Summary
Following the SYNTAX trial, the multidisciplinary Heart Team has been emphasised as a tool for screening patients with coronary artery disease. The introduction of transcatheter-based therapies for the treatment of aortic stenosis and mitral regurgitation has expanded the indication for a Heart Team discussion. Recent and currently ongoing randomised trials now mandate a Heart Team discussion to identify patients eligible for randomisation. Risk models are frequently used during the Heart Team discussion to guide clinicians in the decision-making process. Popular models are the STS score, EuroSCORE, and SYNTAX (II) score. Although there is no data supporting the superiority of a Heart Team discussion over clinicians’ individual evaluation, current European and North American guidelines recommend that appropriate patients should be discussed by a Heart Team.
Introduction
Coronary artery disease (CAD) has historically been treated with coronary artery bypass graft (CABG) surgery. Since the introduction of percutaneous coronary intervention (PCI), first with balloon angioplasty and subsequently with stents, interventional cardiologists have increasingly treated patients with PCI [11. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72.
The first randomised trial comparing stenting with drug-eluting stents to coronary surgery, showing that surgery remains the preferred treatment for complex coronary artery disease., 22. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001-2008. JAMA. 2011;305:1769-76.
Study examining the national trends of coronary revascularisation in the United States, showing a decline in the annual rate of revascularisation, mainly due to a decrease in coronary surgery.].
Whether PCI or CABG should be the preferred revascularisation strategy depends on a number of factors including the lesional complexity of CAD, presence of ischaemia, left ventricular function, the involvement of prognostic coronary vessels, and comorbidities of the patient. Recent studies, however, have shown that the choice of treatment is also influenced by the geographical region and the treating clinician [33. Rothberg MB, Sivalingam SK, Ashraf J, Visintainer P, Joelson J, Kleppel R, Vallurupalli N, Schweiger MJ. Patients’ and cardiologists’ perceptions of the benefits of percutaneous coronary intervention for stable coronary disease. Ann Intern Med. 2010;153:307-13. , 44. Brownlee S, Wennberg J, Barry M, Fisher E, Goodman D, Bynum J. Improving patient decision-making in health care: a 2011 Dartmouth Atlas report highlighting Minnesota. In; 2011. ]. Cardio-thoracic surgeons and cardiologists may either intentionally or unintentionally omit certain details of PCI and CABG when counselling the patient, thereby creating a bias towards a specific treatment [55. Head SJ, Bogers AJ, Serruys PW, Takkenberg JJ, Kappetein AP. A crucial factor in shared decision making: the team approach. Lancet. 2011;377:1836. , 2727. Chandrasekharan DP, Taggart DP. Informed consent for interventions in stable coronary artery disease : problems, etiologies, and solutions. Eur J Cardiothorac Surg. 2011;39:912-7. ]. Patients need to be aware of risk-benefit ratios of different treatment strategies to take an evidence-based position and generate treatment preferences. A Heart Team consisting of (interventional) cardiologists and surgeons can best weigh up the advantages and disadvantages of revascularisation strategies, and thus advise which strategy is objectively preferrable for an individual patient. Active involvement of the patient in the Heart Team will furthermore allow shared decision-making which will ultimately increase patient satisfaction [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ].
In addition to coronary revascularisation, several catheter-based techniques to treat structural heart disease have been introduced over the last decades. The first transcatheter aortic valve implantation (TAVI) for symptomatic severe aortic stenosis (AS) was performed in 2002 [66. Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F, Derumeaux G, Anselme F, Laborde F, Leon MB. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106:3006-8. ], after which it has rapidly evolved into the new standard of care for patients deemed at very high risk for surgical aortic valve replacement (SAVR) with an estimated >15% risk of 30-day mortality [2929. Généreux P, Head SJ, Wood DA, Kodali SK, Williams MR, Paradis JM, Spaziano M, Kappetein AP, Webb JG, Cribier A, Leon MB. Transcatheter aortic valve implantation 10-year anniversary: review of current evidence and clinical implications. Eur Heart J. 2012;33:2388-98. , 3030. Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2012;33:2403-18. ]. For patients at high risk (>10%-15% risk of morality) TAVI was non-inferior to SAVR and thus both strategies are excellent. However, estimating risk and deciding who is a better candidate for TAVI than for SAVR is not straightforward. Patient referral patterns to either a cardiologist or cardio-thoracic surgeon might be region dependent [77. Bach DS, Siao D, Girard SE, Duvernoy C, McCallister BD Jr, Gualano SK. Evaluation of patients with severe symptomatic aortic stenosis who do not undergo aortic valve replacement: the potential role of subjectively overestimated operative risk. Circ Cardiovasc Qual Outcomes. 2009;2:533-9. ]. In addition, clinicians from different specialties do not always agree on what is the best treatment option and thus management of AS may result in an unmet need [88. Iung B, Cachier A, Baron G, Messika-Zeitoun D, Delahaye F, Tornos P, Gohlke-Bärwolf C, Boersma E, Ravaud P, Vahanian A. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26:2714-20.
First study to show that a large percentage of patients with aortic stenosis evaluated for surgery are not operated on.]. Current guidelines on valvular disease therefore provide a 1C recommendation to the Heart Team concept and stress that TAVI should only be performed if the Heart Team acknowledges that the patient is too high risk for surgery [3131. Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancelotti P, Pierard L, Price S, Schäfers HF, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppel UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2013;33:2451-96. ]. The Heart Team functions as a decision-making tool that includes all the necessary specialties to optimise treatment decisions for the individual patient.
This chapter describes the Heart Team and its development, inclusion of different specialties, tools for decision-making, and validation of the concept. Also discussed are its potential limitations.
The need for a Heart Team
Accumulating evidence suggest that decision-making in its current form may not be optimal; these is clear variability of care, and treatment recommendations are not always appropriate.
Data from the Euro Heart survey suggested that there were geographical differences among decisions to perform SAVR on patients with severe AS: 57% received SAVR in Eastern Europe while 73% in Western Europe [3232. Iung B, Cachier A, Baron G, Messika-Zeitoun D, Delahaye F, Tornos P, Gohlke-Bärwolf C, Boersma E, Ravaud P, Vahanian A. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26:2714-20. ]. In the European Association for Cardio-Thoracic Surgery (EACTS) database that included over one million patient records from 29 countries, the number of coronary procedures versus valvular procedures of the total case load was very diverse among countries, suggesting that decisions to perform surgery differ [3333. Head SJ, Howell NJ, Osnabrugge RL, Bridgewater B, Keogh BE, Kinsman R, Walton P, Gummert JF, Pagano D, Kappetein AP. The European Association for Cardio-Thoracic Surgery (EACTS) database: an introduction. Eur J Cardiothorac Surg. 2013;44:e175-80. ]. Strong evidence of variance in treatment for CAD comes from the Organization of Economic Cooperation and Development (OECD) that reported the number of CABG and PCI procedures of countries. In 2007, the mean PCI-to-CABG ratio among 24 countries throughout the world was 3.29 [3434. OECD. Health at a Glance 2009. OECD Publishing. ]. However, the ratio ranged from 0.67 in Mexico to 8.63 in Spain. Remarkably, there were severe discrepancies even in small neighbouring countries the Netherlands and Belgium, the number of CABG procedures per 100,000 inhabitants was 58.2 versus 135.4, respectively, and the number of PCI procedures 140.3 versus 435.1, respectively. There may be some differences in baseline patient characteristics accounting for part of the variance, but it is likely that it is multifactorial taking into consideration economic and reimbursement incentives, as well as clinician-related factors [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ].
As a result of such factors, patients may be subject to over- or undertreatment. Numerous studies have shown that cardiologists and surgeons sometimes inappropriately decide to perform either PCI, CABG, or treat patients medically [99. Chan PS, Brindis RG, Cohen DJ, Jones PG, Gialde E, Bach RG, Curtis J, Bethea CF, Shelton ME, Spertus JA. Concordance of physician ratings with the appropriate use criteria for coronary revascularization. J Am Coll Cardiol. 2011;57:1546-53. , 1010. Chan PS, Patel MR, Klein LW, Krone RJ, Dehmer GJ, Kennedy K, Nallamothu BK, Weaver WD, Masoudi FA, Rumsfeld JS, Brindis RG, Spertus JA. Appropriateness of percutaneous coronary intervention. JAMA. 2011;306: 53-61.
This study applied the appropriateness criteria to stenting procedures performed in the United States, showing that only ~50% of the procedures on patients with non-acute indications were classified as appropriate., 1111. Hemingway H, Crook AM, Feder G, Banerjee S, Dawson JR, Magee P, Philpott S, Sanders J, Wood A, Timmis AD. Underuse of coronary revascularization procedures in patients considered appropriate candidates for revascularization. N Engl J Med. 2001;344:645-54. , 1212. Hilborne LH, Leape LL, Bernstein SJ, Park RE, Fiske ME, Kamberg CJ, Roth CP, Brook RH. The appropriateness of use of percutaneous transluminal coronary angioplasty in New York State. JAMA. 1993;269:761-5. , 1313. Leape LL, Hilborne LH, Park RE, Bernstein SJ, Kamberg CJ, Sherwood M, Brook RH. The appropriateness of use of coronary artery bypass graft surgery in New York State. JAMA. 1993;269:753-60. , 2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ]. Substantial inter- and intrahospital variation of inappropriate rates for PCI reflect that the decision depends strongly on the treating clinician [1010. Chan PS, Patel MR, Klein LW, Krone RJ, Dehmer GJ, Kennedy K, Nallamothu BK, Weaver WD, Masoudi FA, Rumsfeld JS, Brindis RG, Spertus JA. Appropriateness of percutaneous coronary intervention. JAMA. 2011;306: 53-61.
This study applied the appropriateness criteria to stenting procedures performed in the United States, showing that only ~50% of the procedures on patients with non-acute indications were classified as appropriate.] although also on patient factors [3535. Chan PS, Rao SV, Bhatt DL, Rumsfeld JS, Gurm HS, Nallamothu BK, Cavender MA, Kennedy KF, Spertus JA. Patient and hospital characteristics associated with inappropriate percutaneous coronary interventions. J Am Coll Cardiol 2013;62:2274-81. ]. In recent studies evaluating inappropriate use of coronary revascularisation, inappropriate PCI was performed in ~10-20% and inappropriate CABG generally lower in ~1-3% [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. , 3535. Chan PS, Rao SV, Bhatt DL, Rumsfeld JS, Gurm HS, Nallamothu BK, Cavender MA, Kennedy KF, Spertus JA. Patient and hospital characteristics associated with inappropriate percutaneous coronary interventions. J Am Coll Cardiol 2013;62:2274-81. , 3636. Ko DT, Guo H, Wijeysundera HC, Natarajan MK, Nagpal AD, Feindel CM, Kingsbury K, Cohen EA, Tu JV ; Cardiac Care Network (CCN) of Ontario Variations in Revascularization Practice in Ontario (VPRO) Working Group. Assessing the association of appropriateness of coronary revascularization and clinical outcomes for patients with stable coronary artery disease. J Am Coll Cardiol. 2012;60:1876-84. ][1313. Leape LL, Hilborne LH, Park RE, Bernstein SJ, Kamberg CJ, Sherwood M, Brook RH. The appropriateness of use of coronary artery bypass graft surgery in New York State. JAMA. 1993;269:753-60. ].
The COURAGE trial demonstrated that PCI in addition to optimal medical therapy did not reduce cardiovascular events when compared to medical therapy alone in selected patients with stable coronary artery disease [1414. Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503-16.
The COURAGE trial showed that percutaneous coronary intervention on top of optimal medical therapy did not reduce the rate of adverse events in patients with evidence of myocardial ischaemia and significant coronary artery disease.], and it remains unclear whether revascularization is beneficial in patients lacking evidence of ischemia [3737. Hachamovitch R, Rozanski A, Shaw LJ, Stone GW, Thomson LE, Friedman JD, Hayes SW, Cohen I, Germano G, Berman DS. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012-24. ]. Nevertheless, revascularisation can be underused. In a summary of older studies reporting the underuse of revascularization procedures, the rate was relatively consistent at 20-40% [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ]. In a more recent study, again 31% of patients received medical therapy although revascularization with either PCI or CABG would have been appropriate [3636. Ko DT, Guo H, Wijeysundera HC, Natarajan MK, Nagpal AD, Feindel CM, Kingsbury K, Cohen EA, Tu JV ; Cardiac Care Network (CCN) of Ontario Variations in Revascularization Practice in Ontario (VPRO) Working Group. Assessing the association of appropriateness of coronary revascularization and clinical outcomes for patients with stable coronary artery disease. J Am Coll Cardiol. 2012;60:1876-84. ]. Several studies have shown that the underuse of revascularization resulted in significantly higher rates of death, non-fatal myocardial infarction, or recurrent angina during mid- to long-term follow-up [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. , 3636. Ko DT, Guo H, Wijeysundera HC, Natarajan MK, Nagpal AD, Feindel CM, Kingsbury K, Cohen EA, Tu JV ; Cardiac Care Network (CCN) of Ontario Variations in Revascularization Practice in Ontario (VPRO) Working Group. Assessing the association of appropriateness of coronary revascularization and clinical outcomes for patients with stable coronary artery disease. J Am Coll Cardiol. 2012;60:1876-84. ][1111. Hemingway H, Crook AM, Feder G, Banerjee S, Dawson JR, Magee P, Philpott S, Sanders J, Wood A, Timmis AD. Underuse of coronary revascularization procedures in patients considered appropriate candidates for revascularization. N Engl J Med. 2001;344:645-54. ].
One of the reasons why inappropriate revascularization occurs is the lack of transparency towards patients. In 60-70% of patients treated by either PCI or CABG, the alternative treatment strategy is not discussed with the patient [2727. Chandrasekharan DP, Taggart DP. Informed consent for interventions in stable coronary artery disease : problems, etiologies, and solutions. Eur J Cardiothorac Surg. 2011;39:912-7. ]. Furthermore, clinicians are often not in agreement about the appropriateness of PCI [99. Chan PS, Brindis RG, Cohen DJ, Jones PG, Gialde E, Bach RG, Curtis J, Bethea CF, Shelton ME, Spertus JA. Concordance of physician ratings with the appropriate use criteria for coronary revascularization. J Am Coll Cardiol. 2011;57:1546-53. ]. Thus, there is a need for multidisciplinary decision-making so that patients are evaluated in a collegiate environment by different specialty stakeholders. This group can consider multiple treatment options and finally form a consensus and advise on the most appropriate treatment. Central to the concept of the Heart Team is the patient and the non-paternalistic facilitation of informed treatment decisions ( Figure 1 ). Importantly, the Heart Team is not a replacement of the individual doctor-patient relationship, which remains the cornerstone of clinical care and must not be jeopardised.
Development
The Heart Team is not a novel concept in the field of cardiology. Already in the early randomised trials comparing CABG with medical therapy for stable CAD, a Heart Team was used to select patients eligible for randomisation [3838. European Coronary Study Group. Prospective randomised study of coronary artery bypass surgery in stable angina pectoris. Second interim report by the European Coronary Surgery Study Group. Lancet. 1980;2:491–5. , 3939. Murphy ML, Hultgren HN, Detre K, Thomsen J, Takaro T. Treatment of chronic stable angina. A preliminary report of survival data of the randomized Veterans Administration cooperative study. N Engl J Med. 1977;297:621–7. ]. After the introduction of PCI, which in itself was a collaboration between Andreas Grüntzig and his surgical colleagues in Zürich, randomised comparisons between the two different revascularisation strategies initiated a close partnership between the two specialties. Particularly the results from the nested registries alongside the randomised EAST, BARI and MASS-II trials pointed to the fact that decision-making as performed by the coronary Heart Team provided excellent results, even better than those achieved in the randomized trials [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ]. Not only in CAD, but also for other clinical scenarios the Heart Team grew stronger. A statement in 1995 from the American Heart Association recommended that a multidisciplinary team should evaluate patients with severe heart failure, weighing up patient characteristics and clinical features to conclude whether medical therapy, surgery, or a heart transplantation would be the best treatment [1515. Costanzo MR, Augustine S, Bourge R, Bristow M, O’Connell JB, Driscoll D, Rose E. Selection and treatment of candidates for heart transplantation. A statement for health professionals from the Committee on Heart Failure and Cardiac Transplantation of the Council on Clinical Cardiology, American Heart Association. Circulation. 1995;92:3593-612. ].
Despite these early experiences, the coronary Heart Team was never really adopted in clinical practice until only a few years ago when the SYNTAX trial regenerated a focus on the Heart Team [11. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72.
The first randomised trial comparing stenting with drug-eluting stents to coronary surgery, showing that surgery remains the preferred treatment for complex coronary artery disease.]. In the SYNTAX trial, both an interventional cardiologist and cardio-thoracic surgeon were mandated to assume that clinical equipoise with PCI and CABG could be met. If the clinicians decided that a more favourable outcome could be achieved with either PCI or CABG, that patient was not randomised but included in one of two nested registries: a PCI-ineligible CABG registry or a CABG-ineligible PCI registry. Using this design, the SYNTAX trial was able to accurately demonstrate the PCI/CABG distribution of patients with left main (LM) and/or multivessel coronary artery disease. The SYNTAX Heart Team decided that 29% of patients good not be treated in SYNTAX. Of the 3,075 patients who were revascularised in the randomised cohort and nested registries, 6.4% (5% of total) and 35% (25% of total) of patients could only undergo PCI and CABG respectively, due to a combination of comorbid and lesion specific factors ( Figure 2 ) [4040. Head SJ, Holmes DR Jr, Mack MJ, Serruys PW, Mohr FW, Morice MC, Colombo A, Kappetein AP; SYNTAX Investigators. Risk profile and 3-year outcomes from the SYNTAX percutaneous coronary intervention and coronary artery bypass grafting nested registries. JACC Cardiovasc Interv. 2012;5:618-25. ]. The Heart Team initiative has been continued in more recent ongoing trials comparing PCI and CABG, such as the EXCEL trial.
Notwithstanding the importance of the SYNTAX trial, it is essential to recognise that the Heart Team within a clinical trial is different from “real world” clinical practice. Trials are designed with the premise that it is uncertain which therapy will provide superior results. However, in the real world, patients are treated according to guidelines, and therefore some indications do not mandate a Heart Team discussion (e.g., single-vessel coronary disease without proximal left anterior descending artery involvement). A further aspect of includes the opportunities afforded by a collegiate discussion of in-house cases in terms of local governance, harmonisation of protocols and medico-legal support given by a group consensus over a unilateral decision of a lone clinician. These potential benefits enhance the applicability of the Heart Team concept for contemporary daily practice.
Tools for coronary artery disease decision making
Whether patients benefit most from PCI or CABG depends heavily on comorbidities, the complexity of CAD, left ventricular function and specific vessel involvement (e.g., LM). During a Heart Team meeting, this information is needed to obtain an objective view of the patient’s status. Several tools can be used to summarise the comorbidities, the patient’s history, presence of ischaemia, lesion complexity, and operative risk.
Specialist involvement in the Heart TeamCoronary Heart Team should include at least:
- Surgeon
- Interventional cardiologist
- Primary non-invasive cardiologist
Valvular Heart Team should include at least:
- Surgeon
- Interventional cardiologist
- Primary non-invasive cardiologist
- Image specialist
- Anaesthesiologist
Popular risk scores that are frequently used are the EuroSCORE and STS score. Both include patient characteristics (e.g., age, gender, body mass index), comorbidities (e.g., peripheral vascular disease, renal failure, left ventricular dysfunction, diabetes), previous events (e.g., recent myocardial infarction, previous surgery, previous stroke), and operative factors (e.g., combined valve surgery, AVR + CABG) to calculate an operative risk [1616. Rosenhek R, Iung B, Tornos P, Antunes MJ, Prendergast BD, Otto CM, Kappetein AP, Stepinska J, Kaden JJ, Naber CK, Acartürk E, Gohle-Bärwolf C. ESC Working Group on Valvular Heart Disease Position Paper: assessing the risk of interventions in patients with valvular heart disease. Eur Heart J. 2011;doi:10.1093/eurheartj/ehr061. ]. Using these scores, when the risk of surgery is estimated to be high, patients could be preferentially directed to undergo PCI. It is, however, crucial that decisions are not solely based on the results of these scores. Their limitations have been described extensively, and it is thus better to weigh up all relevant factors within the Heart Team. These scores, although helpful, should therefore only be used as guidance.
The SYNTAX score, established in 2005, was developed to grade the degree and complexity of CAD [1717. Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, van Dyck N, Russel ME, Mohr FW, Serruys PW. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-27. ]. Validated in the SYNTAX trial, the score demonstrated that it was a good predictor of adverse events and a useful tool to stratify which patients should receive PCI or CABG. Patients with a low SYNTAX score (0-22) can safely and efficiently undergo PCI, while those with high scores (≥33) can better undergo CABG [1818. Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Ståhle E, Dawkins KD, Mohr FW, Serruys PW, Colombo A. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125-34.
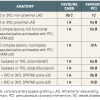
Three-year follow-up paper of the SYNTAX trial demonstrating diverging curves between stenting and surgery.]. Patients with intermediate SYNTAX scores (23-32) preferably should undergo CABG but comorbidities may direct patients towards PCI. Apart from the SYNTAX trial data, numerous studies have provided additional evidence to support the recommendation of using the SYNTAX score as a guide for decision-making [4141. Head SJ, Farooq V, Serruys PW, Kappetein AP. The SYNTAX score and its clinical implications. Heart. 2014;100:169-77. ]. The use of the SYNTAX score is now widely accepted and current guidelines on myocardial revascularisation indicate that the preferred revascularisation strategy depends on the SYNTAX score ( Table 1 ). However, more recently the SYNTAX II score has been introduced, which allows to combine the clinical characteristics (age, creatinine clearance, left ventricular function, gender, COPD, and peripheral vascular disease) of patients with the lesion complexity (SYNTAX score) to estimate long-term (e.g. 4-year) mortality [4242. Farooq V, an Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, Kappetein AP, Colombo A, Holmes DR Jr, Mack M, Feldman T, Morice MC, Stahle E, Onuma Y, Morel MA, Garcia-Garcia HM, van Es GA, Dawkins KD, Mohr FW, Serruys PW. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639-50. ]. It was found to be superior to the conventional SYNTAX score in guiding decision-making between CABG and PCI in the SYNTAX trial, and subsequently validated in the DELTA registry ( Figure 5 ).
Risk scores- STS score for risk estimate of short-term operative mortality based on clinical factors
- EuroSCORE for risk estimate of short-term operative mortality based on clinical factors
- SYNTAX score for mid- and long-term coronary lesion complexity based on angiographic factors
- SYNTAX II score for combined clinical and angiographic long-term risk estimation
Other key factors than are influential to the decision-making process, and not captured in conventional risk scores, are the patients’ preferences. Some patients are unwilling to undergo surgery because of its invasiveness, while others prefer treatment with CABG to ensure better long-term results. Moreover, patients with a short life-expectancy (e.g., malignancy) or who desire a rapid convalescence should preferably undergo PCI to improve quality of life and obviate any postoperative pain and rehabilitation. Similarly patients who desire a single definitive treatment with the lowest risk of repeat revascularisation may opt for a surgical solution. These patient risk-benefit preferences are therefore important and may form part of the next generation of risk scores.
The valvular Heart Team
As alluded to before, the Heart Team is not only a necessary component in the evaluation of patients with CAD but also those with valvular heart disease [1919. Holmes DR Jr, Mack MJ. Transcatheter valve therapy a professional society overview from the american college of cardiology foundation and the society of thoracic surgeons. J Am Coll Cardiol. 2011;58:445-55. ]. TAVI has emerged as a promising therapy to treat patients with aortic stenosis at high risk for surgery, but this relatively new intervention is not yet validated for treating intermediate risk patients [2020. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S; PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597-607.
The PARTNER B study was the first to randomise patients with severe aortic stenosis deemed too high risk for surgery to medical management or transcatheter aortic valve implantation, showing significantly better outcomes with intervention. ][2121. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ; PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187-98.
In patients at high risk for surgery, those randomised to transcatheter aortic valve implantation showed non-inferior results to those patients randomised to surgical aortic valve replacement in the PARTNER A trial.]. The selection of patients is therefore critical and many aspects of this therapy need to be discussed within a Heart Team forum. In addition to primary cardiologists, interventional cardiologists, and surgeons, the team needs to incorporate imaging specialists. Furthermore, heart failure specialists and geriatricians can sometimes be especially helpful in choosing optimal therapy within this cohort that comprises an elderly population. This expanded team should also include anaesthesiologists, who are integral to any discussion of general anaesthetic risk ( Figure 3 ).
A similar development is currently seen in the treatment of mitral regurgitation. Percutaneous repair with the MitraClip (Abbott Vascular, Santa Clara, CA, USA) has been introduced as an alternative to surgery [2222. Feldman T, Foster E, Glower DG, Kar S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L; EVEREST II Investigators. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364:1395-406. ]. Evaluation of patients in the EVEREST II trial that randomised patients between percutaneous and surgical repair was undertaken by a Heart Team. This group consisted of primary cardiologists, interventional cardiologists, surgeons, and imaging specialists (including at least one echocardiographer). In the recent European valvular guidelines the need for Heart Team decision-making for severe MR was again stressed by giving a IIb C recommendation to the statement that "percutaneous edge-to-edge procedures may be considered in patients with symptomatic severe primary MR who fulfil the echo criteria of eligibility, are judged inoperable or at high surgical risk by a ‘heart team’, and have a life expectancy greater than 1 year."
Other structural disease interventions (e.g., patent foramen ovale closure) may also benefit from systematic Heart Team discussion.
Tools for aortic valvular intervention decision making
Compared to patients with CAD, the evaluation of patients with AS using risk scores does not sufficiently enhance the decision-making process. Numerous studies have assessed the use of risk scores, including the EuroSCORE and STS score, to predict outcomes of high-risk patients that are candidates for TAVI or SAVR, but non seems to suffice in stratifying which patients may benefit most from a specific treatment. One of the main reasons is that several important factors that have an impact on clinical outcome are not included in contemporary operative risk models: porcelain aorta; general frailty; severe liver disease; a hostile chest as a result of an abnormal antomy, complications from prior surgery, radiation damage, or recurrent pleural effusions; an internal mammary artery adherent to the postertior table of the sternum; or severe pulmonary hypertension or right ventricular dysfunction [44. Brownlee S, Wennberg J, Barry M, Fisher E, Goodman D, Bynum J. Improving patient decision-making in health care: a 2011 Dartmouth Atlas report highlighting Minnesota. In; 2011. ]. Definitions for these conditions have been proposed in the latest version of standardized defnitions by the Valve Academic Research Consortium (VARC) [3030. Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2012;33:2403-18. ].
Unfortunately, an anatomical score similar to the SYNTAX score is as yet unavailable for patients with AS. As a result, the Heart Team is the only approach to weigh up comorbidities and technical feasibility according to the importance specifically for AS. Nevertheless, prediction models that can guide specialists as to what might be the most optimal treatment for the individual patient, using an expansion of current models is therefore needed.
Imaging by multi-slice computed tomography is necessary for choosing the most optimal access route (transfemoral, transapical, subclavicular, direct aortic access). Sizing of the annulus is important to ascertain whether the correct size of the prosthesis is available. The complexity of imaging expertise required underlines the value of an expanded Heart Team in valvular intervention that is not mandatory for the coronary Heart Team.
Heart team limitations
In patients with less complex CAD that are good candidates for PCI the Heart Team might not be mandatory. To avoid treatment on two different occasions, ad hoc PCI following diagnostic catheterisation could be performed without a multidisciplinary discussion, according to the 2010 ESC/EACTS revascularisation guidelines [2323. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI), Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2010;38:S1-S52. ]. This is indicated where the clinical presentation is that of an identifiable culprit lesion for an acute coronary syndrome, the presence of non-recurrent instent restenosis, and favourable single or two vessel disease (RCA, and/or non ostial Cx and LAD). However, it may be appropriate to schedule a ‘time-out’ to allow surgical consultation in the catheterization laboratory. Importantly for stable presentations and acute coronary syndromes with non-culprit vessels, diagnostic coronary angiography and therapeutic procedures should be separated, until local institutional protocols have established which patients can be left out a formal Heart Team meeting and may undergo ad hoc stenting. This may obviate the unnecessary need for systematic face-to-face discussion of all diagnostic coronary angiograms Key exceptions to this include invasive diagnostic procedures using intravascular ultrasound and/or fractional flow reserve evaluation that identify a favourable target lesion as well as cardiogenic shock.
Essential to the function of this multidisciplinary approach is that both the cardiologists and surgeons refer all appropriate patients to the Heart Team. When commencing a programme based upon this approach, to better understand the referral patterns, clinical decision-making process, and treatment disposition, all patients with a clear indication for TAVI/SAVR and PCI/CABG treatment should be sent for Heart Team discussion [2424. Bavaria JE, Szeto WY, Roche LA, Walsh EK, Buckley-Blaskovich V, Solometo LP, Burtch KE, Desai ND, Herrmann HC. The Progression of a Transcatheter Aortic Valve Program: A Decision Analysis of More Than 680 Patient Referrals. Ann Thorac Surg. 2011;92:2072-7.
The referral patterns of patients evaluated for transcatheter aortic valve implantation are crucial for observation of the decision-making process and treatment disposition, which are reported in this study.]. This initial approach is useful for benchmarking and integrating information from mortality and morbidity meetings.
Clinicians may be hesitant to participate in Heart Team meetings due to time constraints, cost considerations, and the current lack of proven benefit. Indeed, Heart Team meetings demand time and effort, but lengthy meetings can be avoided by scheduling regular meetings with only a limited number of patients [2828. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Jean Marco, Bogers AJ, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J. 2013;34:2510-8. ]. If scheduled in the ealy morning, interference with other clinical obligations will be minimized [4343. Sanchez CE, Badhwar V, Dota A, Schindler J, Chu D, Smith AJ, Lee JS, Khandhar S, Tima C, Marroquin OC, Schmidhofer M, Bhama J, Wei L, Scolieri S, Esper S, Lee A, Mulukutla SR. Practical implementation of the coronary revascularization Heart Team. Circ Cardiovasc Qual Outcomes. 2013;6:598-603. ]. In their initial experience with the coronary Heart Team, Sanchez et al. reported increasing the collaboration between surgeons and cardiologists, better unstanding the issues of both specialties and provide an educational experience [4343. Sanchez CE, Badhwar V, Dota A, Schindler J, Chu D, Smith AJ, Lee JS, Khandhar S, Tima C, Marroquin OC, Schmidhofer M, Bhama J, Wei L, Scolieri S, Esper S, Lee A, Mulukutla SR. Practical implementation of the coronary revascularization Heart Team. Circ Cardiovasc Qual Outcomes. 2013;6:598-603. ].
Tasks of the local coronary Heart Team- Benchmarking decision-making
- Mortality and morbidity conferences
- Develop local institutional protocols for ad hoc PCI
- Develop local institutional protocols, based on international guidelines, on cases that require discussion to avoid systematic discussion of all diagnostic coronary angiograms
Validation
A number randomised trials have used the Heart Team as screening tool [11. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72.
The first randomised trial comparing stenting with drug-eluting stents to coronary surgery, showing that surgery remains the preferred treatment for complex coronary artery disease., 2222. Feldman T, Foster E, Glower DG, Kar S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L; EVEREST II Investigators. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364:1395-406. ]. Unfortunately, it is difficult to design a study that demonstrates that the Heart Team is better than decision-making by individual clinicians. A comparison of outcomes between centres with or without a Heart Team discussion could be an option to validate the Heart Team, but other site- and clinician-related factors will play a confounding role. Potential study designs have been proposed but no data is yet available ( Table 2 ).
Widespread introduction of the valvular Heart Team has been, in contrast to the coronary Heart Team, less complex because of the mandates to perform and receive reimbursements for catheter-based therapies only if a Heart Team discussion took place. Were the feasibility of the coronary Heart Team within the setting of a trial has been demonstrated, only limited data is available of a ‘real-world’ coronary Heart Team. One recent study prospectively documented treatment decisions of 201 patients with complex CAD discussed after introduction of a regular Heart Team meeting [4343. Sanchez CE, Badhwar V, Dota A, Schindler J, Chu D, Smith AJ, Lee JS, Khandhar S, Tima C, Marroquin OC, Schmidhofer M, Bhama J, Wei L, Scolieri S, Esper S, Lee A, Mulukutla SR. Practical implementation of the coronary revascularization Heart Team. Circ Cardiovasc Qual Outcomes. 2013;6:598-603. ]. Indeed the SYNTAX and STS scores were used to guide treatment decisions, but a low or high SYNTAX score did not necessarily translate in a PCI or CABG recommendation, respectively ( Figure 4 ). These results are in line with the inclusion of patients in the SYTNAX registries; in the PCI registry that included only patients deemed unsuitable to undergo CABG, 43% of patients had a SYNTAX score ≥33, and in the CABG registry of patients not suitable to undergo PCI, 11% of patients had a low SYNTAX scores [4040. Head SJ, Holmes DR Jr, Mack MJ, Serruys PW, Mohr FW, Morice MC, Colombo A, Kappetein AP; SYNTAX Investigators. Risk profile and 3-year outcomes from the SYNTAX percutaneous coronary intervention and coronary artery bypass grafting nested registries. JACC Cardiovasc Interv. 2012;5:618-25. ].
One study evaluated the reproducibility of the Heart Team by discussing 50 cases in the Heart Team and reduscussing the exact same cases a year later [2525. Long J, Luckraz H, Thekkudan J, Maher A, Norell M. Heart team discussion in managing patients with coronary artery disease: outcome and reproducibility. Interact Cardiovasc Thorac Surg. 2012;14:594-8. ]. The authors reported that the recommendation was consistent in 76% of cases; but altered in 12/50 cases. In these cases the evidence to treat the respective CAD pattern was not particularly strong in favour of medical therapy, PCI, or CABG. Therefore, either an additional diagnostic test or medical therapy was recommended in 8/12 and 6/12 cases in the first and second round of discussion, respectively.
Data from Sanchez et al. [4343. Sanchez CE, Badhwar V, Dota A, Schindler J, Chu D, Smith AJ, Lee JS, Khandhar S, Tima C, Marroquin OC, Schmidhofer M, Bhama J, Wei L, Scolieri S, Esper S, Lee A, Mulukutla SR. Practical implementation of the coronary revascularization Heart Team. Circ Cardiovasc Qual Outcomes. 2013;6:598-603. ]. CABG = coronary artery bypass grafting; MT = medical therapy; PCI = percutaneous coronary intervention.
Conclusions
The Heart Team has become a popular and necessary tool for patient evaluation. Its use has been expanded from patients that present with heart failure to a wide range of indications such as coronary artery disease, aortic valve stenosis, and mitral valve regurgitation. Several tools can help guide clinicians to identify patients that will benefit most from less invasive treatment options. Scientific validation of the Heart Team is limited, and may be difficult due to the study design required. Nevertheless, the current guidelines on myocardial revascularisation both in Europe and North America [2525. Long J, Luckraz H, Thekkudan J, Maher A, Norell M. Heart team discussion in managing patients with coronary artery disease: outcome and reproducibility. Interact Cardiovasc Thorac Surg. 2012;14:594-8. , 2626. Levine GN, Bates ER, Blakenship JA, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot U, Lange R, Mauri L, Mehran R, Moussa ID, Nallamothu BK, Ting HH 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: Executive Summary. Circulation. 2011;124:2574-609. ] recommend that the Heart Team needs to systematically discuss patients with multivessel coronary disease, and the most recent European guidelines on valvular heart disease have expanded the recommendation of Heart Team decision-making for patients with aortic stenosis and mitral valve regurgitation in whom a catheter-based treatment strategy may be an option [3131. Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancelotti P, Pierard L, Price S, Schäfers HF, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppel UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2013;33:2451-96. ]. These guidelines were complied by groups consisting of interventional, and non-interventional cardiologists as well as cardiothoracic surgeons reinforcing the principle of collegiality embodied by this new approach to decision-making.
Conclusions- For coronary artery disease and valvular heart disease, the Heart Team should be used for patient evaluation
- Several risk scores can be used to guide the Heart Team during the decision-making process
- The Heart Team is a IC indication in the current guidelines on myocardial revascularisation
- Patients with severe aortic stenosis should be discussed in a Heart Team according to the latest European guidelines on valvular heart disease
- Patients with severe mitral regurgitation in whom a percutaneous treatment strategy is considered should be subjected to a Heart Team discussion
Personal perspective - Arie Pieter Kappetein
Decision-making can be difficult when there are multiple viable treatment options. Although risk scores are often used to guide treatment selection, this should be performed with caution. Complex patients should be treated in centres where a multidisciplinary team consisting of at least an interventional cardiologist, non-invasive cardiologist and cardiothoracic surgeon are present. Even though there is no data supporting the Heart Team concept, centres should quickly adopt this discussion forum to manage individual patients according to the best personalised treatment option.