Summary
Non-invasive imaging modalities have almost entirely replaced diagnostic peripheral angiography in everyday clinical practice. However, catheter-based angiography remains the procedure of choice in case of inconclusive imaging results or as a foundation for an endovascular revascularisation procedure. A patient’s history of previous endovascular or surgical revascularisation procedures, as well as the clinical presentation and non-invasive imaging results, should be integrated in the planning of an angiographic study with respect to choice of access site, sheath size, and catheters. The specific technicalities of catheterisation for each peripheral territory – lower extremities, visceral arteries, supra-aortic vessels and upper extremities – are described. Complications of peripheral diagnostic angiography are rare and mainly related to access site management, inappropriate manipulation of wires or catheters, and use of nephrotoxic iodinated contrast agents.
Introduction
The purpose of this chapter is to provide an overview of the technical aspects of catheterisation of the peripheral vasculature, including the supra-aortic vessels, the visceral organs (i.e., renal arteries, coeliac trunk and mesenteric arteries), and the upper and lower extremities. General aspects of catheterisation of the peripheral vasculature as well as the vessel anatomy are described in  View chapter. Thanks to the good performance of noninvasive imaging modalities such as duplex ultrasound (US), computed tomography angiography (CTA) and magnetic resonance angiography (MRA), catheter-based angiography is rarely performed for diagnostic purposes alone. However, in the presence of a discrepancy between clinical presentation and the results of noninvasive imaging or of inconclusive noninvasive assessment, patients should undergo catheter angiography. Furthermore, all interventionists should be familiar with the detail of invasive angiography, because it remains the foundation for any endovascular revascularisation procedure.
View chapter. Thanks to the good performance of noninvasive imaging modalities such as duplex ultrasound (US), computed tomography angiography (CTA) and magnetic resonance angiography (MRA), catheter-based angiography is rarely performed for diagnostic purposes alone. However, in the presence of a discrepancy between clinical presentation and the results of noninvasive imaging or of inconclusive noninvasive assessment, patients should undergo catheter angiography. Furthermore, all interventionists should be familiar with the detail of invasive angiography, because it remains the foundation for any endovascular revascularisation procedure.
The following principles apply to vascular access and angiography of the peripheral circulation (see Focus box 1):
- Due to the multiple vascular access sites available (e.g., femoral, radial, brachial), angiography can be performed with success in virtually all patients, even in the presence of extensive vascular disease. However, the risk related to the procedure may increase when faced with an unfavourable access site, advanced atherosclerosis, or complex catheter manipulations.
- Whenever possible, diseased vascular segments should not be used for access because of the increased rate of vascular complications.
- In patients with end-stage renal disease – independently of whether they are or not on dialysis or transplanted – upper extremity access should be avoided whenever possible in order not to jeopardise functioning arteriovenous fistulas or future fistula options. Importantly, however, this access point must not be regarded as an absolute contraindication to angiography if there are no alternatives.
- Operators, should be aware that, although not absolutely contraindicated, vascular access gained through a prosthesis (e.g., aorto-bifemoral prosthesis) may result in difficult haemostasis and thus may entail a higher rate of access-related complications than in the native circulation.
Complications of contrast angiography in the peripheral circulation are usually related either to access or to contrast agents or else they are the consequence of catheter manipulation (i.e., vessel dissection and distal embolisation). While  View chapter includes access site complications, and contrast-induced nephropathy is described in
View chapter includes access site complications, and contrast-induced nephropathy is described in  View chapter, specific risks associated with diagnostic peripheral angiography in the different vascular beds are detailed below.
View chapter, specific risks associated with diagnostic peripheral angiography in the different vascular beds are detailed below.
Basic principles of peripheral angiography
- Angiography can be performed in virtually all patients
- Procedural complications may increase in patients with advanced atherosclerosis
- Whenever possible, diseased vascular segments should not be used for vascular access
- In patients with end-stage renal disease upper extremity access should be avoided whenever possible
- Vascular access gained through prosthesis should be performed with caution
- Complications are related either to access or to contrast agents, or are the consequence of catheter manipulations
Techniques of peripheral angiography
CATHETERS
Knowledge of appropriate catheter equipment, projections and injection rates is of paramount importance in order to perform safe and high-quality vascular angiography. Diagnostic 5 Fr catheters are commonly used for this purpose because, compared to catheters requiring larger sheath sizes, they allow for optimal vascular opacification while minimising vascular access as well as catheter-related complications.
Side-hole catheters
These catheters have one or more (typically multiple) side holes along their distal portion. This configuration allows for safe injections of large volumes of contrast at a rapid rate (e.g., with power injectors) while the likelihood of catheter whipping or vessel damage is minimised. Side-hole catheters may also be very useful to determine the haemodynamic relevance of angiographically borderline stenosis. To avoid false gradient generation, especially in small calibre vessels, a 4 Fr diagnostic catheter may be progressively pulled back across the lesion in order to detect a significant pressure gradient. Although there is no consensus, a systolic pressure gradient >10-20 mmHg is generally accepted as haemodynamically relevant. This pressure gradient approach is mostly used at the aorto-iliac level where pressures are easily measured without major catheter-induced artefacts.
End-hole catheters
Simple curve and complex reverse curve catheters enable selective vessel angiography by manual contrast injection into the vessel. Care should be taken not to inject contrast into the vessel wall as this may lead to intimal dissection or distal embolisation of plaque material. To that end it is helpful to connect the catheter to a pressure line before contrast injection. A normal pressure curve reduces the risk of direct contact of the catheter tip with the vessel wall. In the absence of a pressure line, gentle injection of a small amount of contrast should be performed in order to localise the catheter tip position before image acquisition.
CONTRAST AGENTS
Low-osmolar or, better still, iso-osmolar agents are preferred in peripheral vascular contrast studies. In many centres the iso-osmolar agent iodixanol (Visipaque®) is considered the preferred contrast agent for peripheral vascular angiography and interventions. Although the advantage over low-osmolar products (e.g., iopamidol [Iopamiro®], iohexol [Accupaque®]) in terms of renal protection is still a matter of debate, iodixanol gives adequate image quality and at the same time it is better tolerated in terms of muscular pain following selective injection in the extremities. As an alternative, a low-osmolar contrast agent may be diluted with NaCl 0.9% at a one-to-one ratio. While this approach is feasible for lower and upper extremities selective injections, the quality of the images obtained is generally insufficient for aortography or pelvic angiograms. Contrast agents and contrast-related complications are detailed in  View chapter. In brief, for patients presenting with moderate to severe renal insufficiency, a 24-hour pre- and post-hydration with 0.9% or 0.45% NaCl should be prescribed. This precaution is by far the most effective one in reducing contrast medium induced nephropathy. In patients at high risk of developing contrast medium induced nephropathy, checking serum creatinine 48-72 hours after the procedure is recommended. Importantly, the amount of contrast medium administered, together with the baseline renal function, are the most important factors causing post-procedural renal failure. Therefore, in patients with renal insufficiency operators should apply the simple rule “as little contrast medium as possible, as much as is necessary”. Additional measures to limit the amount of contrast include the use of digital subtraction angiography (DSA), as detailed below, and the injection of diluted contrast.
View chapter. In brief, for patients presenting with moderate to severe renal insufficiency, a 24-hour pre- and post-hydration with 0.9% or 0.45% NaCl should be prescribed. This precaution is by far the most effective one in reducing contrast medium induced nephropathy. In patients at high risk of developing contrast medium induced nephropathy, checking serum creatinine 48-72 hours after the procedure is recommended. Importantly, the amount of contrast medium administered, together with the baseline renal function, are the most important factors causing post-procedural renal failure. Therefore, in patients with renal insufficiency operators should apply the simple rule “as little contrast medium as possible, as much as is necessary”. Additional measures to limit the amount of contrast include the use of digital subtraction angiography (DSA), as detailed below, and the injection of diluted contrast.
ACQUISITION SETTINGS
For the adequate angiographic assessment of the peripheral vasculature, and particularly of the lower extremities, it is useful to have an image intensifier larger than the one commonly used for coronary angiography (i.e., 30-40 cm/12-16 inches). However, smaller intensifiers do not preclude high-quality peripheral angiography. While a small image field allows for a better visualisation of vascular details, more angiographic runs, and therefore higher radiation doses and contrast medium quantities, are necessary to visualise the extremities. Digital subtraction angiography (DSA) is very useful but not mandatory for peripheral angiography and interventions, with the exception of carotid and vertebral circulation procedures for which DSA is essential. While general aspects of catheterisation of the peripheral vasculature as well as the vessel anatomy are described in  View chapter , we will concentrate on the technical aspects of catheterisation of the peripheral vasculature.
View chapter , we will concentrate on the technical aspects of catheterisation of the peripheral vasculature.
For peripheral angiography and interventions performed in the cardiac catheterisation laboratory, the standard “head position” of the image intensifier/flat-panel detector can be used to study the supra-aortic and the upper extremity vessels, as well as the thoracic and abdominal aorta, while “left side” or “right side” positions are used for pelvic and lower extremity procedures. Below-the-knee angiography and interventions in tall patients (i.e., >1.80m [5.9 feet]) require special attention. Accordingly, depending on the type of facility, the patient may need to be repositioned on the table more cranially (towards the head) or to have the knees flexed mildly in order to obtain complete visualisation of the foot circulation. In addition, the positioning of the patient on the catheterisation table for lower limb interventions is dependent on the target segment and the access route. For example, in the case of an antegrade femoral approach, many operators prefer to place the patient “upside down” (= feet first) in order to maintain a comfortable operator position, while limiting the radiation exposure.
The settings for the examination (e.g., frame rate, type of acquisition) are commonly adapted to the different vascular territories using preset vascular software packages ( Table 1 ). The frame rate for peripheral angiography is generally set at 2-3 frames/sec for aortic or supra-aortic acquisitions while it is commonly decreased for upper and lower extremity angiography: 1 frame/sec for upper extremity angiography and for lower extremity angiography at the femoropopliteal level, while 0.5-1 frame/sec is sufficient for below-the-knee acquisitions. For static vascular structures, DSA is the preferred invasive imaging modality. However, DSA angiography requires that the patient remains immobile during image acquisition to avoid artefacts. In addition, for abdominal aortography, patients should be able to hold their breath. Therefore, in patients unable to breath-hold sufficiently, one might consider performing standard cine-angiography with a high-frame count (i.e., 10-15 frames/sec for abdominal angiographies and 7.5-10 frames/sec for lower extremities) instead of DSA.
Fluoroscopic and cine-angiography series can be stored as memory in the background of a live fluoroscopic image (‘’picture-in-picture’’) along with the road-map and overlay trace subtract functions respectively. This may improve the safety of angiography – for example, during wire and catheter advancement for selective angiography ( for details on these imaging modalities,  View chapter ).
View chapter ).
PREVENTION OF COMPLICATIONS
Other than access site complications, described in  View chapter , adverse events related to peripheral diagnostic angiography are rare and mostly concern inappropriate manipulation of wires or catheters, and power injections performed with automatic injectors (Focus box 2). Catheters should always be advanced over a wire. Before performing contrast injection, the catheter tip should be fluoroscopically screened to ensure that is free, in order to prevent injection-related vessel wall dissections or embolisation of plaque material. An invasive pressure measurement at the catheter tip is helpful to exclude contact between the tip and the vessel wall. If diagnostic catheters are advanced over hydrophilic 0.035” wires, the latter should be handled with caution because they may lead to inadvertent vessel wall dissection or perforation through the loss of tactile feedback. High-flow injections delivered by power injectors should be performed using catheters with multiple-side-hole (e.g., pigtail) to prevent vessel injury. Finally, to minimise the risk of thrombus formation, catheters and sheaths should be checked for adequate back flow and flushed regularly with heparinised saline and, in case of prolonged diagnostic angiography, periprocedural anticoagulation with a low dose of heparin should be considered. Prolonged catheter manipulation in patients with advanced atherosclerotic disease may trigger cholesterol embolisation syndrome, a condition which cannot be prevented by anticoagulation [11. Cholesterol embolization syndrome. Circulation. 2010;122:631-41.
View chapter , adverse events related to peripheral diagnostic angiography are rare and mostly concern inappropriate manipulation of wires or catheters, and power injections performed with automatic injectors (Focus box 2). Catheters should always be advanced over a wire. Before performing contrast injection, the catheter tip should be fluoroscopically screened to ensure that is free, in order to prevent injection-related vessel wall dissections or embolisation of plaque material. An invasive pressure measurement at the catheter tip is helpful to exclude contact between the tip and the vessel wall. If diagnostic catheters are advanced over hydrophilic 0.035” wires, the latter should be handled with caution because they may lead to inadvertent vessel wall dissection or perforation through the loss of tactile feedback. High-flow injections delivered by power injectors should be performed using catheters with multiple-side-hole (e.g., pigtail) to prevent vessel injury. Finally, to minimise the risk of thrombus formation, catheters and sheaths should be checked for adequate back flow and flushed regularly with heparinised saline and, in case of prolonged diagnostic angiography, periprocedural anticoagulation with a low dose of heparin should be considered. Prolonged catheter manipulation in patients with advanced atherosclerotic disease may trigger cholesterol embolisation syndrome, a condition which cannot be prevented by anticoagulation [11. Cholesterol embolization syndrome. Circulation. 2010;122:631-41.
Excellent review on the topic.]. Although virtually any organ or tissue can be affected by cholesterol embolisation syndrome, most commonly involved are the brain, the kidneys, the gastrointestinal tract, and the skin and skeletal muscles of the lower extremities. End-organ damage is the result of small vessel occlusion due to embolisation and foreign-body inflammatory response to cholesterol emboli.
Basic principles to reduce the risk of non-access-related complications of diagnostic angiography:
- Perform high-flow injections through multiple-side-hole catheters
- Do not advance a catheter without a wire
- Make sure that the catheter tip is not in contact with the vessel wall before injecting
- Check sheaths and catheters for back-flow and flush them regularly
- For prolonged catheterisation consider periprocedural anticoagulation
- Caution while advancing hydrophilic wires
- Minimise catheter manipulations.
Lower extremity angiography
INTRODUCTION
The indications for pelvic and lower extremity angiography include ischaemia (either resting or exertional) owing to atherosclerosis, embolism, thrombosis and vasculitis [22. Endorsed by: the European Stroke Organisation (ESO); Authors/Task Force Members, Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clément D, Collet JP, Cremonesi A, De Carlo M, Erbel R, Fowkes FG, Heras M, Kownator S, Minar E, Ostergren J, Poldermans D, Riambau V, Roffi M, Röther J, Sievert H, van Sambeek M, Zeller T; ESC Committee for Practice Guidelines (CPG), Bax J, Auricchio A, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Knuuti J, Kolh P, McDonagh T, Moulin C, Poldermans D, Popescu B, Reiner Z, Sechtem U, Sirnes PA, Torbicki A, Vahanian A, Windecker S; Document Reviewers, Kolh P, Torbicki A, Agewall S, Blinc A, Bulvas M, Cosentino F, De Backer T, Gottsäter A, Gulba D, Guzik TJ, Jönsson B, Késmárky G, Kitsiou A, Kuczmik W, Larsen ML, Madaric J, Mas JL, McMurray JJ, Micari A, Mosseri M, Müller C, Naylor R, Norrving B, Oto O, Pasierski T, Plouin PF, Ribichini F, Ricco JB, Ruilope L, Schmid JP, Schwehr U, Sol BG, Sprynger M, Tiefenbacher C, Tsioufis C, Van Damme H. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries * The Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2851-906.
First guidelines from the European Society of Cardiology on atherosclerotic peripheral disease including carotid and vertebral disease., 33. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM Jr, White CJ, White J, White RA, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B; American Association for Vascular Surgery; Society for Vascular Surgery; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society of Interventional Radiology; ACC/AHA Task Force on Practice Guidelines Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease; American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; Vascular Disease Foundation. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113:e463-654.
Latest guidelines from the American College of Cardiology/American Heart Association on peripheral artery disease., 44. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG; TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45:S5-67.
Latest edition of the TASC guidelines.]. Other potential indications include detection of active bleeding, peripheral aneurysms, vascular tumours, trauma and extrinsic compression. Prior to angiography, the ankle-brachial index (ABI) should be assessed in patients presenting with claudication, critical or acute limb ischaemia ( for details,  View chapter ). From an interventional perspective, the main advantage of the routine ABI measurements at baseline is the possibility of assessing the immediate haemodynamic impact of revascularisation as well as of detecting early (e.g., vessel occlusion, distal embolisation) and late (e.g., restenosis) complications.
View chapter ). From an interventional perspective, the main advantage of the routine ABI measurements at baseline is the possibility of assessing the immediate haemodynamic impact of revascularisation as well as of detecting early (e.g., vessel occlusion, distal embolisation) and late (e.g., restenosis) complications.
From an anatomical standpoint, the lower extremity vasculature can be classified into three functional segments:
- The inflow vessels – the common iliac (CIA) and the external iliac (EIA) arteries. The internal iliac artery (IIA) is not considered as an inflow vessel, even if it may be responsible for buttock claudication or impotence and may play an important role for collateral supply when the EIA is occluded.
- The outflow vessels – the common femoral (CFA), profunda femoral artery (PFA), superficial femoral (SFA) and the popliteal arteries; and
- The runoff vessels – the tibioperoneal trunk, the anterior tibial, the posterior tibial and the peroneal arteries.
Based on the territory affected, the condition is classified as inflow, outflow, distal or multilevel disease.
VASCULAR ACCESS
A critical step of any endovascular procedure involving the lower extremity is the choice of the most appropriate access site. Accordingly, adequate access reduces the rate of complications, shortens the duration of the procedure, reduces the amount of contrast used, and limits the radiation exposure of patients and operators. While the general principles of vascular access at the different sites, as well as the related complications, are detailed in  View chapter, we focus here on some technical aspects related to lower extremity angiography and interventions ( Table 2 ). As a general rule, the location of the lesion(s) to be treated determines the access site. In addition, the diameter of the access vessel has to be adequate for the size of catheter and sheaths required for the intervention. Finally, the presence of an underlying bony structure facilitates haemostasis through manual compression. This point is of particular importance if vascular closure devices cannot be used. A small number of pre-requisites are critical for an optimal access site choice:
View chapter, we focus here on some technical aspects related to lower extremity angiography and interventions ( Table 2 ). As a general rule, the location of the lesion(s) to be treated determines the access site. In addition, the diameter of the access vessel has to be adequate for the size of catheter and sheaths required for the intervention. Finally, the presence of an underlying bony structure facilitates haemostasis through manual compression. This point is of particular importance if vascular closure devices cannot be used. A small number of pre-requisites are critical for an optimal access site choice:
a) The review of previous angiographic and noninvasive exams.
b) The exact knowledge of timing and nature of previous lower extremity revasculariation procedures (endovascular or surgical). Puncture of grafts – especially if close to the anastomosis site – should be avoided in the first 6-12 months following surgery. However, if necessary, the native vessel or the prosthetic graft may be accessed under fluoroscopic or ultrasound guidance in order to reduce the risk of puncturing the anastomotic site.
Retrograde CFA access
This is the most frequently performed for diagnostic and interventional procedures of the lower extremities. Puncture of the CFA should be performed proximal to its bifurcation, which in more than 75% of cases is located at the level of the lower part of the femoral head or inferiorly ( Figure 1 ) [55. Schnyder G, Sawhney N, Whisenant B, Tsimikas S, Turi ZG. Common femoral artery anatomy is influenced by demographics and comorbidity: implications for cardiac and peripheral invasive studies. Catheter Cardiovasc Interv. 2001;53:289-95.
Prospective study on the common femoral anatomy and bony landmarks to identify the ideal puncture site.]. To that end, the puncture site should be defined with fluoroscopy based on bony landmarks. Of note, a puncture of the CFA proximal to the inguinal ligament may lead to a retroperitoneal bleed because of the inability to perform efficacious manual compression in case of vascular closure device failure. In the case of high CFA puncture, contrast angiography performed through the sheath can help to define whether the puncture occurred above or below the inguinal ligament. Accordingly, the deep circumflex iliac artery takes off at the distal border of the inguinal ligament. In case of puncture above the inguinal ligament, vascular closure devices devices have a higher failure rate. A puncture above the inguinal ligament includes the risk of a retroperitoneal bleeding and the patient should be checked very carefully. Through a cross-over manoeuvre, retrograde CFA access allows for the treatment of the ipsilateral iliac arteries as well as the contralateral limb.
Antegrade CFA access
This offers an extremely stable platform to treat SFA, popliteal as well as below-the-knee (BTK) disease. As for the retrograde approach, the target site of entry is the CFA below the inguinal ligament. Gaining access using an antegrade technique may be more challenging and associated with higher complication rates than the retrograde CFA approach, especially in obese patients or in the presence of high CFA bifurcation. If the anatomy is not known, it is recommended that an ultrasound to assess the level of the CFA bifurcation should be carried out. In the case of high bifurcation, the operator may be more inclined to use a retrograde approach with cross-over instead of an antegrade one. Alternatively, puncture under ultrasound guidance may be a valid option. In obese patients with high CFA bifurcation, the proximal segment of the SFA may be accessed under ultrasound guidance, as long as it is free from disease. However, haemostasis may be more challenging. Finally, antegrade access limits the angiography and intervention targets to the ipsilateral leg at the femoropopliteal as well as BTK levels. The minimum learning curve for experienced interventionists prior to applying the antegrade femoral approach correctly and safely across different patient and anatomical subsets has been estimated to be 60 cases [66. Biondi-Zoccai GG, Agostoni P, Sangiorgi G, Dalla Paola L, Armano F, Nicolini S, Alek J, Fusaro M. Mastering the antegrade femoral artery access in patients with symptomatic lower limb ischemia: learning curve, complications, and technical tips and tricks. Catheter Cardiovasc Interv. 2006;68:835-42.
Series addressing the learning curve issue for the antegrade common femoral approach suggesting that a minimum of 60 procedures is needed to master the technique.].
Retrograde CFA access and cross-over manoeuvre vs. antegrade CFA access ( Table 2 )
An in-depth analysis of patient characteristics and lesions subsets should be performed before choosing between a retrograde and an antegrade access. In the presence of very tortuous and/or calcified iliac axes as well as a narrow angled aortic bifurcation (i.e., steep bifurcation), the antegrade approach should be favoured because the cross-over manoeuvre may be challenging and be more prone to complications such as vascular dissection ( Figure 2 ). Similarly, if the target lesion is at the femoropopliteal level and is severely calcified, the antegrade approach may be advantageous because of the greater back-up delivered. Conversely, in obese patients, because of the increased risk of antegrade access complications, the retrograde approach should be favoured [66. Biondi-Zoccai GG, Agostoni P, Sangiorgi G, Dalla Paola L, Armano F, Nicolini S, Alek J, Fusaro M. Mastering the antegrade femoral artery access in patients with symptomatic lower limb ischemia: learning curve, complications, and technical tips and tricks. Catheter Cardiovasc Interv. 2006;68:835-42.
Series addressing the learning curve issue for the antegrade common femoral approach suggesting that a minimum of 60 procedures is needed to master the technique.]. While the retrograde approach remains the most popular for the treatment of most femoral lesions, for some centres the antegrade puncture is the default strategy for the same condition.
Brachial access
Vascular access using a brachial approach may be considered in bilateral CIA or distal aortic occlusions and in the presence of a CIA occlusion either when associated with an acutely angulated CIA bifurcation or in the absence of a sufficient CIA stump, that does not allow for adequate support with a cross-over approach. In case of ostial CIA occlusion, the brachial approach offers advantages over the retrograde CFA approach. In fact, a retrograde approach carries the risk of subintimal tracking extending into the distal abdominal aorta. The insertion of sheaths >6 Fr carries an increased risk of arm ischaemia, especially in women or in short men. However, thanks to the low profile of new endovascular equipment, a 6 Fr introducer sheath allows for most endovascular procedures. In addition, the current shaft length of most balloon catheters and stents allows for revascularisation down to the proximal segment of the femoral arteries in most patients.
Accessing the brachial artery at the level of the elbow crease, if necessary under ultrasound guidance, allows for adequate haemostasis using manual compression and reduces the access-site complications. Nevertheless, the complication rate for brachial access remains higher compared with the retrograde CFA one [77. Hildick-Smith DJ, Khan ZI, Shapiro LM, Petch MC. Occasional-operator percutaneous brachial coronary angiography: first, do no arm. Catheter Cardiovasc Interv. 2002;57:161-5.
Prospective series showing high complication rates of the brachial approach.]. Complications of the brachial approach include acute arterial occlusion – with subsequent forearm ischaemia requiring emergency surgical or endovascular revascularisation – bleeding, compartment syndrome, nerve damage with transitory or permanent sensory disturbances, and pseudo-aneurysm (  View chapter ). The following may lead to bleeding complications: a) challenging haemostasis with manual compression (e.g., in obese patients); b) the fact that vascular closure devices are not approved and rarely used in this location; and/or c) the fact that the sheath is usually retrieved immediately at the end of the procedure while the patient is still fully anticoagulated, in order to prevent vessel occlusion. On account of the possibility of major complications, in cases of access site bleeding and insufficient control with manual compressions, operators should have a low threshold for reversing heparin.
View chapter ). The following may lead to bleeding complications: a) challenging haemostasis with manual compression (e.g., in obese patients); b) the fact that vascular closure devices are not approved and rarely used in this location; and/or c) the fact that the sheath is usually retrieved immediately at the end of the procedure while the patient is still fully anticoagulated, in order to prevent vessel occlusion. On account of the possibility of major complications, in cases of access site bleeding and insufficient control with manual compressions, operators should have a low threshold for reversing heparin.
Radial access
The radial approach has become very popular among interventional cardiologists because most of the coronary procedures can be performed using that route and 6 Fr access, and the incidence of vascular complications is lower than that using the CFA approach (  View chapter ). Before accessing the radial artery, a dual hand blood supply (i.e., by the radial and ulnar arteries) should be confirmed using the Allen test. Insufficient collateral arterial supply as assessed by this test is considered a contraindication to the technique. Under such circumstances a radial artery occlusion, which occurs in up to 5% of the procedures, theoretically may result in dramatic hand ischaemia although observational data in support of this is lacking.
View chapter ). Before accessing the radial artery, a dual hand blood supply (i.e., by the radial and ulnar arteries) should be confirmed using the Allen test. Insufficient collateral arterial supply as assessed by this test is considered a contraindication to the technique. Under such circumstances a radial artery occlusion, which occurs in up to 5% of the procedures, theoretically may result in dramatic hand ischaemia although observational data in support of this is lacking.
Radial access can be used for lower extremity angiography (e.g., in the setting of coronary angiography) using 125 cm long catheters such as the multipurpose or the Judkins right but it is rarely adopted for interventions below the inguinal ligament because those regions may not be reached with standard equipment, due to the insufficient working lengths available. In tall individuals (i.e., > 1,80 m [>5.9 feet]), the usual length of shaft of sheaths (90 cm), catheters (100 cm), and balloons/stents (135 cm) may not be adequate even to treat iliac lesions safely (i.e., may not allow for the treatment of downstream dissections). The insertion of long sheaths ≥6 Fr may be problematic, especially in women.
Left vs. right arm approach
Compared to the right approach, the left arm access is preferred for the following reasons ( Figure 3 ):
a) It reduces the distance between the access site and the target lesion, thereby augmenting the working length of the equipment.
b) It offers greater manoeuvrability of the equipment, especially in the presence of a tortuous/angulated aortic arch.
c) It minimises the risk of brain embolisation because instrumentation and passage of equipment only occurs across the origin of the left vertebral artery, whereas, with the right brachial approach, embolisation to all supra-aortic vessels may occur.
ANGIOGRAPHIC TECHNIQUES
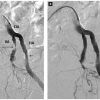
The most frequently used sheath size for diagnostic angiography of the lower extremities is 5 Fr. A 4 Fr strategy may be suitable for antegrade femoral access, in the case of purely diagnostic exams or of an increased risk of bleeding if, based on noninvasive imaging, the revascularisation procedure could also be performed with 4 Fr compatible equipment (e.g., for simple femoro-popliteal or BTK lesions). In the absence of renal insufficiency, it is useful to start all angiographic studies of the lower extremities with a pelvic aortogram in DSA. To that end, a pigtail catheter is placed at the level of L3, slightly above the aortoiliac bifurcation (typically the aorta bifurcates at L4-L5 level) (Focus box 3). The field of image should include L3 cranially and both femoral heads caudally. The table should be positioned so that the catheter tip is visualised at the top of the screen, and elevated to its highest setting in order to maximise the size of the field of view and minimise the radiation dose. This allows for optimal visualisation of the distal aorta, CIA, IIA and EIA ( Figure 4 ). If clinically indicated, the pigtail catheter may be placed more cranially – at the level of the intervertebral space L1-L2 – and a lower magnification may be used in order to visualise the renal arteries as well (usually the kidney arteries arise from the aorta at L1-L2 level). The acquisition run of the abdominal aorta is obtained at 2-3 frames/sec, preferably during a patient breath-hold, using a contrast injection rate of 10-15ml/sec for a total of 20-30 ml at a maximum of 800 to 1000 psi ( Table 1 ). In addition to excluding a relevant pathology at this level, the pelvic aortogram allows for an assessment of the feasibility/risk associated with a cross-over approach, should this be considered. If a stenosis at the level of the CIA or EIA is suspected, then an angulated view (contralateral anterior oblique 30 – 45°) should be performed to allow the visualisation of the CIA bifurcation without overlap ( Figure 2 ).
Key points for lower extremity angiography
- Pelvic angiography is necessary for the assessment of cross-over options
- Distal run-off angiography should always be performed prior to endovascular interventions in order to:
- have a complete diagnostic study;
- plan the intervention;
- estimate the probability of success;
- identify complications during revascularisation such as distal embolisation.
- Multiple projections may be needed to make an adequate assessment of:
- the internal-external iliac bifurcation;
- the common femoral bifurcation;
- the distal popliteal trifurcation.
- In patients with critical limb ischaemia, the angiographic study should include the foot circulation.
Subsequently, runoff DSA angiography of the lower extremity is performed with a catheter placed in the distal segment of the EIA and by taking sequential static images of the extremity. Usually, an image rate of 1-frame/second for above-the-knee and 0.5 to 1-frame/second for BTK acquisitions is sufficient in order to visualise the vascular bed adequately. Commonly, 10 ml of contrast at a 4-6 ml/sec rate is injected. If DSA is not available, angiography can be performed at 10-15 frames/sec and 7.5-10 frames/sec for aortoiliac and femoropopliteal territories respectively.
Alternatively, a lower extremity runoff angiogram can be performed by injecting a bolus of contrast agent followed in real time by a manual or automatic (i.e., bolus chase technology) movement of the table from the pelvis to the foot. To that end, the catheter delivering the contrast should have an adequate lumen (≥ 5 Fr) and multiple side holes (e.g., pigtail catheter). If angiography is performed with a moving table and bolus chase technology, contrast material must be injected, possibly with the help of an automatic injector, at a rate of 6-8 ml/sec for a total of 2-3 seconds (i.e., 15-20 ml). Filming is begun immediately after the injection and the bolus of contrast is then chased – either manually or automatically – from the proximal CFA to the feet. If the bolus chase is combined with DSA, a run without contrast is performed prior to bolus injection. Although the image quality is usually sufficient with these dynamic acquisitions, the total radiation dose is higher – especially with DSA acquisition – because of the constant dose adaptation required according to the segments studied and the major dose differences required for pelvis, thigh or calf acquisition. The advantage of the bolus chase technology is that it allows full lower limb visualisation in one shot with a limited amount of contrast medium.
Optimal opacification of the runoff vessels –preferably with DSA – prior to any lower limb intervention is critical: first, because the quality of the runoff predicts the short- and long-term success of revascularisation; secondly, a baseline study allows for early detection of complications such as distal embolisation and wire dissections or perforations (Focus box 3).
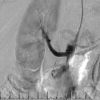
To assess the take-off of the BTK vessels adequately, a 45°-60° ipsilateral view is frequently helpful. In particular, the ostium of the anterior tibial artery is often hidden by the tibio-peroneal trunk in the AP projection. Further down, the AP projection is usually adequate to assess the vessels to the foot. However, especially in the angulated view, the peroneal and the anterior tibial arteries do cross at mid-calf level and this may lead to misinterpretations ( Figure 5 ). Finally, the best projection to visualise the entire foot circulation is the lateral view, which may easily be obtained simply by asking the patient to turn the foot slightly to one side and by setting the x-ray camera at 90°. An angiography of the pedal and plantar arteries is of paramount importance in patients with critical limb ischaemia. If a stenosis is suspected on the standard view, an additional angulated view should be performed. Multiple views may be indicated to make an adequate assessment of the CFA bifurcation as well as the distal popliteal trifurcation.
For the selective lower extremity runoff ipsilateral to the access site, contrast is injected directly through the arterial sheath placed in the EIA. If the contralateral leg needs to be injected, then a cross-over manoeuvre is required. To accomplish this, catheters such as the internal mammary or the Cobra are advanced over a soft-tipped steerable 0.035” guidewire. Wires frequently used include the non-hydrophilic ones, Wholey™ (Mallinckrodt, Inc., Hazelwood, MO, USA) and Magic Torque™ (Boston Scientific, Natick, MA, USA), and hydrophilic-angled Glidewire® and stiff-angled Glidewire® (Terumo Corp., Tokyo, Japan). When the angle between both CIA is acute, a shepherd’s crook-shaped catheter such as the Simmons-1 or -2 (Cook Medical Inc., Bloomington, IN, USA) or the SOS-OMNI® (AngioDynamics, Latham, NY, USA) may be used to cannulate the contralateral CIA. These catheters have to be pre-shaped in the aorta before attempting the selective engagements in the contralateral iliac artery. Alternatively, the contralateral CIA can also be engaged by unfolding a pigtail catheter using an angled 0.035” wire. Once the tip of the catheter is at the ostium of the contralateral CIA, the wire is then advanced gently down the CFA and the catheter is placed in the distal CIA. Hand or power injection at 6-8 ml/sec for a total of 15 ml is sufficient for adequate visualisation of the iliac arteries. Using the brachial approach, the iliac vessels may be visualised by selectively engaging the common iliac artery with a 125 cm multipurpose catheter.
COMPLICATIONS
As in any other territory, complications secondary to diagnostic angiography of the lower limbs are rare and are mostly related to access or inappropriate manipulation of wires or catheters as well as to power injections performed with an automatic injector (Focus box 2). As a general rule, the bleeding risk associated with the femoral approach increases with punctures above the inguinal ligament, while punctures at the level of, or distally to, the femoral bifurcation cause more haematomas and carry an increased risk of pseudoaneurysms and the formation of arteriovenous fistulae. Aortography should be performed carefully in patients with abdominal aortic aneurysm because distal embolisation of wall-apposed thrombus may occur during power injections.
Renal and mesenteric angiography
INTRODUCTION
Based on the adequate accuracy of duplex US, CTA and MRA, catheter angiography is rarely required for diagnostic purposes. However, in the presence of a high degree of clinical suspicion and inconclusive noninvasive imaging, catheter angiography remains the gold standard to document significant stenosis of the visceral arteries (i.e., renal arteries, celiac trunk, superior and inferior mesenteric arteries).
VASCULAR ACCESS
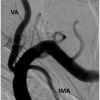
The retrograde femoral access is the most frequently adopted for angiography of the visceral arteries. Selective engagement of the vessels is obtained with dedicated pre-shaped catheters. For the endovascular treatment of the superior and inferior mesenteric arteries as well as for renal arteries with extreme inferiorly directed take-offs (>120° angle between the abdominal aorta and the proximal portion of the vessel), the left brachial approach is frequently preferred because it enables a more stable sheath or catheter position ( Figure 6 ). The left (preferably) or right radial approaches can also be used for diagnostic angiography, but 125 cm long catheters may be required. However, in most patients a revascularisation procedure may not be possible due to the insufficient length of guiding catheters, sheaths, balloon catheters or stents via the radial access.
ANGIOGRAPHIC TECHNIQUES
It is recommended to perform an abdominal aortic angiogram in the AP view prior to selective engagement of the renal or mesenteric vessels (Focus box 4). The catheter – commonly a pigtail 5 Fr – should be placed at the level of the L1-L2 intervertebral space. Satisfactory DSA images can be obtained using a total volume of 20-40 ml of contrast at a rate of 15-20 ml/sec. Patients should be instructed to hold their breath and not to move during image acquisition. As long as the opacification is adequate, aortography is sufficient to exclude significant renal artery disease. Selective renal artery angiography may be indicated only if the aortogram is of insufficient quality or if a renal artery stenosis is suspected. Conversely, aortography is often insufficient to assess adequately the degree of stenosis of mesenteric vessels. Since these vessels arise anteriorly, an additional lateral projection aortography is very helpful to visualise the take-off of the mesenteric arteries and to quantify the degree of the stenosis, which frequently has an ostial location ( Figure 7 ). Prior to revascularisation of mesenteric arteries, an angiogram should be obtained with a guiding catheter just in front of the ostium and a 0.014’’ guidewire advanced into the vessel. This allows for an adequate assessment and at the same time reduces the risk of guiding-induced vascular dissections.
Angiography of the mesenteric and renal arteries
- Femoral approach is the most common
- If downward take-off of the vessels and intervention is planned, consider arm approach
- Left brachial approach is adequate for both diagnostic angiography and interventions
- Radial approach may be used for angiography - 125 cm catheters may be needed - but is not adequate in all patients for revascularisation
- Aortography prior to selective cannulation is recommended
Mesenteric angiography
A 5 Fr system is usually adequate for selective mesenteric angiography. Femoral access is commonly used and DSA is favoured, as long as the patient can hold his breath sufficiently. Alternatively, a left brachial or radial approach may facilitate the selective engagement of the mesenteric vessels, which typically have an inferiorly directed take-off (Focus box 4). The arm approach may be particularly helpful if a percutaneous intervention is likely because of the better back-up conveyed. From a femoral approach, Judkins Right 4, internal mammary or Cobra catheters can be used to engage visceral vessels selectively. Alternatively, reverse angulation catheters such as an SOS-OMNI® or a Simmons 1 catheter are frequently used. Reverse angulation catheters are particularly helpful in patients with dilated abdominal aorta and should firstly be placed and manipulated in the thoracic aorta in order to regain their original curve. Thereafter, the mesenteric vessels may be engaged by gently retrieving the catheter while keeping it in an anterior orientation. Having a wire protruding 1-2 cm from the catheter tip may prevent the catheter from catching onto sidewall atheroma with subsequent plaque embolisation during the retrieval manoeuvre.
From a brachial or radial approach, the mesenteric arteries can usually be engaged easily using a multipurpose diagnostic catheter. If a radial approach is used, a 125 cm length catheter may be required. Arm access is particularly helpful in patients with severe aorto-iliac disease or tortuosity, abdominal aortic aneurysm, and inferiorly directed vessel origins. A sharp angle between the abdominal aorta and the origin of the mesenteric vessels is of particular concern if a femoral approach is chosen because, despite the fact that it is almost always possible to engage and wire the mesenteric arteries, it may be challenging to advance a bulky/rigid balloon-expandable stent (usually 6-8 mm in diameter) if the vessel take-off has an angle >90°.
Selective angiography of the coeliac trunk is performed with a 15°-30° left anterior oblique (LAO) angulation to demonstrate the coeliac axis origin and trifurcation into the left gastric, common hepatic and splenic arteries. In cases of suspected coeliac artery compression syndrome, comparative selective views should be obtained at end-inspiration and end-expiration as expiration itself may exacerbate vessel compression. Given its course to the rightward pelvis, angiography of the superior mesenteric artery should be performed in a 15°-30° LAO projection. By comparison, the inferior mesenteric artery has a leftward course. Selective angiography of this vessel should therefore be performed in a 15°-30° right anterior oblique (RAO) projection.
Renal angiography
The renal arteries originate from the lateral abdominal aorta immediately below the superior mesenteric artery at the level of the lower border of the L1 vertebral body. The right and left renal arteries originate at the same level in approximately half of patients while in the rest the right renal artery arises slightly higher than the left. Typically, the right renal artery has a more anterolateral origin from the aorta and courses downward while the left renal artery is located in a more posterolateral position and has a horizontal course [88. Verschuyl EJ, Kaatee R, Beek FJ, Patel NH, Fontaine AB, Daly CP, Coldwell DM, Bush WH, Mali WP. Renal artery origins: best angiographic projection angles. Radiology. 1997;205:115-20.
CT study of 200 patients addressing the best views for the renal arteries.].
The femoral approach is the most common access used for renal angiography, and adequate images can easily be obtained with a 5 Fr system. Left brachial access is reserved for patients with severe aortoiliac disease, known as abdominal aortic aneurysm, or for whom a renal revascularisation procedure is planned and whose target renal artery has a marked downward course (Focus box 4 and Figure 6 ). For diagnostic purposes a left or right radial access (e.g., simultaneously with coronary angiography) and 125 cm Judkins right or multipurpose catheter may be used. However, in most patients a revascularisation procedure may not be possible due to the insufficient length of guiding catheters or sheaths via the radial access. Via the femoral access, the Judkins Right 4 catheter is frequently used by cardiologists as a workhorse catheter for selective renal angiography as well as for renal interventions. Alternatively, an internal mammary or renal double curve catheter can be used. In cases of aortoiliac tortuosity, a Cobra C2, a Simmons 1-2, or a SOS-OMNI catheter may be necessary to reach the ostia. Aortic calcifications and prior-placed renal artery stents serve as important landmarks to indicate the renal ostia.
Importantly, the right renal artery originates about 20°-30° anteriorly, and the left originates only slightly posteriorly. Therefore, AP projection angiography may not adequately illustrate the renal ostia. Accordingly, one study demonstrated that in AP projection the optimal visualisation of the right renal ostium was obtained in only 26% of cases and of the left renal ostium in 38% of cases [88. Verschuyl EJ, Kaatee R, Beek FJ, Patel NH, Fontaine AB, Daly CP, Coldwell DM, Bush WH, Mali WP. Renal artery origins: best angiographic projection angles. Radiology. 1997;205:115-20.
CT study of 200 patients addressing the best views for the renal arteries., 99. Beregi JP, Mauroy B, Willoteaux S, Mounier-Vehier C, Rémy-Jardin M, Francke J. Anatomic variation in the origin of the main renal arteries: spiral CTA evaluation. Eur Radiol. 1999;9:1330-4.
CT study of 100 patients to assess the origin of the renal arteries.].
In the majority of cases, selective right and left renal ostia may be adequately shown on a 10°-20° LAO angulation. Occasionally, slight additional (~10°) cranial or caudal angulation may be necessary to improve visualisation. Care should be taken to visualise any accessory renal arteries since these are commonly present. The presence of an accessory renal artery should be suspected when the kidney is not entirely opacified by the selective main artery contrast injection. Only if a sizeable part of the kidney is not vascularised by the main artery is selective injection of the accessory artery necessary. Prior to injection, the catheter must be carefully aspirated to retrieve all the plaque material possibly located at the tip of the catheter and the absence of contact between the catheter and the vessel wall should be assessed via pressure waveform or a gentle contrast injection by hand. The field of view should be large enough to incorporate the kidney, and the angiography run should also be long enough to visualise the influx of contrast into the renal cortex. Care should also be taken not to introduce the catheter too deeply into the renal ostium as this may lead to underestimation of the lesion severity due to insufficient opacification of the ostium. Damping of the pressure waveform upon selective engagement may indicate significant ostial stenosis.
The visualisation of the renal arteries using a brachial or radial approach may at times be challenging, e.g., in cases of subclavian or innominate stenosis or tortuosity, or steep aortic arch. In this setting, the use of a stiff 0.035” Glidewire® (Terumo) or the advancement of a 125 cm long catheter over a 90 cm long sheath placed above the level of the mesenteric vessels may be helpful.
COMPLICATIONS
Worsening of the renal function following mesenteric or renal angiography may be the result of underlying parenchymal disease, renal artery stenosis, micro-embolisation, or contrast-induced nephropathy. Particular care should be taken in the angiographic study of patients with pre-existing renal dysfunction and suspected renal artery stenosis, as described in  View chapter. Since kidneys are end-organs with unique vascularisation, any distal embolisation occurring during angiography will result in tissue loss. Even if most of the time these infarctions are very small, it has been postulated that they may be responsible for the kidney function deterioration sometimes observed after renal stenting. Other visceral organs, such as the liver and the bowel, have a double vascularisation and multiple connections between the two systems. Therefore, distal embolisation following angiography or intervention is rarely an issue. However, organ dysfunction of the visceral organs may be observed in the case of cholesterol embolisation syndrome [11. Cholesterol embolization syndrome. Circulation. 2010;122:631-41.
View chapter. Since kidneys are end-organs with unique vascularisation, any distal embolisation occurring during angiography will result in tissue loss. Even if most of the time these infarctions are very small, it has been postulated that they may be responsible for the kidney function deterioration sometimes observed after renal stenting. Other visceral organs, such as the liver and the bowel, have a double vascularisation and multiple connections between the two systems. Therefore, distal embolisation following angiography or intervention is rarely an issue. However, organ dysfunction of the visceral organs may be observed in the case of cholesterol embolisation syndrome [11. Cholesterol embolization syndrome. Circulation. 2010;122:631-41.
Excellent review on the topic.].
Carotid and vertebral angiography
INTRODUCTION
Selecting an appropriate imaging modality is an essential component of the management of patients with carotid or vertebral disease. Duplex US remains the cornerstone of diagnostics of cervical vascular disease while other frequently applied techniques include CTA and MRA [1010. Qureshi AI, Alexandrov AV, Tegeler CH, Hobson RW 2nd, Dennis Baker J, Hopkins LN; American Society of Neuroimaging; Society of Vascular and Interventional Neurology. Guidelines for screening of extracranial carotid artery disease: a statement for healthcare professionals from the multidisciplinary practice guidelines committee of the American Society of Neuroimaging; cosponsored by the Society of Vascular and Interventional Neurology. J Neuroimaging. 2007;17:19-47.
American guidelines on the duplex screening of carotid disease.]. Although DSA remains the imaging gold standard of the carotid and vertebral arteries, based on the good level of accuracy of noninvasive imaging, catheter angiography is rarely needed for diagnostic purposes. However, invasive angiography remains an essential step in the planning and execution of endovascular procedures. In addition to DSA, the equipment used for angiography of the cervicocranial vessels should include the roadmap or overlay trace subtract functions.
VASCULAR ACCESS
Carotid and vertebral angiography are usually performed under local anaesthesia using a femoral approach and 4 Fr or 5 Fr diagnostic catheters. In selected cases, e.g., in the presence of advanced aortoiliac disease, the supra-aortic vessel may be engaged using a brachial or radial approach. However, these alternative access strategies may increase the risk of complications such as distal embolisation and vessel dissections due to more complex catheter manipulations in the aortic arch.
ANGIOGRAPHIC TECHNIQUES
Selective cannulation of supra-aortic vessels requires gentle manipulation and training. Intubation techniques with different catheters can be taught successfully on simulators [1111. Patel AD, Gallagher AG, Nicholson WJ, Cates CU. Learning curves and reliability measures for virtual reality simulation in the performance assessment of carotid angiography. J Am Coll Cardiol. 2006;47:1796-802.
Study documenting the learning curve for carotid angiography on virtual reality simulation.]. Sedation should be avoided in order to make an adequate assessment of the neurological status of the patients throughout the procedure. Despite the lack of data, the administration of unfractionated heparin - usually at a dose ranging from 2,000 to 5,000 units - is encouraged for carotid angiography and especially for a complete four-vessel cerebral angiography. The performance of an aortic arch angiogram at the beginning of cerebral angiography is recommended, especially in the presence of complex anatomy or if the arch was not studied noninvasively (Focus box 5). In this way, an accurate assessment of the aortic arch may detect disease at the level of the arch or at the origin of the supra-aortic vessels and may guide the choice of the appropriate strategy and choice of equipment. The suggested view is 30°-40° LAO. Good quality arch angiography is achieved using a 5 Fr pigtail catheter placed in the ascending thoracic aorta, and injecting 40 ml of contrast at a rate of 15 ml/sec with a pressure limit of 1,000 psi ( Figure 8 ). The classification of aortic arch anatomy is described in Figure 9 .
Carotid angiography
Intubation of the supra-aortic vessels is performed under fluoroscopic guidance in LAO or AP projections. While the left common carotid artery (CCA) is intubated directly, the innominate artery needs to be intubated first in order to engage the right CCA selectively. As a general rule, a diagnostic catheter should not be advanced in the supra-aortic vessels without prior advancement of a steerable 0.035” wire. The wire should not be advanced blindly but by using stored images such as a roadmap or overlay. The best view to open the bifurcation between the right CCA and the right subclavian artery (SCA) may be an AP or RAO view ( Figure 10 ), while the projection which allows optimal catheter control while advancing the diagnostic catheter into both the left and the right CCA is LAO. At the level of the carotid bifurcation, angiography may be performed in AP and in lateral views, as well as in ~30° RAO and ~30° LAO ( Figure 11 ). Multiple views may be necessary in order to separate the internal from the external carotid artery and to make an adequate assessment of the severity of the internal carotid artery stenosis. A view with adequate separation of the external and internal carotid arteries and which at the same time allows for good catheter control in the aortic arch is critical prior to starting an endovascular revascularisation of the carotid artery.
Intubation of the CCA may be achieved with a variety of diagnostic catheters. In the presence of a “friendly” aortic arch, it can be performed with catheter shapes such as the Judkins right coronary or the vertebral/Bernstein catheters. Alternatively, the headhunter catheter or the Bentson diagnostic catheter (Merit Medical Inc, Utah, USA) can be used as routine. For steeper/more tortuous aortic arches, reversed shaped catheters such as the Vitek (Cook Inc., Bloomington, IN, USA) or the Simmons “Sidewinder” may be needed. The handling of these catheters is more challenging and may be associated with an increased risk of embolisation. While the Vitek catheter can typically be shaped in the descending thoracic aorta, the Simmons “Sidewinder” catheters require manipulation in the aortic arch to shape the catheter for vessel engagement.
As already mentioned, in order to engage the right CCA selectively advancing the diagnostic catheter over a steerable 0.035” under roadmap or trace subtraction is recommended. In the presence of a “bovine arch” (i.e., left CCA originating from the brachiocephalic trunk) direct intubation of the left CCA may be achieved with a coronary Amplatz left catheter or a Simmons “Sidewinder” shape. Alternatively, intubation of the left CCA with this particular anatomy may be achieved using a right radial or brachial approach. In patients undergoing carotid artery stenting, it is recommended that a baseline intracranial angiogram in AP view (better if a lateral view is also added) is performed in order to detect additional lesions in the distal/intracranial ICA, and in order to have a comparative study should complications occur during the procedure.
Vertebral angiography
The evaluation of the origin and the proximal portion of the vertebral arteries (VA) might be difficult on aortic arch angiography because of frequent vessel overlap. As atherosclerosis of the VA typically affects the ostium and/or the proximal segment, it is mandatory to perform angiography in the absence of vessel superimposition in those segments. The left SCA is usually easily accessible to catheterisation with a variety of diagnostic catheters. Selective intubation of the right SCA may pose difficulties in tortuous/steep aortic arches or in cases where the innominate artery has an elongated, tortuous course. For most cases a vertebral, Judkins right or headhunter diagnostic catheter will easily allow cannulation of the innominate artery. In more demanding aortic arches this may be achieved with catheter shapes such as Bentson or Simmons “Sidewinder”. A roadmap is then performed, and the catheter is advanced over a steerable 0.035” wire in the SCA. Following intubation of the SCA, the first contrast injection should be performed in AP view. This should show adequately the ostium and proximal VA in the presence of a take-off at the superior aspect of the SCA. If there is insufficient visualisation, additional ~30° RAO and ~30° LAO projections may be used for assessment of both the right and the left VA. Sometimes multiple views are necessary to exclude an ostial stenosis. The more distal segments of the VA are usually well visualised on AP and lateral views. Since both VA unify intracranially and give origin to the basilar artery, the opacification of one VA - preferably the dominant one - is usually sufficient to demonstrate the whole vertebrobasilar circulation, and selective VA catheterisation may not be necessary ( Figure 12 ). The quality of a subselective VA angiogram may be improved by positioning the catheter in the SCA and by inflating the blood pressure cuff on the ipsilateral arm at suprasystolic levels during contrast injection.
If selective VA angiography is needed, then gentle manipulation of simple-shaped diagnostic catheters – like the vertebral, Judkins right or headhunter –is mandatory. If the catheter position at the VA ostium is not adequate, then it is is advanced a few centimetres into the VA over a steerable 0.035” guidewire. In difficult anatomical situations, the selective catheterisation of the VA should be discouraged because of the associated dissection or distal embolisation risk.
COMPLICATIONS
Specific complications of cerebral angiography include vessel dissection or distal embolisation. Both can result from catheter manipulations or forced contrast injection. In patients with symptomatic cerebral atherosclerosis undergoing diagnostic cerebral angiography, the reported risk of stroke ranged between 0.5% and 5.7%, and the risk of transient ischaemic attack was 0.6% to 6.8% [1212. Connors JJ 3rd, Sacks D, Furlan AJ, Selman WR, Russell EJ, Stieg PE, Hadley MN; NeuroVascular Coalition Writing Group; American Academy of Neurology; American Association of Neurological Surgeons; American Society of Interventional and Therapeutic Radiology; American Society of Neuroradiology; Congress of Neurological Surgeons; AANS/CNS Cerebrovascular Section; Society of Interventional Radiology. Training, competency, and credentialing standards for diagnostic cervicocerebral angiography, carotid stenting, and cerebrovascular intervention: a joint statement from the American Academy of Neurology, American Association of Neurological Surgeons, American Society of Interventional and Therapeutic Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, AANS/CNS Cerebrovascular Section, and Society of Interventional Radiology. Radiology. 2005;234:26-34.
Guidelines from the American neurology/neuroradiology societies.]. Recently, neurological complication rates <1% associated with angiography have been observed, suggesting that the risk may be lower than previously reported [1313. Fayed AM, White CJ, Ramee SR, Jenkins JS, Collins TJ. Carotid and cerebral angiography performed by cardiologists: cerebrovascular complications. Catheter Cardiovasc Interv. 2002;55:277-80.
Series documenting low complication rates in a high-volume centre.]. Possible explanations for these differences include improvements in equipment, technique (e.g., by flushing the catheters, cleaning the wires, and gentle catheter manipulation), operator experience, monitoring of catheter-tip pressure, and the use of procedural heparin and antiplatelet agents. While dissection may be treated either conservatively or with stenting, the management of distal embolisation depends on the location of the embolic process and the symptoms of the patient. Possible options include heparinisation, the administration of glycoprotein IIb/IIIa receptor inhibitors, systemic or in-situ thrombolysis, or mechanical recanalisation (  View chapter ).
View chapter ).
Upper extremity angiography
INTRODUCTION
Subclavian and brachiocephalic occlusive disease often has an intra-thoracic location. As a consequence, its assessment with duplex US may be challenging. Nevertheless, duplex scanning is helpful in suggesting the presence of haemodynamic significant stenosis of those vessels by detecting a pathological flow pattern in the distal SCA. In addition, the detection of flow reversal in the VA confirms the presence of critical stenosis or occlusion of the ipsilateral subclavian artery or brachiocephalic trunk. These vessels can be adequately studied with CTA and MRA. Therefore, DSA, although still considered the “gold standard” imaging modality for atherosclerotic disease, is rarely required for diagnostic purposes.
Invasive angiography of the arm or proximal forearm vessels for diagnostic purposes is rarely performed because, with modern US, CTA, or MRA equipment, these vessels are easily and adequately visualised. However, angiographies of the upper extremities are still frequently performed in the case of dysfunction of an arteriovenous shunt for dialysis, and selective DSA imaging is still the imaging modality of choice for disease of the distal forearm and the hand.
VASCULAR ACCESS
Diagnostic angiography of the upper extremities is typically performed using retrograde femoral access, because subclavian, brachial, radial and ulnar arteries may be visualised easily using standard catheters. If hand angiography is required, the quality of the images may be improved by advancing a 125 cm long catheter into the distal part of the brachial artery just cranially of the radio-ulnar bifurcation. Direct antegrade puncture of the brachial artery should be favoured if a revascularisation of the hand is planned. Angiography of arteriovenous fistulas for dialysis may be performed via an arterial access (i.e., femoral, radial or brachial) or via direct retrograde or antegrade puncture of the arterialised vein.
ANGIOGRAPHIC TECHNIQUES
An initial assessment of the anatomy of the aortic arch with an arch angiogram may be helpful if the patient has no contraindications such as renal insufficiency and was not investigated with CTA or MRA. This may be helpful in determining the appropriate diagnostic catheter for engagement of the right and left SCA, and for the detection of anomalies (e.g., anomalous origin of right SCA distal to left SCA [arteria lusoria], direct origin of the vertebral artery from the arch) which might influence vessel intubation.
In patients with normal anatomical origin of the great vessels and a benign configuration of the arch, the innominate artery and left SCA artery can be selectively engaged with either a Bernstein, a Judkins right, or a vertebral diagnostic catheter. With increasing complexity of the aortic arch, a Vitek catheter or Simmons catheter may be required. The bifurcation of the innominate artery (i.e., including the ostium and proximal portion of the right SCA) is best imaged in the RAO projection, whereas the LAO projection typically provides the best assessment of the origins of the right vertebral and right internal mammary arteries. While the left SCA is also nicely demonstrated in AP projection, the RAO projection generally allows the most accurate assessment of the origins of the left vertebral artery and left internal mammary artery ( Figure 13 ).
Subclavian angiography
When imaging the SCA specifically for the purpose of assessing the presence of arterial compression due to thoracic outlet syndrome, angiography should be performed in the AP projection with the arm in the neutral position (i.e., arm at side in adducted position) and the image repeated with the shoulder in full abduction, external rotation, and retroversion (as if pitching a baseball).
Imaging of the upper extremity vessels beyond the level of the SCA usually requires that a diagnostic catheter be advanced from the origins of the innominate and left SCA to the level of the axillary artery. In patients with friendly aortic arches this step is usually straightforward and is achieved by advancing the diagnostic catheter over a long (300 cm) soft-tipped 0.035” wire (e.g., Wholey™ [Mallinckrodt, Inc.], Magic Torque™ [Boston Scientific]) which is placed in the brachial artery using the road-mapping function for guidance. The presence of significant tortuosity in the subclavian artery may occasionally require the use of a hydrophilic wire such as the Glidewire® (Terumo Corp.). With complex arch anatomy which necessitates the use of a Vitek or Simmons catheter for engagement of the left SCA or innominate artery ostia, these catheters generally need to be exchanged for a gentle-shaped catheter (e.g., angled Glide, Judkins right, Bernstein) which can be delivered to the axillary artery after the 0.035” wire has been advanced into the brachial artery.
Axillary angiography
Axillary artery angiography is performed with the arm in the neutral position or slightly abducted. Angiography of the arm, forearm and hand is performed with the patient’s forearm and hand placed in the supine position on an arm board, and the digits splayed apart. Tape may be required to maintain the hand in this position and avoid motion artefact. Prior to imaging of the hand vessels, the administration of intra-arterial vasodilators is recommended (e.g., nitroglycerine 0.1-0.2 mg or verapamil 1-2.5 mg), and the surface of the hand should be kept warm to remove any risk of spasm. After achieving the appropriate positioning of the patient’s upper extremity, sequential overlapping static images of the upper extremity vessels are acquired in the AP projection, using angulated views when required. Again, the use of an automated power injector which allows the injection of 10 ml over a 2-second period (psi of 500-600) for a 25-40 cm (10-15 inches) field of view is optimal for imaging above the level of the hand. For optimal opacification of the hand, a selective angiography with the catheter placed at the level of the brachial artery (e.g., 3 ml/sec for a total of 6 ml) and higher magnification images are required.
COMPLICATIONS
Other than complications related to access, complications such as distal embolisation may occur in the presence of very tortuous and/or calcified aortic arch and subclavian arteries.
Personal perspective – Marco Roffi
Noninvasive imaging modalities such as duplex US, CTA and MRA have achieved a high degree of accuracy for the detection of atherosclerotic occlusive disease of the peripheral circulation. Therefore, catheter-based angiography is rarely required merely for diagnostic purposes. Nevertheless, invasive angiography remains the imaging gold standard for the peripheral vasculature and should be applied whenever there is a high degree of clinical suspicion of atherosclerotic disease if the results of noninvasive imaging are inconclusive or if they do not reflect the clinical presentation of the patient. Knowledge of appropriate catheter equipment, projections and injection rates are of paramount importance to perform a safe and high-quality vascular angiographic study. A critical step in the planning of an angiographic study is the choice of access site. This is mainly determined by the location of the lesion(s) and vascular anatomy. Complications of peripheral diagnostic angiography are rare and are mainly related to the access site, inappropriate manipulation of wires or catheters, and contrast agents.















CLEARLY
THANKS
excellent!