6 month follow up [7474. Agostoni P, Vermeersch P, Vydt T, Debrauwere J, Van den Heuvel P, Convens C, Van den Branden F, Verheye S, Van Langenhove G. Acute and mid-term local vascular effects of compliant balloon inflation (GuardWire system) on saphenous vein bypass grafts: an angiographic analysis. Int J Cardiol. 2007;120:227-31. ]. A second distal occlusion device has also been tested effectively and is available on the market [7575. Carrozza JP Jr, Mumma M, Breall JA, Fernandez A, Heyman E, Metzger C. Randomized evaluation of the TriActiv balloon-protection flush and extraction system for the treatment of saphenous vein graft disease. J Am Coll Cardiol. 2005;46:1677-1683. ].
Distal filters have the same rationale but a different mechanism of action with respect to the distal occlusion device( Figure 4). They are constituted of a porous filter, which is placed distally to the lesion before the PCI in order to collect embolic material and retrieve it after the procedure. Their value has been proven in the FilterWire Randomized Evaluation (FIRE) trial another large randomised study, enrolling 651 patients, in which the filter has been shown to be non-inferior to the previously described “occlusion and aspiration” system. The major adverse clinical event rate at 30 days was respectively 9.9% vs. 11.6% (p for non-inferiority=0.0008) [7676. Stone GW, Rogers C, Hermiller J, Feldman R, Hall P, Haber R, Masud A, Cambier P, Caputo RP, Turco M, Kovach R, Brodie B, Herrmann HC, Kuntz RE, Popma JJ, Ramee S, Cox DA. Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts. Circulation. 2003;108:548-53. ]. Several filters have been released recently on the market, some with proven non-inferiority as compared with the first devices released [7777. Kereiakes DJ, Turco MA, Breall J, Farhat NZ, Feldman RL, McLaurin B, Popma JJ, Mauri L, Zimetbaum P, Massaro J, Cutlip DE, AMEthyst Study Investigators. A novel filter-based distal embolic protection device for percutaneous intervention of saphenous vein graft lesions: results of the AMEthyst randomized controlled trial. JACC Cardiovasc Interv. 2008;1:248-257. , 7878. Dixon SR. Saphenous vein graft protection in a distal embolic protection randomized trial. Presented at Transcatheter Cardiovascular Therapeutics. 2005, Washington, DC, October 2005. ], some without clear evidence of benefit [7979. Dixon SR, Mann JT, Lauer MA, Casale PN, Dippel EJ, Strumpf RK, Feldman RL, Shear W, Resar JR, Zimmer SD, O’Neill WW, TRAP Investigators. A randomized, controlled trial of saphenous vein graft intervention with a filter-based distal embolic protection device: TRAP trial. J Interv Cardiol. 2005;18:233-2341. , 8080. Holmes DR, Coolong A, O’Shaughnessy C, Chauhan M, Van Langenhove G, Hall P, Vermeersch P, Verlee P, Popma JJ, Cutlip D, Kuntz RE. Comparison of the CardioShield filter with the guardwire balloon in the prevention of embolisation during vein graft intervention: results from the CAPTIVE randomised trial. EuroIntervention. 2006;2:161-168. ].
The last type is the proximal protection device. This is a catheter with a proximal protection balloon which is inflated temporarily, proximal to the lesion to treat, occluding blood flow and creating a column of stagnant blood, so that the debris dislodged during the PCI can then be aspirated from the vessel through the same catheter. Proximal protection device is currently abandoned and not used anymore.
In the light of these results, embolic protection devices are currently accepted as standard therapy for the prevention of distal embolization during percutaneous treatment of SVG disease. Despite this large body of evidence, protection devices remain underutilised (<25% of SVGs treated with PCI) in daily practice [8282. Mehta SK, Frutkin AD, Milford-Beland S, Klein LW, Shaw RE, Weintraub WS, Krone RJ, Anderson HV, Kutcher MA, Marso SP. Utilization of distal embolic protection in saphenous vein graft interventions (an analysis of 19,546 patients in the American College of Cardiology-National Cardiovascular Data Registry). Am J Cardiol. 2007;100:1114-8. , 9393. Brennan JM, Al-Hejily W, Dai D, Shaw RE, Trilesskaya M, Rao SV, Brilakis ES, Anstrom KJ, Messenger JC, Peterson ED, Douglas PS, Sketch MH Jr. Three-Year Outcomes Associated With Embolic Protection in Saphenous Vein Graft Intervention: Results in 49 325 Senior Patients in the Medicare-Linked National Cardiovascular Data Registry CathPCI Registry. Circ Cardiovasc Interv. 2015 Mar;8(3). ]. The elevated costs of these devices seem to be a major explanation for their low utilisation. Moreover, the need for a learning curve in order to use these devices properly can also play a role in the speed of their adoption in clinical practice. We recommend that operators select a couple of embolic protection devices they can use on a regular basis in order to build up experience and confidence to use them.
Although, the described evidence favors the routine use of EPD during SVG PCI, the use of distal EPDs is technically not possible in many distal and tortuous grafts, increasing the risk of both distal dissections and device entrapment. As a result, most of SVGs are frequently treated without EPD use [4646. Mehta SK, Frutkin AD, Milford-Beland S, Klein LW, Shaw RE, Weintraub WS, Krone RJ, Anderson HV, Kutcher MA, Marso SP. Utilization of distal embolic protection in saphenous vein graft interventions (an analysis of 19546 patients in the American College of Cardiology-National Cardiovascular Data Registry). Am J Cardiol. 2007;100:1114–1118. ]. In addition, the results of a large contemporary US based EDP registry CathPCI (n=49,325) [9393. Brennan JM, Al-Hejily W, Dai D, Shaw RE, Trilesskaya M, Rao SV, Brilakis ES, Anstrom KJ, Messenger JC, Peterson ED, Douglas PS, Sketch MH Jr. Three-Year Outcomes Associated With Embolic Protection in Saphenous Vein Graft Intervention: Results in 49 325 Senior Patients in the Medicare-Linked National Cardiovascular Data Registry CathPCI Registry. Circ Cardiovasc Interv. 2015 Mar;8(3). ] and a recently published meta-analysis [115115. Paul TK, Bhatheja S, Panchal HB, Zheng S, Banerjee S, Rao SV, Guzman L, Beohar N, Zhao D, Mehran R, Mukherjee D. Outcomes of Saphenous Vein Graft Intervention With and Without Embolic Protection Device: A Comprehensive Review and Meta-Analysis. Circ Cardiovasc Interv. 2017;10(12):e005538]. ] which includes 8 studies (n=52,893) reported no benefit on the routine use of EDP. The CathPCI registry involved senior patients, finding that EPDs were used more commonly among patients with high-risk clinical indications, however, no acute- or long-term benefit to routine EPD use in SVG coronary intervention were seen, despite adjustment for differences in patient characteristics. The described meta-analysis showed no difference in all-cause mortality, major cardiovascular events, TVR and MI. Contrary to expectations, the use of EPD was associated with 1.5-fold higher rate of periprocedural MI. As a result, we warranted selective use of EPDs in high-risk graft interventions, while further randomized evaluations of EPDs in contemporary practice are conducted.
DIRECT & UNDERSIZED STENTING APPROACH
We previously reported the clinical benefit of direct stenting on SVGs compared to conventional stenting [8383. Leborgne L, Cheneau E, Pichard A, Ajani A, Pakala R, Yazdi H, Satler L, Kent K, Suddath WO, Pinnow E, Canos D, Waksman R. Effect of direct stenting on clinical outcome in patients treated with percutaneous coronary intervention on saphenous vein graft. Am Heart J. 2003;146:501-6. ]. Later we communicated the excellent clinical outcome using this strategy and suggested that it seemed as effective as distal protection in patients undergoing SVG interventions [8484. Okabe T, Lindsay J, Torguson R, Steinberg DH, Roy P, Slottow TL, Kaneshige K, Xue Z, Satler LF, Kent KM, Pichard AD, Waksman R. Can direct stenting in selected saphenous vein graft lesions be considered an alternative to percutaneous intervention with a distal protection device?. Catheter Cardiovasc Interv. 2008;72:799-803. ]. Recently we reported the initial results on SVG lesions treated with DESs (n=209), including the “undersized” stenting approach (n=71), defined as stent diameter <10% of the average reference lumen diameter [5555. Hong YJ, Pichard DA, Mintz GS, et al. Outcome of Undersized Drug-Eluting Stents for Percutaneous Coronary Intervention of Saphenous Vein Graft Lesions. Am J Cardiol. 2010;105:179-185.
Clinical series of 209 saphenous vein graft treated lesions using ‘undersized’ drug-eluting stents. The lesions were divided into 3 groups according to the ratio of the stent diameter to the average intravascular ultrasound reference lumen diameter: group I, 1.0. The plaque intrusion area and volume were smallest in group I. The incidence of a creatine kinase-MB elevation >3 times normal was 6% in group I, 9% in group II, and 19% in group III (p = 0.025). No significant differences were found in the incidence of 1-year target lesion revascularization (group I, 13%; group II, 9%; and group III, 15%; p = 0.5) among the 3 groups.]. We observed that the undersized stenting approach was associated with a reduction in frequency of post-procedural CK-MB elevation, significant less plaque prolapse showed by IVUS, and no increase in the rate of 1-year TLR. As shown in the Illustrative Case 1, this approach usually implies adequate expansion of an intentionally undersized stent, which may leave areas of malapposition, as better demonstrated by optical coherence tomography technology. The “undersized stenting” strategy to treat SVGs could be particularly attractive when embolic protection devices are not available or cannot be used.
Strategies to prevent no-reflow in SVG interventions
- Pharmacology
- glycoprotein IIb/IIIa inhibitors increase the rate of bleeding without any apparent benefit
- vasodalitors can improve angiographic results but do not appear to improve clinical outcomes
- Covered stents
- their use has been linked to worse outcomes in several randomised trials
- use not recommended
- Embolic protection devices
- strategy that might decreases periprocedural myocardial infarction and the no-reflow phenomenon
- routine use is recommended in selected high-risk interventions
- both proximal and distal protection devices should be available and used according to disease location in the graft itself
- Direct and undersized stenting
- alternative approach to prevent distal embolization
Acute myocardial infarction due to saphenous vein grafts
The long-term outcomes of patients presenting with an acute MI from an SVG remains particularly poor and there is little prospective data to guide treatment strategies. Primary PCI of a SVG for acute MI appears to be independently associated with adverse cardiac events [8585. Al Suwaidi J, Velianou JL, Berger PB, Mathew V, Garratt KN, Reeder GS, Grill DE, Holmes DR Jr. Primary percutaneous coronary interventions in patients with acute myocardial infarction and prior coronary artery bypass grafting. Am Heart J. 2001;142:452-9. ]. In a series of 57 patients with ST-elevation MI (STEMI) from an SVG culprit, Brodie et al reported in-hospital mortality of 21.1%, with 46% of culprit SVGs occluded at 1 year and 51% of patients deceased at 10 years [8686. Brodie BR, VerSteeg DS, Brodie MM, Hansen C, Richter SJ, Stuckey TD, Gupta N, Pulsipher M, Downey W. Poor long-term patient and graft survival after primary percutaneous coronary intervention for acute myocardial infarction due to saphenous vein graft occlusion. Catheter Cardiovasc Interv. 2005;65:504-9. ]. Although, more contemporary data suggests that acute results have improved but the long-term prognosis remains poor. [9494. Kohl LP, Garberich RF, Yang H, Sharkey SW, Burke MN, Lips DL, Hildebrandt DA, Larson DM, Henry TD. Outcomes of primary percutaneous coronary intervention in ST-segment elevation myocardial infarction patients with previous coronary bypass surgery. JACC Cardiovasc Interv. 2014;7:981-7. ]
The role of thrombectomy for acute MI due to a SVG culprit also remains unclear. Initial studies established the feasibility of aspiration thrombectomy before primary PCI for STEMI, showing that this strategy reduced CK-MB release and microvascular obstruction and improved angiographic flow [8787. Burzotta F, Trani C, Romagnoli E, Mazzari MA, Rebuzzi AG, De Vita M, Garramone B, Giannico F, Niccoli G, Biondi-Zoccai GG, Schiavoni G, Mongiardo R, Crea F. Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus-aspiration in primary and rescue angioplasty (REMEDIA) trial. Journal of the American College of Cardiology. 2005;46:371-6. , 8888. Silva-Orrego P, Colombo P, Bigi R, Gregori D, Delgado A, Salvade P, Oreglia J, Orrico P, de Biase A, Piccalò G, Bossi I, Klugmann S. Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study. Journal of the American College of Cardiology. 2006;48:1552-9. , 8989. Galiuto L, Garramone B, Burzotta F, Lombardo A, Barchetta S, Rebuzzi AG, Crea F. Thrombus aspiration reduces microvascular obstruction after primary coronary intervention: a myocardial contrast echocardiography substudy of the REMEDIA Trial. Journal of the American College of Cardiology. 2006;48:1355-60. ]. These initial studies did not specifically include SVG culprits. The Thrombus Aspiration during Percutaneous intervention in Acute Coronary myocardial infarction Study (TAPAS) also examined aspiration thrombectomy for STEMI, showing a reduction in cardiac death and non-fatal MI at 1 year when compared to conventional PCI [9090. Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915-20. ]. TAPAS did not exclude SVG culprits, but included only about 2% “other” culprit vessels. This makes conclusions about the utility of thrombectomy in STEMI due to SVG difficult. Given that angiographically visible thrombus appears to be associated with more benefit of aspiration thrombectomy, [9191. Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557-67. ] one would intuitively expect this technique to be of some benefit in thrombus-prone SVGs. Comparisons of aspiration thrombectomy in SVGs to either conventional primary PCI or embolic protection devices are not available. An initial clinical experience in 20 patients presenting with non-STEMI and occluded SVG reported good results with a multi-staged PCI strategy after initial SVG recanalisation using small balloons followed by anticoagulation plus GPIs for several days [9292. Fiorina C, Meliga E, Chizzola G, Curello S, Tayeh O, Vizzardi E, Dei Cas L, Ettori F. Early experience with a new approach for percutaneous intervention of totally occluded saphenous vein graft: is the flow the best thrombolytic?. EuroIntervention.
6:461-6]. The authors claimed that this approach allowed a decrease in the thrombus burden prior to definitive stenting, thereby reducing the incidence of distal embolization and improving outcomes.
Acute myocardial infarction due to saphenous vein grafts
- High related in-hospital mortality and poor long-term prognosis
- Possible role of aspiration thrombectomy – especially in the presence of visible thrombus
- Possible role of staged procedure after aggressive pharmacology approach
Technical aspects
When dealing with a SVG lesion, pharmacological pre-treatment of the patient is extremely important. Dual antiplatelet therapy (with a thienopyridine given upfront) and statins are mandatory, unless clearly contraindicated. The use of GPIs, in cases of acute MI due to acute graft closure, is still suggested but their effectiveness in this setting is uncertain.
Choosing the correct guiding catheter is the first important step. In our experience, for the vein graft to the right coronary artery, originating most of the time from the right anterior surface of the aorta, the multipurpose catheter has the best alignment and support when performing the procedure either via the femoral or the radial artery. Engagement of the catheter can be performed in the left anterior oblique view. For vein grafts originating from the left anterior surface (usually to the left anterior descending/diagonal or marginal/circumflex arteries), we prefer Judkins right (Cordis, Johnson & Johnson, Warren, NJ, USA) or left coronary bypass catheters (the best fitting catheter can be tested during the diagnostic angiography) in case of femoral access. If additional support is needed, Amplatz left catheters can be used, but optimal support is obtained with the MP1 guide (Medtronic) that has a long nose, so it gets support in the opposite wall of the aorta, does not “fall” when pushed, and provides coaxial access to the SVG. Engagement is feasible in the right anterior oblique view. When approaching these bypasses via the radial approach, we strongly recommend avoiding the right radial artery, instead choosing the left radial artery. Guiding catheters of choice can be extra-back up shaped, multipurpose with a long distal arm (MP1), or Amplatz left catheters. Sometimes vein grafts to the circumflex originate from the posterior surface of the aorta. In this case, Amplatz left or multipurpose guiding catheters are preferred. Also in this case engagement is performed in the right anterior oblique view.
Embolic protection devices should be advocated in high-risk SVG procedure unless the “undersized stent strategy” is used (see above). However, for economic reasons, they can be dispensed with in cases of very focal lesions in small (<3.5 mm) grafts. In this case, a soft-tip coronary guide wire and direct stenting without pre-dilatation and post-dilatation should be the recommended strategy. Choosing the type of protection device depends mainly on the location of the lesion and on the operator’s personal experience with the device. In the case of lesions in the mid body of the graft, any type of protection device is usable. However, proximal devices give the hypothetical advantage of a protection before any type of intervention, even the simple crossing with the coronary guidewire. On the contrary, in cases of proximal or ostial lesions, distal protection devices should be recommended. In cases of distal lesions, a proximal protection device fits better. The theoretical background for these choices relies on the fact that every protection device needs a vein graft disease-free landing zone of around 3 cm to 5 cm.
When using occlusion protection devices, the control of complete vessel occlusion is needed. This means that a column of stagnant blood (checked with contrast) should be evident once the device is in place. If a filter is used, we recommend securing good deployment of the filter (good apposition to the vessel wall) in two orthogonal views. We always recommend direct stenting, and in case the stent remains significantly under-deployed, post-stent high-pressure dilatation with an undersized balloon must be done with a protection device in place.
Once the stenting procedure is finished, attention should be given to the collection of debris from the protection device. With proximal device placement, direct aspiration of at least 5 cc of blood from the device should be performed before releasing the occlusion. In case of distal occlusion device use, the specific manual aspiration device should be used, and 2 syringes of 20 cc of blood should be aspirated. If a filter is used, careful, complete closure of the filter is necessary before retrieval. We recommend performing the complete procedure under fluoroscopy. Final angiographic control of the stenting procedure without a device in place is mandatory in at least two orthogonal views.
Conclusions
Percutaneous intervention in SVGs remains challenging and carries a higher risk of poor outcome than in native coronary vessels, despite the advances in embolic protection and pharmacotherapy. PCI is usually preferred over repeat CABG for early recurrent symptoms after CABG (<3 years). However, most symptomatic patients present later with extensive native and graft disease. In this setting, the revascularisation strategy must be based on careful risk/benefit assessment of the procedure and the local experience. Although, protection devices for distal embolization improves outcomes, particularly in difficult setting, in many cases those devices are not utilised, or cannot be used. Their current utility has been questioned. Therefore, novel percutaneous approaches and further research are certainly merited in this field. Early and aggressive statin therapy appears to be an effective strategy to improve SVG durability and clinical outcomes.
Personal perspective - Augusto D. Pichard
Percutaneous SVG interventions represent a major challenge for the interventionist because of complications and their relation to poor outcome. Interventions must be based on good clinical judgment taking into consideration the clinical presentation, the patient’s age, associated comorbidities, and a meticulous analysis of the native coronary and graft anatomy. The main emphasis must be placed on preventing distal embolization during the intervention. The use of undersized stents for large, degenerated SVG’s is an effective strategy. The recent improvements in PCI for native total occlusions opens a new treatment approach for degenerated SVGs: opening the chronic native totally occluded vessel instead. However, we anticipate improvements in the natural history of SVG disease due to the important advances made in medical therapy and in the harvesting vein technique, as well as improvements in PCI of SVGs related to minimisation of distal embolization and the use of DES. Further research is certainty required in this interesting field.