Summary
During the past 30 years, percutaneous coronary interventions (PCI) and coronary artery bypass grafting (CABG) have been compared in order to identify the optimal revascularisation technique for multivessel coronary artery disease. All trials have shown that both CABG and PCI increase health-related quality of life (HRQL), with greater short-term benefits seen with PCI. The transition from balloon angioplasty, done without stents (subsequently referred to as “plain old balloon angioplasty” or POBA), to bare metal and drug-eluting stent use have progressively reduced the differences between PCI and CABG in terms of risk of repeat procedures. Since a key goal of treating patients with ischaemia is to restore a normal life for the patient as quickly as possible, risk-benefit models have evolved to provide an additional perspective for procedural choice. Risk-benefit modelling can be used to demonstrate the trade-off that physicians and patients face in choosing between the deferred benefits of reduced rates of repeat revascularisation from CABG versus delayed relief from pain or improvements in HRQL. The same modelling may be applied to high-risk patients who undergo transcatheter aortic valve replacement (TAVR). This chapter describes standard benefit measures, reviews results from randomised trials, describes how a risk-benefit model enables comparisons of the short-run benefits of PCI to the long-run benefits of CABG. Comparison between TAVR versus surgical aortic valve replacement in terms of HRQL will be also explored.
Introduction
The optimal revascularisation technique for multivessel coronary artery disease has been a matter of continual debate and investigation over the past 20 years, with advocates supporting both percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Data from the United States and Europe show that both the absolute volume and rate of percutaneous procedures have increased substantially whilst CABG rates have progressively declined [11. Ulrich MR, Brock DM, Ziskind AA. Analysis of trends in coronary artery bypass grafting and percutaneous coronary intervention rates in Washington state from 1987 to 2001. Am J Cardiol. 2003;92:836-9. , 22. Dawkins KD, Gershlick T, de Belder M, Chauhan A, Venn G, Schofield P, Smith D, Watkins J, Gray HH; Joint Working Group on Percutaneous Coronary Intervention of the British Cardiovascular Intervention Society and the British Cardiac Society. Percutaneous coronary intervention: recommendations for good practice and training. Heart. 2005;91:vi1-27. , 33. Sheridan BC, Stearns SC, Massing MW, Stouffer GA, D’Arcy LP, Carey TS. Percutaneous Coronary Intervention or Coronary Artery Bypass Grafting: Intervention in Older Persons with Acute Coronary Syndrome-Part I. Clin Geriatr. 2008;16:39-44. , 44. Sheridan BC, Stearns SC, Massing MW, Stouffer GA, D’Arcy LP, Carey TS. Percutaneous Coronary Intervention or Coronary Artery Bypass Grafting: Intervention in Older Persons with Acute Coronary Syndrome-Part II. Clin Geriatr. 2008;16:40-6. ]. These trends indicate a growing preference for PCI over CABG for many patients and their treating physicians, especially for patients older than 65 years [55. Gerber Y, Rihal CS, Sundt TM 3rd, Killian JM, Weston SA, Therneau TM, Roger VL. Coronary Revascularization in the Community: A Population-Based Study, 1990 to 2004. J Am Coll Cardiol. 2007;50:1223-9. ].
Risk-benefit models allow the treating physician to assign a risk score to a patient grading them in terms of occurrence of events or benefits and to give patient feedback, namely in terms of benefit and risk for various treatment options. Various scores have been developed to estimate the tangible benefit derived from a medical therapeutic intervention for a patient (e.g. the SF-36, Seattle Angina Questionnaire, etc.). These scores have been used to measure the impact of health on quality of life (QoL) and to compare CABG versus PCI. During the past 20 years, PCI has undergone progressive technological improvements from POBA to the subsequent introduction of bare metal and drug-eluting stents. Risk-benefit assessments have continued to show a progressive reduction in the superiority of CABG over PCI, making the benefits from PCI a more tangible therapeutic option for patients.
The main goal for treating patients with ischaemia is to restore the patient to as normal a QoL as possible. As a consequence, evidence of benefits and risks which are meaningful from the patient’s perspective are important considerations in the comparison of treatment strategies.
Measures for benefit evaluation
Benefits from medical procedures may be measured with either generic or disease-specific measures of health outcomes. Disease-specific measures have the advantage of being more sensitive to improvements in aspects of health which may most likely be affected by the proposed intervention; conversely, many social scientists argue that generic measures of a broader spectrum of health are only more relevant for policy-making decisions [66. Gold MR, Russel LB, M.C. SJEW. Cost effectiveness in health and medicine. New York; Oxford University Press. 1996. ]. Both types of measures are ultimately useful in understanding relative benefits. The commonly used measures are therefore described briefly below.
GENERIC MEASURES OF HEALTH OUTCOME
SF-36
The short form-36 health survey is a survey of patient health based on 36 questions (http://www.sf-36.org/). The measure yields an 8-scale profile of functional health and wellbeing scores as well as psychometrically-based physical and mental health summary measures and a preference-based health utility index. Each scale is directly transformed into a 0 to 100 scale on the assumption that each question carries equal weight. The eight sections are: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, social role functioning, and mental health. ( Figure 1 )
The SF-36 was constructed to satisfy minimum psychometric standards necessary for group comparisons. The eight health concepts were selected from forty included in the Medical Outcomes Study. Those chosen represent the most frequently measured concepts in widely-used health surveys and those most affected by disease and treatment [77. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83. , 88. Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33:AS264-79. ].
The experiences to date with SF-36 have been documented in nearly 4,000 publications. The SF-36 was also judged to be the most widely evaluated generic patient assessed health outcome measure in a bibliographic study of the growth of QoL measures, published in the British Medical Journal [99. Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ. 2002;324:1417. ].
In 1996, version 2.0 of the SF-36 was introduced to correct deficiencies identified in the original version. The improvements were implemented after careful study using both qualitative and quantitative methods. Briefly, the major improvements included:
- improvements in instructions and questionnaire items to shorten and simplify the wording and make them more familiar and less ambiguous
- an improved layout for questions and answers in the self-administered forms which makes them easier to read and complete, and reduces the potential for missing responses
- greater comparability with translations and cultural adaptations widely used
- five-level response choices (in place of dichotomous response choices) for seven items in the two role functioning scales
- five-level (in place of six-level) response categories to simplify items in the mental health and vitality scales
Nevertheless, the SF-36 has some limitations, especially the fact that it does not consider sleep impairment and that it may have a low response rate in people older than 65 years.
The SF-36 has been simplified into the SF-12, focusing specifically in 12 items related to physical component summary and mental component summary scales. The SF12 includes only four of the original eight sections: body pain, general health, vitality, and social functioning. This simplified survey showed a relative validity coefficient that was approximately 10% below those observed for the SF-36. However, for studies with large sample sizes (e.g. n=500), the difference in reliability between SF-12 and SF-36 is less, because confidence intervals around group averages are determined largely by the sample size.[1010. Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey of Scales and Preliminary Construction Tests of Reliability and Validity. Med Care. 1996;34:220–33. ]
EQ-5D
EuroQol-5D (EQ-5D) is a standardised instrument for measuring health outcome. Applicable to a wide range of health conditions and treatments, it provides a simple descriptive profile and a single index value for health status. It is designed for self-completion by respondents and is ideally suited for use in postal surveys, in clinics and in face-to-face interviews. It is cognitively simple, taking only a few minutes to complete and with instructions to respondents included in the questionnaire.
An EQ-5D health state may be converted to a single summary index by applying a formula which attaches preference weights to each level in each domain, based on the evaluation of EQ-5D health states from general population samples. The standardised extended version, designed for the collection of health state values, uses a VAS rating scale – a vertical 20 cm visual analogue scale with the end points labelled best imaginable health state at the top and worst imaginable health state at the bottom and having numeric values of 100 and 0 respectively.
Nottingham Health Profile
The Nottingham Health Profile was developed for use in epidemiological studies of health and disease [1111. Hunt SM, McEwen J. The development of a subjective health indicator. Sociol Health Illn. 1980;2:231-46. ]. It consists of two parts. The first part contains 38 yes/no questions regarding pain, physical mobility, emotional reactions, energy, social isolation and sleep. The second part contains 7 yes/no questions concerning daily living problems. The two parts may be used independently. Part I may be scored using weighted values and gives a range of possible scores from zero (poor health) to 100 (good health).
Kansas City Cardiomyopathy Questionnaire
Kansas City Cardiomyopathy Questionnaire (KCCQ) is a 23-item, self-administered instrument that quantifies physical function, symptoms (frequency, severity and recent change), social function, self-efficacy and knowledge, and QoL. It provides a measure of the health status of heart failure and it has been used and validated for patients with severe aortic stenosis. Its range is from 0 to 100, with higher scores indicating a lower burden of symptoms and a better QoL.[1212. Arnold S V, Spertus JA, Lei Y, Allen KB, Chhatriwalla AK, Leon MB, Smith CR, Reynolds MR, Webb JG, Svensson LG, Cohen DJ. Use of the Kansas City Cardiomyopathy Questionnaire for Monitoring Health Status in Patients With Aortic Stenosis. Circ Hear Fail. 2012;6:61–7. ]
DISEASE-SPECIFIC MEASURES OF HEALTH OUTCOME
A number of disease-specific measures exist for different cardiovascular conditions. As an example, we describe the Seattle Angina Questionnaire below.
Seattle Angina Questionnaire (SAQ)
The Seattle Angina Questionnaire is a HRQL measure for patients with coronary artery disease developed by John Spertus as a research project during his cardiology fellowship and masters of public health studies in Seattle [1313. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333-41. ]. The questionnaire is a 19-item self-administered questionnaire measuring five dimensions of coronary artery disease:
- physical limitation: a measure of how much a patient’s condition is hampering his/her ability to do what he/she wants to do
- angina stability: a measure of whether a patient’s symptoms change over time
- angina frequency: a measure of how often a patient has symptoms
- treatment satisfaction: a measure of how well a patient understands his/her care and what he/she thinks of it
- disease perception: a measure of the overall impact of a patient’s condition on a patient’s interpersonal relationships and state of mind
Importantly, the Seattle Angina Questionnaire physical limitation scale captures activity limitations specific to coronary artery disease, whereas the generic health measures reflect the effects of other co-morbid conditions. If the goal is to understand the impact of treatment on the disease being treated, the use of a disease-specific measure is particularly important in patients with multiple medical problems. For example, if a patient with both rheumatoid arthritis and coronary disease has a flare-up of his/her arthritis without a change in the coronary artery disease, the SF-36 would detect a marked decrease in the patient’s activity. This change in activity could be mistakenly interpreted as a worsening of the patient’s coronary disease by SF-36, but not by the Seattle Angina Questionnaire.
Measures of health outcomeEvaluating benefits from medical procedures
- Disease-specific measures of health outcomes
-more sensitive to improvements in aspects of health which may be most likely to be affected by the proposed intervention
- Generic measures of health outcomes
-broader spectrum, more relevant for policy decisions
Existing evidence of impact of revascularisation on patients' health and quality of life
Multiple studies have demonstrated improvements in QoL from pre-procedure to post-procedure for both PCI and CABG, when compared to medical treatment [1414. Strauss WE, Fortin T, Hartigan P, Folland ED, Parisi AF. A comparison of quality of life scores in patients with angina pectoris after angioplasty compared with after medical therapy. Outcomes of a randomized clinical trial. Veterans Affairs Study of Angioplasty Compared to Medical Therapy Investigators. Circulation. 1995;92: 1710-9. , 1515. Kiebzak GM, Pierson LM, Campbell M, Cook JW. Use of the SF36 general health status survey to document health-related quality of life in patients with coronary artery disease: effect of disease and response to coronary artery bypass graft surgery. Heart Lung. 2002;31:207-13. , 1616. Seto TB, Taira DA, Berezin R, Chauhan MS, Cutlip DE, Ho KK, Kuntz RE, Cohen DJ. Percutaneous coronary revascularization in elderly patients: impact on functional status and quality of life. Ann Intern Med. 2000;132:955-8. ]. For PCI, the magnitude of improvement in terms of reduced risk of repeat revascularisation depends on the technology used (POBA, BMS or DES). With CABG, pre-operative assessment of personality factors, including denial, optimism, control and need for support, appears to be predictive of psychological outcome raising the possibility of individually- tailored interventions for those patients at potential risk of post-operative psychological problems [1717. Duits AA, Boeke S, Taams MA, Passchier J, Erdman RA. Prediction of quality of life after coronary artery bypass graft surgery: a review and evaluation of multiple, recent studies. Psychosom Med. 1997;59:257-68. ]. Of note is that whilst women are reported to be more severely ill at the time of CABG when compared to men, both reported similar physical and psychosocial functioning six months after surgery [1818. Ayanian JZ, Guadagnoli E, Cleary PD. Physical and psychosocial functioning of women and men after coronary artery bypass surgery. JAMA. 1995;274:1767-70. ].
Comparisons of PCI and CABG in terms of QoL could provide tangible feedback for the patients in terms of risks and benefits derived from these revascularisation procedures. More specifically, a particular patient’s perception of QoL may be different after CABG or PCI, and may vary at different points in time following initial revascularisation (i.e., whilst all patients may want to return to normal function as quickly as possible, some patients may place greater value on potentially not having to have a repeat revascularisation in the future). Differences in QoL outcomes may therefore provide helpful information for the selection of a revascularisation procedure.
RISK BENEFIT ASSESSMENT IN PRE-STENT ERA (POBA)
The coronary angioplasty versus bypass revascularisation investigation (CABRI) trial demonstrated equivalent one-year QoL outcomes for patients with multivessel disease and patients randomised to PCI or CABG. This comparison used the Nottingham health profile, which was evaluated at only two time points (baseline and 1-year follow-up) [1919. Währborg P. Quality of life after coronary angioplasty or bypass surgery. 1-year follow-up in the Coronary Angioplasty versus Bypass Revascularization investigation (CABRI) trial. Eur Heart J. 1999;20:653-8.
Quality of life between PCI and CABG in POBA era.].
The same kind of analysis was performed in patients from the bypass angioplasty revascularisation investigation (BARI) trial, randomised to CABG or PCI. In this case, although PCI patients returned to work faster, after the first three months the proportion of patients employed and the number of hours spent in employment were equivalent between the PCI and CABG groups. A greater relief from angina was noted early after bypass surgery compared to after PCI. However, relief from angina and improved functional status did not appear sufficient to preserve long-term employment [2020. Hlatky MA, Rogers WJ, Johnstone I, Boothroyd D, Brooks MM, Pitt B, Reeder G, Ryan T, Smith H, Whitlow P, Wiens R, Mark DB. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. Bypass Angioplasty Revascularization Investigation (BARI) Investigators. N Engl J Med. 1997;336:92-9.
Quality of life between PCI and CABG in POBA era.]. More interestingly, functional status evaluation of these patients using the Duke activity status index (a 12-item scale with total scores ranging from 0 to 58.2 evaluating the ability to perform common activities of daily living) [1919. Währborg P. Quality of life after coronary angioplasty or bypass surgery. 1-year follow-up in the Coronary Angioplasty versus Bypass Revascularization investigation (CABRI) trial. Eur Heart J. 1999;20:653-8.
Quality of life between PCI and CABG in POBA era., 2020. Hlatky MA, Rogers WJ, Johnstone I, Boothroyd D, Brooks MM, Pitt B, Reeder G, Ryan T, Smith H, Whitlow P, Wiens R, Mark DB. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. Bypass Angioplasty Revascularization Investigation (BARI) Investigators. N Engl J Med. 1997;336:92-9.
Quality of life between PCI and CABG in POBA era.] demonstrated that the early significant difference in improvement of the Duke activity status index in favour of CABG with respect to PCI disappeared at 5 years follow-up [2020. Hlatky MA, Rogers WJ, Johnstone I, Boothroyd D, Brooks MM, Pitt B, Reeder G, Ryan T, Smith H, Whitlow P, Wiens R, Mark DB. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. Bypass Angioplasty Revascularization Investigation (BARI) Investigators. N Engl J Med. 1997;336:92-9.
Quality of life between PCI and CABG in POBA era.].
The randomised intervention treatment of angina (RITA) trial compared initial policies of PCI and CABG in 1,011 patients with angina. Although CABG, when compared to PCI, resulted in improved long-term outcomes, namely death, myocardial infarction and prevalence of angina, the patient’s health and recovery time were reported to be better and faster with PCI [2323. Coronary angioplasty versus coronary artery bypass surgery: the Randomized Intervention Treatment of Angina (RITA) trial. Lancet. 1993;341:573-80. , 2424. Pocock SJ, Henderson RA, Seed P, Treasure T, Hampton JR. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation. 1996;94:135-42.
Quality of life between PCI and CABG in POBA era.]. In particular, at one month CABG patients were less physically active, with greater coronary-related unemployment and lower mean exercise time compared to PCI patients [2424. Pocock SJ, Henderson RA, Seed P, Treasure T, Hampton JR. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation. 1996;94:135-42.
Quality of life between PCI and CABG in POBA era.]. These differences in terms of quality of life disappeared at longer follow-up.
Conversely, the Emory angioplasty versus surgery trial (EAST) found that patients randomised to PCI had some QoL impairment compared with those randomised to CABG: fewer patients in this group felt their recoveries were complete due to less complete revascularisation with angioplasty, resulting in more frequently occurring angina at one year. However, compared to CABG patients, PCI patients were more optimistic about their health. This difference may relate to the more invasive nature of CABG and the resulting psychological impact [2525. Weintraub WS, Mauldin PD, Becker E, Kosinski AS, King SB 3rd. A comparison of the costs of and quality of life after coronary angioplasty or coronary surgery for multivessel coronary artery disease. Results from the Emory Angioplasty Versus Surgery Trial (EAST). Circulation. 1995;92:2831-40.
Quality of life between PCI and CABG in POBA era.]. This data on QoL was collected and evaluated three years after randomisation rather than immediately after the procedure.
Borkon et al compared the recovery of health status after PCI and CABG, finding improved symptom control after CABG compared with PCI: specifically, CABG patients were able to attain better physical functioning and QoL one year after their procedure [2626. Borkon AM, Muehlebach GF, House J, Marso SP, Spertus JA. A comparison of the recovery of health status after percutaneous coronary intervention and coronary artery bypass. Ann Thorac Surg. 2002;74:1526-30. ]. The authors demonstrated that the functional and QoL limitations imposed by greater symptoms in the PCI group were mostly attributable to restenosis, and that the QoL outcomes did not differ between CABG patients and those PCI patients who did not experience restenosis [2626. Borkon AM, Muehlebach GF, House J, Marso SP, Spertus JA. A comparison of the recovery of health status after percutaneous coronary intervention and coronary artery bypass. Ann Thorac Surg. 2002;74:1526-30. ]. Within this analysis, the monthly assessment of SAQ allowed for a careful description of the course of recovery after revascularisation, the detection of a one month reduction in physical function associated with CABG, and the impact of restenosis upon the symptom control and QoL in PCI patients.
RISK BENEFIT ASSESSMENT IN THE BARE METAL STENT ERA
With the introduction of the bare metal stent, the risk of repeat revascularisation following PCI was significantly reduced compared with POBA. The MASS-II trial, which compared CABG and PCI with BMS and medical treatment, concluded that both CABG and PCI exhibited greater HRQL improvement at one year compared with medical treatment. The CABG group reported the most improved HRQL [2727. Favarato ME, Hueb W, Boden WE, Boden WE, Lopes N, Noqueira CR, Takiuti M, Góis AF, Borges JC, Favarato D, Aldrighi JM, Olivéira SA, Ramires JA. Quality of life in patients with symptomatic multivessel coronary artery disease: a comparative post hoc analyses of medical, angioplasty or surgical strategies-MASS II trial. Int J Cardiol. 2007;116:364-70.
Quality of life between PCI and CABG in POBA era.]. The SOS trial also showed that both CABG and PCI resulted in significant improvements in angina-related health status at six months and one year after intervention. CABG was again more effective than PCI in relieving angina, increasing physical functioning and improving QoL [2828. Zhang Z, Mahoney EM, Stables RH, Booth J, Nugara F, Spertus JA, Weintraub WS. Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: one-year results from the Stent or Surgery trial. Circulation. 2003;108:1694-700. ].
Both risks and benefits were assessed from the arterial revascularisation therapies study (ARTS) I trial, comparing CABG and PCI with BMS implantation in patients with multivessel disease [2929. Serruys PW, Ong AT, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, Schönberger JP, Buller N, Bonser R, Disco C, Backx B, Hugenholtz PG, Firth BG, Unger F. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575-81. ]. At five years, there was no difference in mortality, myocardial infarction or stroke between PCI and CABG. However, increased rates of repeat revascularisation were observed in the PCI group. The SF-36 was evaluated at 1, 6, 12 and 36 months [3030. van Domburg RT, Daemen J, Pedersen SS, Bressers M, van Herwerden LA, Firth BG, Unger F, Serruys PW. Short- and long- term health related quality-of-life and anginal status after randomisation to coronary stenting versus bypass surgery for the treatment of multivessel disease: results of the Arterial Revascularisation Therapy Study (ARTS). EuroIntervention. 2008;3:506-11.
Quality of life between PCI and CABG in BMS era.]. In this analysis, both PCI and CABG exhibited a significant improvement HRQL and angina status. ( Figure 2 ) In particular, improvements were clear immediately following the revascularisation procedure with PCI compared to CABG. However, at one month after the procedure, the HRQL evaluation detected a larger drop in both physical and mental functioning with CABG compared to PCI. At six months the HRQL after CABG was at the same level as after PCI. Between six months and twelve months patients who underwent CABG had, in general, a better HRQL compared to those who underwent PCI, with most of these differences being attributable to repeat interventions in the stent group. In a further sub-analysis, the difference in HRQL between CABG patients and those PCI patients who did not experience restenosis disappeared. ( Figure 3 )
With regard to the risk of restenosis following PCI, Spertus et al demonstrated a significant relationship between the pre-procedural risk of restenosis and the relative benefits of CABG and PCI with respect to a patient’s one year health status [3131. Spertus JA, Nerella R, Kettlekamp R, House J, Marso S, Borkon AM, Rumsfeld JS. Risk of restenosis and health status outcomes for patients undergoing percutaneous coronary intervention versus coronary artery bypass graft surgery. Circulation. 2005;111:768-73.
Importance of the risk of restenosis for the quality of life evaluation between PCI and CABG.]. They developed a risk score, based on eight clinical characteristics (STEMI diagnosis, diabetes, daily angina, age <55 years, prior PCI, weekly/monthly angina, male sex, and multivessel coronary artery disease), assigning each a different statistical weighting. By categorising the patients according to this score, they demonstrated no differences in SAQ angina frequency scores amongst patients at a low risk of restenosis. Conversely, in patients at intermediate risk of restenosis, CABG was associated with significantly less frequent angina and better QoL compared with PCI. Amongst patients at a higher risk of restenosis, even larger differences in one year angina and quality of life in favour of CABG were observed [3131. Spertus JA, Nerella R, Kettlekamp R, House J, Marso S, Borkon AM, Rumsfeld JS. Risk of restenosis and health status outcomes for patients undergoing percutaneous coronary intervention versus coronary artery bypass graft surgery. Circulation. 2005;111:768-73.
Importance of the risk of restenosis for the quality of life evaluation between PCI and CABG.].
In high-risk patients with medically refractory ischaemia, when randomised to PCI versus CABG, their baseline higher risk was translated into a higher rate of events at follow-up, so that the balance of risk versus benefit changed. The angina with extremely serious operative mortality (AWESOME) study included high-risk patients with medically refractory angina who were typically excluded from other trials (prior heart surgery, age > 70, ejection fraction < 0.35, MI within seven days and/or need for pre-procedure intra-aortic balloon pressure). This study found equivalent HRQL outcomes for both PCI and CABG at six months [3232. Rumsfeld JS, Magid DJ, Plomondon ME, Sacks J, Henderson W, Hlatky M, Sethi G, Morrison DA; Department of Veterans Affairs Angina With Extremely Serious Operative Mortality (AWESOME) Investigators. Health-related quality of life after percutaneous coronary intervention versus coronary bypass surgery in high-risk patients with medically refractory ischemia. J Am Coll Cardiol. 2003;41:1732-8. ].
Interestingly, although survival did not significantly differ in diabetic patients who underwent CABG or PCI [3333. Sedlis SP, Morrison DA, Lorin JD, Esposito R, Sethi G, Sacks J, Henderson W, Grover F, Ramanathan KB, Weiman D, Saucedo J, Antakli T, Paramesh V, Pett S, Vernon S, Birjiniuk V, Welt F, Krucoff M, Wolfe W, Lucke JC, Mediratta S, Booth D, Murphy E, Ward H, Miller L, Kiesz S, Barbiere C, Lewis D; Investigators of the Dept. of Veterans Affairs Cooperative Study #385, the Angina With Extremely Serious Operative Mortality Evaluation (AWESOME). Percutaneous coronary intervention versus coronary bypass graft surgery for diabetic patients with unstable angina and risk factors for adverse outcomes with bypass: outcome of diabetic patients in the AWESOME randomized trial and registry. J Am Coll Cardiol. 2002;40:1555-66. ], diabetes was found to be a predictor of worse physical health status in the overall study population. In particular, a trend towards a worse physical health status was seen in diabetics assigned to CABG [3333. Sedlis SP, Morrison DA, Lorin JD, Esposito R, Sethi G, Sacks J, Henderson W, Grover F, Ramanathan KB, Weiman D, Saucedo J, Antakli T, Paramesh V, Pett S, Vernon S, Birjiniuk V, Welt F, Krucoff M, Wolfe W, Lucke JC, Mediratta S, Booth D, Murphy E, Ward H, Miller L, Kiesz S, Barbiere C, Lewis D; Investigators of the Dept. of Veterans Affairs Cooperative Study #385, the Angina With Extremely Serious Operative Mortality Evaluation (AWESOME). Percutaneous coronary intervention versus coronary bypass graft surgery for diabetic patients with unstable angina and risk factors for adverse outcomes with bypass: outcome of diabetic patients in the AWESOME randomized trial and registry. J Am Coll Cardiol. 2002;40:1555-66. ]. Consequently it was potentially demonstrated that the survival benefit in diabetics after CABG surgery may be partially offset by a worse HRQL.
The subsequent introduction of bare metal stents in PCI procedures resulted in some additional value of PCI when compared to CABG. In particular, the rate of revascularisation procedures was reduced when compared to POBA. This, however, did not reach the level to show equivalency with CABG. Nevertheless, PCI patients showed a markedly better HRQL in the short-term period, with patients with a low risk of restenosis maintaining a higher HRQL at longer term follow-up.
RISK BENEFIT ASSESSMENT IN THE DRUG-ELUTING STENT ERA: INSIGHTS FROM ARTS-II
The introduction of the first drug-eluting stent (sirolimus-eluting stent, SES) significantly reduced rates of repeat revascularisation rates after stenting, leading to the need for a randomised comparison between CABG and PCI with SES [3434. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, Molnàr F, Falotico R; RAVEL Study Group. Randomized study with the sirolimus-coated bx velocity balloon-expandable stent in the treatment of patients with de novo native coronary artery lesions. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002;346:1773-80. ]. Although not a randomised trial, the ARTS-II study was designed to make the results comparable to the ARTS-1 study, namely the application of the same inclusion and exclusion criteria, the same protocol definitions and the same primary endpoints as the ARTS-I trial, in order to make the results comparable to the ARTS-I study [3535. Serruys PW, Lemos PA, van Hout BA. Sirolimus eluting stent implantation for patients with multivessel disease: rationale for the Arterial Revascularisation Therapies Study part II (ARTS II). Heart. 2004;90:995-8. , 3636. Serruys PW, Daemen J, Morice MC, De Bruyne B, Colombo A, Macaya C, Richardt G, Fajadet J, Hamm C, Dawkins KD, Vranckx P, Bressers M, van Domburg R, Schuijer M, Wittebols K, Pieters M, Stoll HP. Three-year follow-up of the ARTS-II# - sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. EuroIntervention. 2008;3:450-9. ].
During the 3-year follow-up of ARTS-II, SES patients experienced significantly greater improvements in HRQL and angina status compared to CABG and, from six months onwards, were at the same level as the CABG patients [3737. van Domburg RT, Daemen J, Morice MC, de Bruyne B, Colombo A, Macaya C, Richardt G, Fajadet J, Hamm C, van Es GA, Wittebols K, Macours N, Stoll HP, Serruys PW. Short- and long-term health related quality-of-life and anginal status of the Arterial Revascularisation Therapies Study part II, ARTS-II; sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. EuroIntervention. 2010;5:962-7.
Quality of life between PCI and CABG in DES era.]. Most of the differences, as expected, were attributed to the lower need for repeat revascularisation after SES implantation. ( Figure 4 ) The incidence of angina status was shown to be similar between CABG and SES at six months compared to BMS patients at three years, 10% of the SES patients sustained recurrence of their angina vs. 13% of the CABG patients (p=ns), compared with 21% of the BMS patients (p<0.05). ( Figure 5 )
This analysis highlighted that the availability of DES is an important consideration in the choice of treatment of coronary disease, and confirmed that the differences in outcomes in the BMS era pertained primarily to rates of restenosis [3737. van Domburg RT, Daemen J, Morice MC, de Bruyne B, Colombo A, Macaya C, Richardt G, Fajadet J, Hamm C, van Es GA, Wittebols K, Macours N, Stoll HP, Serruys PW. Short- and long-term health related quality-of-life and anginal status of the Arterial Revascularisation Therapies Study part II, ARTS-II; sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. EuroIntervention. 2010;5:962-7.
Quality of life between PCI and CABG in DES era.]. The patients at a high restenosis risk therefore incurred a more substantial benefit from the use of DES. However, a major limitation of this analysis is that the comparison was with a historical cohort. This may potentially be misleading, due to the advances in procedural techniques and post-operative treatment. The synergy between percutaneous coronary intervention with Taxus and cardiac surgery (SYNTAX) trial, comparing surgery with paclitaxel-eluting stents in 1800 patients with three-vessel or left main coronary artery disease, provided more information for the risk-benefit balance in the decision-making process. In the SYNTAX trial, health status was assessed at baseline, 1, 6, 12, 36 months and 5 years using the SAQ and SF-36. [3838. Abdallah MS, Wang K, Magnuson EA, Osnabrugge RL, Kappetein AP, Morice MC, Mohr FA, Serruys PW, Cohen DJ. Quality of Life After Surgery or DES in Patients With 3-Vessel or Left Main Disease. J Am Coll Cardiol. 2017;69:2039–50. ] The extent of improvement in SAQ angina frequency scores was slightly greater with CABG than with PCI with paclitaxel-eluting stents. Interestingly, in adjusted analyses, patients who underwent repeat revascularization had worse angina frequency scores than patients who did not in both treatment groups. Similarly, among patients who did not undergo repeat revascularization, patients treated with CABG still had better angina relief at 12 months than patients treated with PCI, but with an adjusted between-group difference similar to the treatment effect in the overall population. These findings suggest that some of the anti-anginal benefits of CABG may result from mechanisms unrelated to relief of myocardial ischemia (eg, denervation, placebo effects).[3939. Arnold SV, Magnuson EA, Wang K, Serruys PW; Kappetein AP, Mohr FW, Cohen DJ. Do differences in repeat revascularization explain the antianginal benefits of bypass surgery versus percutaneous coronary intervention? Implications for future treatment comparisons. Circulation. 2012;5:267-275. ]
In addition, the strength of association between repeat revascularization and angina was greater among patients treated with CABG as compared with those treated with PCI, indicating that the end point of repeat revascularization has a different clinical impact based on the original treatment. This may indicate a different threshold for physicians to consider re-intervention or, perhaps, by patients to seek medical evaluation after CABG versus PCI. For this reason, the endpoint of repeat revascularization seems to play a limited role as an indirect measure of health outcomes between these 2 revascularization strategies.
It is of note that bioresorbable vascular scaffolds have shown reduced cumulative angina rates at 1 year, evaluated by SAQ, as compared to the metallic stent group (72 [2929. Serruys PW, Ong AT, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, Schönberger JP, Buller N, Bonser R, Disco C, Backx B, Hugenholtz PG, Firth BG, Unger F. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575-81. ] vs. 50 [2929. Serruys PW, Ong AT, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, Schönberger JP, Buller N, Bonser R, Disco C, Backx B, Hugenholtz PG, Firth BG, Unger F. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575-81. ], p=0.04). [4040. Serruys PW; Chevalier B, Dudek D, Cequier A, Carrie D, Iniguez A, Dominici M, van der Schaaf RJ, Haude M, Wasungu L; Veldhof S, Peng L, Staehr P, Grundeken M, Ushibashi Y, Garcia-Garcia HM, Onuma Y. A bioresorbable everolimus-eluting scaffold versus a metallic everolimus-eluting stent for ischaemic heart disease caused by de-novo native coronary artery lesions (ABSORB II): an interim 1-year analysis of clinical and procedural secondary outcomes from a randomised controlled trial. Lancet. 2015;385:43-54 ] However, this observation was not confirmed in the ABSORB-IV trial, which comparing everolimus-eluting bioresorbable scaffolds vs. cobalt-chromium everolimus-eluting stents did not show any difference in adjudicated angina at 1-year (20.4% BRS vs 20.3% EES) between the two groups. [4141. Stone GW, Ellis SG, Gori T, Metzger DC, Stein B, Erickson M, Torzewski J, Jr JW, Lawson W, Broderick TM, Kabour A, Piegari G, Cavendish J, Bertolet B, Choi JW, Marx SO. Blinded outcomes and angina assessment of coronary bioresorbable scaffolds : 30-day and 1-year results from the ABSORB IV randomised trial. Lancet. 2018;6736:1–11. ]
Assessments of risks and benefits traditionally do not incorporate the diverse points of view of individual patients. However, in the decision-making process, the point of view of the patient is paramount as many patients may not be willing to undergo the greater initial recovery period associated with CABG, when compared with PCI, to achieve the margin of improved health status after recovery. Conversely, others may value the long-term HRQL highly and be particularly willing to endure the short-term pain associated with CABG.
Given the improvements in outcomes from PCI over time, reassessments of the benefits and risks from PCI and CABG are warranted. Furthermore, given some of the differences in risks and benefits from the procedures (e.g., more rapid return to normal function from PCI versus lower risk of repeat revascularisation from CABG, albeit with a decreasing difference as PCI technology improves), the tailoring of the decision-making process on an individual patient basis may be warranted. Such an assessment may balance the larger upfront risk and delay in returning to normal function associated with CABG against the risk of repeat revascularisation and residual angina with PCI.
Revascularisation and quality of lifeMultiple studies have demonstrated improvements in QoL from pre-procedure to post-procedure for both PCI and CABG, when compared to medical treatment
- PCI clearly improves the QoL immediately following the revascularisation procedure
- CABG has less risk of repeat revascularisation but a higher comorbidity in the short term compared to PCI
- Given the improvements in outcomes from PCI over time (e.g., introduction of BMS and DES), reassessments of the benefits and risks from PCI versus CABG would be warranted
New approaches in risk/benefit evaluation
All randomised controlled trials have demonstrated equivalent mortality after CABG and PCI. Both CABG and PCI improve HRQL for patients with multivessel disease, although in the long term CABG was demonstrated to have lower rates of revascularisation when compared to bare metal stents [4242. Legrand VMG, Serruys PW, Unger F, van Hout BA, Vrolix MC, Fransen GM, Nielsen TT, Paulsen PK, Gomes RS, de Queiroz e Melo JM, Neves JP, Lindeboom W, Backx B; Arterial Revascularization Therapy Study (ARTS) Investigators. Three-Year Outcome After Coronary Stenting Versus Bypass Surgery for the Treatment of Multivessel Disease. Circulation. 2004;109:1114-20. ]. However, the acceptance of these deferred benefits of reduced rates of repeat revascularisation requires the recognition of sustaining a higher morbidity in the short term. These morbidities are predominantly related to delayed relief from pain or improvement in HRQL in the time period immediately following the procedure.
From the patient’s perspective, it would be important to translate the risk and benefit resulting from different revascularisation procedures to something more tangible and easy to understand. For example, measures of pain relief may potentially be a good candidate for benefit estimation for patients to understand rather than the scores derived from the various benefit-estimating assessments.
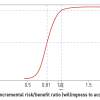
Economists have become interested in using probabilistic methods to portray the trade-off between risks and benefits as well as the implicit evaluation that patients make when one technique is chosen over a competitor. A risk-benefit acceptability curve (RBAC), analogous to the cost-effectiveness acceptability curves [4343. Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves - facts, fallacies and frequently asked questions. Health Economics. 2004;13:405-15. ], has been developed and applied to the risk benefit analysis of PCI over CABG [4444. Federspiel JJ, Stearns SC, van Domburg RT, Sheridan BC, Lund JL, Serruys PW. Risk-benefit trade-offs in revascularisation choices. EuroIntervention. 2011;6:936-41.
Introduction to the risk-benefit curves in the trade-off choice between PCI and CABG from the patient’s perspective.]. The RBAC provides estimates of the probability that a particular approach such as PCI is viewed by the consumer as being risk-effective over different preference thresholds for the risk-benefit trade-offs identified. In particular, the estimates may be useful to physicians in explaining trade-offs between risks and benefits of alternative treatments to their patients.
ARTS-I
The RBAC analysis was applied for the first time to the choice of CABG versus PCI in the data from the ARTS-I trial for patients who were implanted with bare metal stents [4444. Federspiel JJ, Stearns SC, van Domburg RT, Sheridan BC, Lund JL, Serruys PW. Risk-benefit trade-offs in revascularisation choices. EuroIntervention. 2011;6:936-41.
Introduction to the risk-benefit curves in the trade-off choice between PCI and CABG from the patient’s perspective.]. In contrast to the previous analysis of the risks and benefits of this trial illustrated in the previous section [3030. van Domburg RT, Daemen J, Pedersen SS, Bressers M, van Herwerden LA, Firth BG, Unger F, Serruys PW. Short- and long- term health related quality-of-life and anginal status after randomisation to coronary stenting versus bypass surgery for the treatment of multivessel disease: results of the Arterial Revascularisation Therapy Study (ARTS). EuroIntervention. 2008;3:506-11.
Quality of life between PCI and CABG in BMS era.], the RBAC analysis used the EuroQoL EQ-5D. Three measures were used to quantify the QoL benefits of PCI over CABG:
- pain/discomfort question on the EQ-5D recorded as a binary variable;
- weighted composite HRQL measure calculated from the EQ-5D responses;
- quality-adjusted life years post-intervention estimated from the HRQL measure.
The incremental risk was calculated as the difference in the proportion of patients experiencing additional revascularisation when assigned to PCI or to CABG. Incremental benefit was calculated as the difference in the proportion of patients reporting to be free from pain. The incremental risk/benefit ratio was obtained by dividing incremental risk by incremental benefit. A long time frame was chosen for the risks of PCI, whilst a shorter time frame was chosen for benefits, due to differences in benefit being concentrated in the first few months after initial revascularisation. ( Figure 6 ) In this way the choice of PCI over CABG is a model for accepting greater long-term risk of additional revascularisation in exchange for reduced post-procedural morbidity, specifically pain and composite HRQL.
The results of this analysis demonstrated that in order to be 95% confident that their decision in choosing PCI over CABG is risk-effective, a patient and their treating physician would need to be willing to accept that for each patient who benefits from PCI (i.e., by being pain-free at one month when they would still potentially be in pain had they chosen CABG), there are 1.06 PCI patients who experience over the next three years an additional revascularisation that would potentially have been avoided with CABG. ( Figure 7 )
Importantly, individual patients will value the trade-off differently: for some, exchanging the increased risk of repeat PCI or CABG to obtain short-term pain relief will be acceptable, whilst others may prefer to endure short-term pain to obtain a higher probability of avoiding a subsequent revascularisation. Patients may also prefer to risk undergoing multiple PCI procedures rather than a single CABG, or they may prefer to avoid the risk of requiring CABG subsequent to PCI and instead have CABG initially.
Use of freedom of pain, as a measure of benefit from revascularisation, provides a useful way for physicians to work with patients, as the presence or absence of pain is intuitive and more tangible for the patients compared with quantitative scores of QoL. In addition, the distribution of risk/benefit ratios provides patients and physicians with a sense of the trade-off between risks and benefits and not simply the separate magnitudes of risks and benefits. Arguably patients would be best informed by being given both the risk-benefit ratio and the size of the absolute risks and benefits.
This methodology can be applied to the subsequent trials: in particular, it may enable more informed decision-making on the part of patients and their physicians in choosing between PCI and CABG when neither procedure has a compelling indication or contraindication. The results of the SYNTAX trial explored in detail the different risks and benefits of PCI with DES compared with CABG: for example, the incremental risk of repeat revascularisation was reduced from 17.2% (ARTS-I) to 7.6% (SYNTAX), although differences in inclusion criteria preclude a direct comparison [4545. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. ].
SYNTAX TRIAL
The Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) trial was a large randomised trial that compared PCI with paclitaxel-eluting stents versus CABG among patients with three-vessel or left main coronary artery disease. At one year, the rate of the composite primary endpoint (death, myocardial infarction, stroke or repeat revascularisation) was lower with CABG than with PCI, due to a significant reduction in the need for repeat revascularisation [4545. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-72. ].
SF-36, SAQ and EQ-5D have been evaluated before and after the procedure, at one month, six months and at one year. From a preliminary risk-benefit analysis, both scores improved significantly at six and twelve months for both groups, without any statistical difference at six and twelve months. However, at one month patients who received PCI showed a greater improvement in all the scores analysed compared with those patients who received CABG. Conversely, at twelve months 76.3% of the CABG patients were angina-free compared to 71.6% of PCI patients (p=0.05) [4646. Cohen DJ, Van Hout B, Serruys PW, Mohr FW, Macaya C, den Heijer P, Vrakking MM, Wang K, Mahoney EM, Audi S, Leadley K, Dawkins KD, Kappetein AP. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011;364:1016-26.
Quality of life between PCI and CABG in DES era and left main disease.]. The trade-off methodology applied in the ARTS-I trial will potentially allow comparison of the one year quality of life with the three year outcomes of the SYNTAX trial once longer term follow-up is completed.
At 3-year follow-up, there were no differences in SAQ and SF-36 between PCI and CABG group. However, at 5-year follow-up, there were a small but statistically significant difference in favour of CABG vs. PCI, with lower frequency of angina physical limitation. [3838. Abdallah MS, Wang K, Magnuson EA, Osnabrugge RL, Kappetein AP, Morice MC, Mohr FA, Serruys PW, Cohen DJ. Quality of Life After Surgery or DES in Patients With 3-Vessel or Left Main Disease. J Am Coll Cardiol. 2017;69:2039–50. ]
EXCEL TRIAL
The Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularisation (EXCEL) trial was a prospective, randomised, non-inferiority trial that compared PCI with second generation everolimus-eluting stent versus CABG in patients with left main coronary disease and low or intermediate anatomical complexity. [4747. Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, Kandzari DE, Morice MC, Lembo N, Pagé P, Dressler O, Kosmidou I, Mehran R, Pocock SJ, Kappetein AP. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med. 2016;375:223–35. ] At 5-year, there were no differences in terms of primary composite endpoint of death, stroke, or myocardial infarction between PCI and CABG (22.0% vs 19.2%). [4848. G.W. Stone, A.P. Kappetein, J.F. Sabik, S.J. Pocock, M.-C. Morice JP, D.E. Kandzari, D. Karmpaliotis, W.M. Brown III, N.J. Lembo AB, B. Merkely, F. Horkay, P.W. Boonstra, A.J. van Boven, I. Ungi GB, S. Mansour, N. Noiseux, M. Sabaté, J. Pomar, M. Hickey AG, P.E. Buszman, A. Bochenek, E. Schampaert, P. Pagé, R. Modolo JG, C.A. Simonton, R. Mehran, I. Kosmidou, P. Généreux, A. Crowley OD, Serruys and PW. Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N Engl J Med. 2019;381:1820–30. ]
Quality of life data (SAQ, SF-12, EQ-5D, the Rose Dyspnea Scale and the Patient Health Questionnaire-8) were assessed at baseline, 1-month, 1 and 3-year. Whereas at 1-month, PCI was associated with a better quality of life than CABG, this difference was reduced at 1-year and disappeared at 3-year. [4949. Baron SJ, Chinnakondepalli K, Magnuson EA, Kandzari DE, Puskas JD, Ben-Yehuda O, Van Es G-A, Taggart DP, Morice M-C, Lembo NJ, III WMB, Banning A, Simonton CA, Kappetein P, Sabik JF, Serruys P, Stone GW, Cohen DJ. Quality-of-Life After Everolimus-Eluting Stents or Bypass Surgery for Left-Main Disease. J Am Coll Cardiol. 2017;70:3113–22. ] These data were in line with previous observations that benefits of PCI are usually concentrated early after revascularization as compared to CABG, with a progressive reduction of this benefit over time. ( Figure 8)
New methods in risk/benefit analysis
- Risk-benefit modelling can be used to demonstrate the trade-off that physicians and patients face in choosing between the deferred benefits of reduced rates of repeat revascularisation from CABG versus delayed relief from pain or improvement in HRQL
- This is important, from the patient’s perspective, in order to translate the risk and benefit deriving from different revascularisation procedures to something more tangible and easy to understand
- Risk-benefit acceptability curve (RBAC), analogous to the cost-effectiveness acceptability curves, provides estimates of the probability that a particular approach such as PCI is viewed by the patient as being risk-effective over different preference thresholds for the risk-benefit trade-offs identified
- In this way, the choice of PCI over CABG is a model of accepting greater long-term risk of additional revascularisation in exchange for reduced post-procedural morbidity, specifically pain and composite HRQL
Risk-benefit analysis for treatment of severe aortic stenosis
Aortic stenosis (AS) is the most common valvular heart disease. [5050. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–11. ] For decades, its treatment was surgical aortic valve replacement (SAVR) and very elderly and those patients at high surgical risk were denied to a definitive therapy for AS, with consequences in life prognosis and quality of life. [5151. Lung B, Cachier A, Baron G, Messika-Zeitoun D, Delahaye F, Tornos P, Gohlke-Bärwolf C, Boersma E, Ravaud P, Vahanian A. Decision-making in elderly patients with severe aortic stenosis: Why are so many denied surgery. Eur Heart J. 2005;26:2714–20. ]
In an effort to minimize the perioperative morbidity and mortality associated with SAVR, the less invasive transcatheter aortic valve replacement (TAVR) technique has been developed in order to offer an alternative treatment modality for patients who are not suitable or are considered at very high surgical risk for SAVR. The safety and efficacy of TAVR strategy was assessed primarily by a randomized clinical trial the "AoRTic TraNscathetER Valve Placement" (PARTNER) trial. [5252. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW,Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N Engl J Med. 2011;364:2187–98. , 5353. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S. Transcatheter Aortic-Valve Implantation for Aortic Stenosis in Patients Who Cannot Undergo Surgery. N Engl J Med. 2010;363:1597–607. ]
The PARTNER Trial demonstrated that TAVR is superior to medical treatment and non-inferior to SAVR in terms of mortality. [5252. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW,Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N Engl J Med. 2011;364:2187–98. , 5353. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S. Transcatheter Aortic-Valve Implantation for Aortic Stenosis in Patients Who Cannot Undergo Surgery. N Engl J Med. 2010;363:1597–607. ] For this reason, use of TAVR has become a globally accepted strategy for treating this group of patients. At the time of deciding either a surgical or a percutaneous approach, it is recommended to perform a risk-benefit analysis, considering advantages and disadvantages of each procedure with a patient-centered clinical decision making.
In terms of HRQL, KCCQ and the SF-12 were used in comparison between patients who underwent TAVR and those with standard medical treatment. Both scores showed significant differences in favor of the TAVR group. When comparing TAVR vs. SAVR these scores were better at 1 month in the TAVR vs. SAVR group, with no differences at 6 months and 1-year follow-up, suggesting a quick and early recovery with TAVR vs. SAVR. [5454. Reynolds MR, Magnuson EA, Lei Y, Leon MB, Smith CR, Svensson LG, Webb JG, Babaliaros VC, Bowers BS, Fearon WF, Herrmann HC, Kapadia S, Kodali SK, Makkar RR, Pichard AD, Cohen DJ. Health-Related Quality of Life After Transcatheter Aortic Valve Replacement in Inoperable Patients With Severe. Circulation. 2011;124:1964–72. , 5555. Thourani VH, Williams M, Zajarias A, Rihal CS, Brown DL, Smith CR, Leon MB, Cohen DJ, Ms C. Health-Related Quality of Life After Transcatheter or Surgical Aortic Valve Replacement in High-Risk Patients With Severe Aortic Stenosis ( Placement of AoRTic TraNscathetER Valve ) Trial ( Cohort A ). J Am Coll Cardiol. 2012;60:548–58. ]
Health status assessment at five-years comparing TAVR vs SAVR in high-risk patients shows similar results, with 61% of patients in the TAVR group and 65% in the SAVR group having a KCCQ score more than 60 (p=0.61).[5656. Arnold S V, Chinnakondepalli KM, Magnuson EA, Reardon MJ, Deeb GM, Gleason T, Yakubov SJ, Cohen DJ, Investigators CUSPT. Five-Year Health Status After Self-expanding Transcatheter or Surgical Aortic Valve Replacement in High-risk Patients With Severe Aortic Stenosis. JAMA Cardiol [Internet]. 2021 Jan 1;6:97–101. ]
In conclusion, TAVR approach in high risk patients provides comparable safety and efficacy vs. SAVR, with a earlier and quick improvement in QoL. Future studies are focused on quality of life data in low and intermediate risk patients. (Focus Box 4)
Risk/benefit analysis in AS treatment
- TAVR approach provides a safe and efficient treatment for patients who are not suitable or are consideredat very high surgical risk of for SAVR.
- QoL assessment is important in this specific population at the time of decision between SAVR and TAVR
- Health status assessment showed that patients who underwent a TAVR present an earlier improvement in QoL, with similar results at 6 months and 1 year compared with SAVR.
Conclusion
PCI and CABG have been compared in order to quantify the difference in terms of incidence of various cardiovascular events. From the patients’ perspective, the perception of quality of life is more meaningful compared to having a higher incidence of target lesion revascularisation. Comparison between PCI and CABG, in terms of risk-benefits derived from these revascularisation procedures, potentially allows physicians an evaluation of this perception from the patients’ perspective.
We have described how improvements in PCI technology have been translated into improvements in quality of life in PCI patients whilst simultaneously progressively reducing the gap between PCI and CABG in terms of efficacy. In addition, as the benefits from PCI come predominantly in the first months after the procedure compared with those from CABG, a new risk-benefit model has recently been developed to allow comparison of long-term follow-up against short-term benefit. Consequently, physicians may potentially use the risk-benefit data to give patients a more balanced perspective when faced with a choice between PCI and CABG.
Personal perspective - Sally C. Stearns
The comparative effectiveness and cost-effectiveness of alternative treatments for ischaemic heart disease are important criteria in determining the optimal revascularisation modality. In choosing between treatments, patients may wish to weigh more explicitly short versus long-term trade-offs between a more rapid return to normal health with PCI versus the reduced need for future interventions with CABG. Risk-benefit models offer a platform for making such comparisons more explicit.








_thb.jpg)